Translate this page into:
Deep vein thrombosis and acute renal insufficiency after in vitro fertilization in a medically complicated patient
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The unique case of a young woman with a history of ulcerative colitis and multiple laparotomies is described. She was admitted after oocyte recovery with bilateral lower limb deep vein thrombosis and acute renal insufficiency without convincing evidence of severe ovarian hyperstimulation. This case presented significant diagnostic and therapeutic challenges.
It is not possible to quantify the risk of serious complications after in vitro fertilization (IVF) for women with a known medical history. However, it is expected to be above average for at least some of them. Furthermore, management of the arising complications can be problematic in this group. It is recommended that specific measures be taken when these individuals undergo IVF in order to minimize the risk of adverse events.
Keywords
IVF
ovarian hyperstimulation syndrome (OHSS)
renal failure
thrombosis
ulcerative colitis
INTRODUCTION
Advancement in clinical medicine has led to the improvement of long-term health and quality of life of young women with chronic medical conditions. As a result, many of them pursue pregnancy and should this not occur naturally, seek treatment in the form of assisted conception, in particular, in vitro fertilization (IVF).[1]
It is likely that depending on their medical history, some women are at a higher risk of developing complications after IVF treatment.[2] Should a complication arise, further management may also turn out to be more challenging than usual.
The unique case of a woman with a complicated medical and surgical history, who underwent controlled ovarian stimulation for IVF, is hereby presented. She was admitted after oocyte collection with severe abdominal pain and subsequently, developed two serious medical complications. The diagnostic and therapeutic challenges of this case are described. Recommendations are also made for minimizing the risk(s) in the medically complicated patient(s) undergoing IVF treatment.
CASE REPORT
A 30-year-old Caucasian female and her partner were referred to the assisted reproduction unit with a 4-year history of primary infertility. She had been diagnosed with ulcerative colitis at the age of 15 years and since then underwent various appropriate medical treatments. She had used the combined oral contraceptive pill without any reported side effects. She had not been on medication for the last 3 years except for a daily dose of periconceptional folic acid.
Her medical history also included a single episode of drug-induced acute pancreatitis and a road accident that resulted in the development of a rectovaginal fistula. Her surgical history included a series of three midline laparotomies (colectomy with ileostomy and rectal pouch preservation, excision of a posttraumatic rectovaginal fistula with removal of the rectal pouch, and adhesiolysis for incomplete bowel obstruction). Within the colectomy specimen, a small Dukes A adenocarcinoma was diagnosed that prompted subsequent removal of the remaining rectum.
She had been seen for prepregnancy counseling prior to embarking on the above surgery. At the time, planned surgery was expected to take place mainly in the abdominal area rather than the pelvic area and hence, no significant negative impact on future fertility was anticipated.
At the time of presentation for fertility treatment, she was an ex-smoker with a normal body mass index. Her menstrual cycle was always regular and ovulation had recently been confirmed by progesterone testing. The partner's semen analysis was normal. Based on the couple's long-standing infertility and her history of pelvic surgery, IVF treatment was advised. Her pretreatment assessment included a transvaginal ultrasonography, which revealed normal ovarian appearances with a normal antral follicle count and a left ovary that was situated high in the pelvis. Her follicle-stimulating hormone (FSH) level was also within the normal limits and she was predicted to be a normal responder. She was counseled about the risks of undergoing IVF treatment, with particular emphasis on the risk of complications at the time of and after oocyte recovery due to her previous laparotomies. An antagonist stimulation protocol [225 International Units (IU) of recombinant FSH starting dose] after a progesterone priming period was advised as per the local protocol. The patient was reluctant to use oral hormonal medication due to the concern that it may cause gastrointestinal upset; she was then prescribed a 21-day long gonadotropin-releasing hormone (GnRH) agonist protocol (same starting dose of FSH).
Her ovarian stimulation was uneventful and no dosage adjustment was required. Oocyte recovery was performed under conscious sedation, with fentanyl being used intravenously for pain relief. The patient experienced more than average discomfort during the procedure. Nevertheless, both her ovaries were easy to access and oocyte collection was completed uneventfully. A total of eleven oocytes were obtained. Intraoperative antibiotic cover (intravenous administration amoxicillin/clavulanic acid 1.2 gr bolus) was used as per protocol. A 1-week course of an oral antibiotic (amoxicillin/clavulanic acid 625 mg three times daily) was prescribed postoperatively, as this was deemed a high-risk case for pelvic infection after oocyte collection. Through conventional IVF, eleven oocytes were normally fertilized.
The patient presented to the accident and emergency department approximately 48 h after the oocyte recovery with complaints of severe left iliac fossa pain radiating to the back and associated nausea and vomiting. Her ileostomy was still functional, even though bowel movements were reported to be slower than usual. She was apyrexial and her blood pressure was within normal limits. On examination, she was found to be mildly tachycardiac but not tachypneic. The abdomen was soft but exhibited deep tenderness, mainly on the left iliac fossa region. The rest of the physical examinations were unremarkable. A blood panel revealed normal hemoglobin and hematocrit, elevated white cell count, and creatinine levels at the high-end of the normal spectrum (93 umol/L). Diagnosis of the ovarian hyperstimulation syndrome (OHSS) was considered, although injury to pelvic structures, the bowel in particular, could not be excluded. She was admitted for conservative management and was started on intravenous antibiotics and fluids. Low-molecular-weight heparin (LMWH) was prescribed for thromboprophylaxis and elastic leg stockings were used.
After mild symptomatic improvement during the first 24 h, the abdominal pain and tenderness increased, even though they remained localized. Despite a good urine output, her renal function deteriorated. An abdominal and pelvic computed tomography (CT) scan was requested. In preparation for the scan an intravenous fluid bolus was administered as per protocol, taking into account the reduced renal clearance. The CT scan reported a moderate amount of free peritoneal fluid, large ovaries with areas of hemorrhagic cystic follicles, and a mild unilateral pleural effusion. No localized area suggestive of bowel perforation was visualized. As the CT result was suggestive of ovarian hyperstimulation, conservative management was continued. In view of the patient's clinical condition, ten embryos that resulted from the IVF treatment were cryopreserved for future use.
On the third day, the patient felt unwell and her vital signs suddenly deteriorated; her blood pressure dropped from 103/70 mmHg to 85/56 mmHg, pulse increased from 93 bpm to 110 bpm, and oxygen saturation decreased from 98% to 93% on air. She responded well to oxygen and intravenous fluid administration. Renal function continued to deteriorate (creatinine 286 umol/L) and serum inflammatory markers increased. The possibility of sepsis was reconsidered and an alternative antibiotic regimen was prescribed (piperacillin sodium/tazobactam sodium IV- the dose titrated according to renal function). In the evening of the same day, the patient developed bilateral lower limb edema. Duplex ultrasonography revealed bilateral deep vein thrombosis. In view of the renal insufficiency, a therapeutic heparin infusion was started, titrated against the changing glomerular filtration rate.
During the following day, her creatinine levels reached a peak concentration of 372 umol/L. Emergency hemodialysis was considered; however, conservative management was agreed upon. On the fifth day, the inflammatory markers and renal function started to improve. By the eighth day, her creatinine levels became normal and warfarin was introduced and titrated according to international normalized ratio (INR). Her blood and urine cultures came back negative and immunology screen was positive for antineutrophil cytoplasmic antibodies (ANCAs). She was discharged with follow-up appointments with the IVF, hematology, nephrology, and rheumatology departments.
A summary of this patient's admission is displayed on Table 1.

DISCUSSION
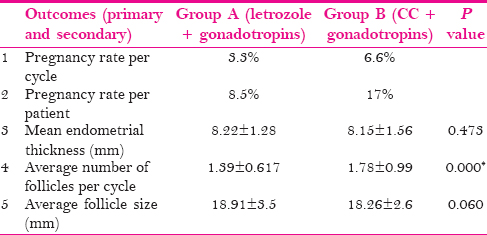
This unique clinical case describes the concurrent development of two serious and potentially life-threatening complications, namely, deep vein thrombosis and acute renal failure in a young woman who underwent controlled ovarian stimulation during IVF treatment. Thromboembolic or urological complication after IVF have been previously described but never on the same individual [Table 2].
The primary cause leading to the aforementioned complications was not confirmed; however, OHSS was considered to be the main suspect. OHSS, in its most severe form, is known to predispose to venous and arterial thromboses as well as acute renal insufficiency.[13,14] Although the exact pathophysiological mechanisms are unclear, significant plasma volume depletion, extravasation, fluid shift to the "third space," and associated hemoconcentration are thought to be the important contributors.[15] Interestingly, in the described case, neither profound hemoconcentration, measured by serial hematocrit levels, nor significant fluid shift, as evident from the only moderate peritoneal fluid collection at the time of CT scan, were ever detected. It is worth noting that in view of the reduced renal clearance, the peritoneal fluid collection could also have been exacerbated by the intravenous fluid challenge in preparation for the CT scan. Based on these findings, this case would be classified as a moderate OHSS case.[16] One could argue that ascites may not be clearly visible with imaging in the case of a woman with previous laparotomies. Likewise, enthusiastic fluid replacement may mask hemoconcentration. However, the albumin levels would have eventually decreased had significant extravasation taken place.[16] It is possible that even less than severe OHSS can lead to substantial changes in the coagulation/fibrinolytic pathway and systemic microcirculation, thus increasing the risk for complications such as thrombosis and renal insufficiency without necessarily mediating plasma volume depletion.[17] An alternative explanation entails the existence of a background patient predisposition to these complications, which manifested when she was exposed to the biological effects of controlled ovarian stimulation. In the discussed case, confirmed deep vein thrombosis and possible pulmonary embolism, accounting for the blood pressure and oxygen saturation drop on the third day, occurred despite the use of prophylactic LMWH. This observation makes an even stronger argument for the existence of a background condition.[18] Such a possibility was explored by requesting a full immunological screen in this particular patient, which included anticardiolipin antibody testing. Only ANCA seropositivity was observed. ANCA seropositivity is found more frequently with inflammatory bowel disease.[19] In the rheumatology field, a group of ANCA-positive vasculitis-related disorders has been medically defined and described.[20] Individuals who have been diagnosed with ANCA-positive vasculitis are more likely to experience venous and arterial thromboses, especially during exacerbation of the disease.[21] They may also be predisposed to renal disease or even acute renal failure.[22] The significance of our patient's ANCA positivity is uncertain. However, it may be that the combination of a less than severe form of OHSS with ANCA positivity achieved the threshold for developing such life-threatening complications.
Sepsis, with or without the associated bowel injury, after oocyte collection was also considered to be a contributor to thrombosis and renal insufficiency. Clinical and laboratory improvements were achieved after switching to a second-line antibiotic. However, the improvement could also be attributed to spontaneous resolution of the condition or to the timely administration of a therapeutic heparin infusion. Lack of fever is not common with sepsis. In our case, temperature elevation could have been masked by the regular administration of paracetamol, 1 gr orally every 6 h for the first 4 days after admission followed by administration on demand. C-reactive protein levels are also raised during and shortly after routine ovarian stimulation or with OHSS and are, therefore, less helpful in exploring the diagnosis of sepsis in this particular group of women.[23]
Other potential contributors to acute renal failure include the medication used during IVF and the contrast medium for CT imaging. However, none of the medications used in IVF are strongly linked to renal insufficiency.[24] Furthermore, the administration of contrast medium does not explain the original renal insult. At the time of presentation, renal function was likely already compromised, as evident from the high-normal serum creatinine levels in the absence of significant hemoconcentration. Postrenal causes were considered but excluded since urine output was always satisfactory and there was no evidence of urinary tract obstruction on the CT scan. Finally, none of the above scenarios accounts for the concurrent development of venous thromboembolism.
Advancement in medical technology and pharmaceutics has encouraged a significant number of women with chronic medical issues to pursue pregnancy. Women with a history of inflammatory bowel disease constitute a high-risk treatment group, not merely because of their systemic condition but also due to extensive abdominal surgery. Although it is unclear whether the original bowel disorder is a causative factor of infertility, it is accepted that relevant pelvic surgery may often lead to subfertility and the need for assisted conception treatments.[25]
When IVF treatment is considered for these women, there may be medical risks even if the original condition has apparently been treated. In this case, ulcerative colitis was cured by total surgical removal of the colon and the patient had been presumed to be fit. Suffering two serious complications at the same time could be attributed to chance or an exaggerated reaction to the effects of ovarian stimulation.
Previous extensive abdominal and pelvic surgery is thought to increase the risk of intraoperative complications during oocyte collection, even though no hard evidence is currently available. As this case highlights, the medical staff are presented with complex diagnostic dilemmas when such a patient is referred with severe abdominal pain after IVF. Emergency surgery to repair a bowel injury can be life-saving but may also cause harm on grounds of a medical diagnosis, such as OHSS. The risk of intraoperative complications is also notably higher in the presence of previous extensive surgery, mainly due to adhesion formation.[26]
When IVF is planned, it seems entirely appropriate to be cautious with the stimulation regime in this high-risk group in an attempt to minimize the potential side effects. An antagonist regime has been shown to protect against severe OHSS compared to the standard long protocol and may be preferable, even without evidence of the predicted high response at preassessment.[27] Additional risk-reducing measures, such as opting for a GnRH agonist instead of a human chorionic gonadotropin "trigger" followed by cryopreservation of any resulting embryos at the cleavage stage, may further reduce the risk of hyperstimulation and should, therefore, be considered.[28]
Prepregnancy counseling is also indicated for such high-risk cases. Ideally, it should be done before contemplating extensive pelvic surgery so as to allow the option of fertility preservation through oocyte or embryo freezing. This is a viable option since a significant proportion of these women will be rendered subfertile after surgery.[1,25] Oocyte retrieval before surgery carries no more than the background risk of intraoperative complications. Furthermore, having IVF at a younger age may be advantageous when the quality of the oocyte and the embryo is considered. Cryopreservation techniques of the embryo and the oocyte have significantly improved over the last decade and cumulative clinical pregnancy rates over 50% after frozen embryo transfers have been achieved.[29] Informed consent should always be practiced before fertility preservation, since IVF still carries a small but not negligible risk of complications.
Further research is required to quantify the absolute risk of complications in women with a preexisting medical or surgical condition who undergo assisted conception treatments. Improved knowledge will lead to better understanding of complex cases and thus, assist clinicians to better address suitability for IVF. In addition, it will assist women in making informed choices about their reproductive future.
Authors' roles
Dr. A. Papathanasiou drafted and revised the manuscript, including the critical discussion. Dr T. Kalampokas participated in the process of drafting and revising the manuscript. Dr A. Maheshwari suggested the case report and participated in the task of revising of the manuscript.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
Dr A. Papathanasiou would like to acknowledge Ms Valerie Peddie for her useful and constructive input.
REFERENCES
- Female fertility and childbirth after ileal pouch-anal anastomosis for ulcerative colitis. Br J Surg. 2007;94:478-82.
- [Google Scholar]
- Ovarian stimulation for ovulation induction and in vitro fertilization in patients with systemic lupus erythematosus and antiphospholipid syndrome. Fertil Steril. 2009;92:1803-10.
- [Google Scholar]
- Venous thromboembolism in relation to in vitro fertilization: An approach to determining the incidence and increase in risk in successful cycles. Fertil Steril. 2012;97:95-100.
- [Google Scholar]
- Incidence of pulmonary and venous thromboembolism in pregnancies after in vitro fertilisation: Cross sectional study. BMJ. 2013;15(346):e8632.
- [Google Scholar]
- Nephrotic Syndrome Developing in Severe Ovarian Hyperstimulation Syndrome: Report of Two Cases. Human Reproduction Conference: 28 th Annual Meeting of the European Society of Human Reproduction and Embryology. In: ESHRE 2012. Istanbul, Turkey: ESHRE; 2012. p. :27.
- [Google Scholar]
- Acute prerenal failure and liver dysfunction in a patient with severe ovarian hyperstimulation syndrome. Hum Reprod. 1990;5:348-51.
- [Google Scholar]
- Acute decline in renal function as a consequence of ovarian hyperstimulation syndrome. Nephron. 1992;60:104-7.
- [Google Scholar]
- Ureteral injury after transvaginal ultrasound-guided oocyte retrieval: A complication of in vitro fertilization-embryo transfer that may lurk undetected in women presenting with severe ovarian hyperstimulation syndrome. Fertil Steril. 2011;96:869-71.
- [Google Scholar]
- Renal artery dissection during an in vitro fertilization/intracytoplasmic sperm injection cycle. Fertil Steril. 2009;92:1498.e1-3.
- [Google Scholar]
- Hydronephrosis in a woman undergoing in vitro fertilization. Urology. 2007;69:384.e19-20.
- [Google Scholar]
- Ovarian hyperstimulation syndrome and its effect on renal function in a renal transplant patient undergoing IVF treatment: Case report. Hum Reprod. 2000;15:1275-7.
- [Google Scholar]
- The "ART" of thromboembolism: A review of assisted reproductive technology and thromboembolic complications. Thromb Res. 2008;121:713-26.
- [Google Scholar]
- Diagnosis, prevention and management of ovarian hyperstimulation syndrome. Br J Obstet Gynaecol. 1995;102:767-72.
- [Google Scholar]
- Increased capillary permeability induced by human follicular fluid: A hypothesis for an ovarian origin of the hyperstimulation syndrome. Fertil Steril. 1995;63:268-72.
- [Google Scholar]
- Review of the evidence base of strategies to prevent ovarian hyperstimulation syndrome. Hum Fertil (Camb). 2007;10:75-85.
- [Google Scholar]
- Subclavian deep vein thrombosis associated with the use of recombinant follicle-stimulating hormone (Gonal-F) complicating mild ovarian hyperstimulation syndrome. Fertil Steril. 2000;73:1253-6.
- [Google Scholar]
- Internal jugular vein thrombosis following mild ovarian hyperstimulation syndrome in women with factor V Leiden mutation. Am J Med Sci. 2006;332:131-3.
- [Google Scholar]
- Anti-neutrophil cytoplasmic antibodies (ANCA) specific for one or several antigens: Useful markers for subtypes of ulcerative colitis and associated primary sclerosing cholangitis. Clin Chem Lab Med. 2012;50:503-9.
- [Google Scholar]
- Venous thromboembolism in ANCA-associated vasculitis--incidence and risk factors. Rheumatology (Oxford). 2008;47:530-4.
- [Google Scholar]
- Renal involvement in anti-neutrophil cytoplasmic autoantibody associated vasculitis. Autoimmun Rev. 2013;12:477-82.
- [Google Scholar]
- Elevated levels of CRP in ovarian hyperstimulation syndrome: An unrecognised potential hazard? BJOG. 2005;112:952-5.
- [Google Scholar]
- British National Formulary (BNF) (65 th). London: Pharmaceutical Press; 2013.
- Female infertility after ileal pouch-anal anastomosis for ulcerative colitis. Dis Colon Rectum. 2004;47:1119-26.
- [Google Scholar]
- Peritoneal adhesions: Pathogenesis, assessment and effects. Trop Gastroenterol. 2006;27:11-8.
- [Google Scholar]
- Gonadotrophin-releasing hormone antagonists for assisted reproductive technology. Cochrane Database Syst Rev 2011:CD001750.
- [Google Scholar]
- Gonadotropin-releasing hormone agonist versus HCG for oocyte triggering in antagonist assisted reproductive technology cycles. Cochrane Database Syst Rev 2011:CD008046.
- [Google Scholar]
- Clinical efficiency of oocyte and embryo cryopreservation. Ann NY Acad Sci. 2008;1127:49-58.
- [Google Scholar]







