Translate this page into:
Demography, expectations and experiences of oocyte donors in northern India − an interview-based study
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Study question:
Oocyte donation is an increasingly popular treatment option for pregnancy and parenthood in women with poor ovarian reserve or advanced age. Indian literature still lacks a formal study focusing on expectations and experiences of oocyte donors.
Aim:
To assess demography, expectations and experiences of oocyte donors in northern India by an interview-based questionnaire.
Material and Methods:
This is a prospective cross-sectional study at a tertiary care IVF centre from August 2018 to January 2019. Sample size was 65 oocyte donors found fit and willing for egg donation. Interviews were taken using structured questionnaire at the time of registration and after successful oocyte retrieval.
Results:
Mean age of donors was 25 years. Most of the donors were housewives (70%) and rest were in a private job. Only 29% of donors were educated above tenth standard. Almost all the donors (96%) were commercial donors introduced by paid agents or friends. Most of the donors had very poor understanding of details of the oocyte retrieval procedure. Only 36% of donors felt that compensation given is adequate, rest expected a higher compensation. Average compensation given to donors was INR 15,000–25,000, which was 5000–10,000 less than their expectations. All donors were satisfied with the procedure and did not feel exploited or anxious or depressed but few complained of discomfort experienced in visits and minimal complications like pain, nausea, and fever. None of the donors developed signs/symptoms of OHSS. Average number of oocytes retrieved per donor was 17. Mean dose of gonadotropins required per donor was 1495 IU.
Conclusion:
Our findings show that the oocyte donation has an overall good acceptance and satisfaction among the donors. However there is a need to impart more detailed information to donors in order to prevent their possible exploitation.
Keywords
Egg donors
infertility
oocyte donation
INTRODUCTION
It is estimated that approximately 22–23 million couples in India experience infertility and the total fertility rate has declined from 3.9 in 1990s to 2.3 in 2013.[1] Oocyte donation is an established treatment in women with premature ovarian failure, gonadal dysgenesis and in carriers of recessive autosomal disorders.[2]
There is exponential increase in egg donation cycles in the last few years, in India as well as abroad. There are no official statistics available on the number of egg donation cycles carried out in India. However, according to the National Assisted Reproductive Technology (ART) Registry of India, in 2006, 12% of total IVF cycles were egg donation cycles and between 2007 and 2009 the number of anonymous egg donation cycles doubled, from 1047 to 2130.[3,4] In Europe and USA, egg donation cycles formed 4% and 12% of total IVF cycles respectively in year 2016.[5] However there is no latest data in Indian literature as to what proportion of total IVF cycles form oocyte donation cycles.
Oocyte donation is mainly commercial in India.[6,7] Nearly 20% of Indians live below poverty line.[8] This could lead to a ready availability of willing commercial egg donors. Since no regulation exists yet that can safeguard the interest of this growing cohort of vulnerable individuals in ART treatment, there exists no mechanism to keep a check on complete and full compensation to these donors. They could be exposed to exploitation at various levels.
Since the scenario in India is different from other countries socioeconomically, there is a need to study the demographic details, expectations and experiences of donors. Assessment of these is expected to play a crucial role in safeguarding their interest which will encourage them for donations. Results of this study will also help policy makers and recruitment campaigns in making policies for betterment of physical and mental health of oocyte donors and to prevent their exploitation.
AIM AND OBJECTIVES
The aim of this article is to assess demography, motivation, expectations and experiences of oocyte donors in northern India by an interview-based questionnaire. The objectives are as follows:
to assess the demographic characteristics of oocyte donors enrolled in third-party ART cycles;
to determine motivation, knowledge and expectations from the procedure;
to determine post procedural experiences as determined by post procedural complications, satisfaction with compensation and psychological impact of the act of oocyte donation.
METHODOLOGY
This was a prospective cross-sectional survey carried out at a tertiary care IVF centre which is a large IVF centre of northern India where around 1200 IVF cycles are carried out per year. The study was conducted from August 2018 to January 2019. The sample size calculation was based on the data that 90–100 IVF cycles are carried out at the centre of study in a month, out of which nearly 10% are donor cycles. As our study duration was 6 months, we could recruit 65 oocyte donors in our study.
We came across 137 women who were willing for oocyte donation during our study period of 6 months. However, 72 women were found not fit for oocyte donation due to variable reasons like low AMH, positive viral markers, anaemia, etc. These women were hence excluded from our study, giving us our sample size of 65 oocyte donors who were fit for donation. All of these 65 women gave consent to participate in the study. These 65 donors were interviewed via structured questionnaire after registration but cycles got cancelled in seven of these donors due to poor follicular development. Hence information about experiences was collected from 58 donors after oocyte retrieval. A follow-up interview by telephonic call was also done after one week of oocyte retrieval for emergence of any new complication. Consort diagram is shown in Figure 1.

- Consort diagram of cases included in study
RESULTS
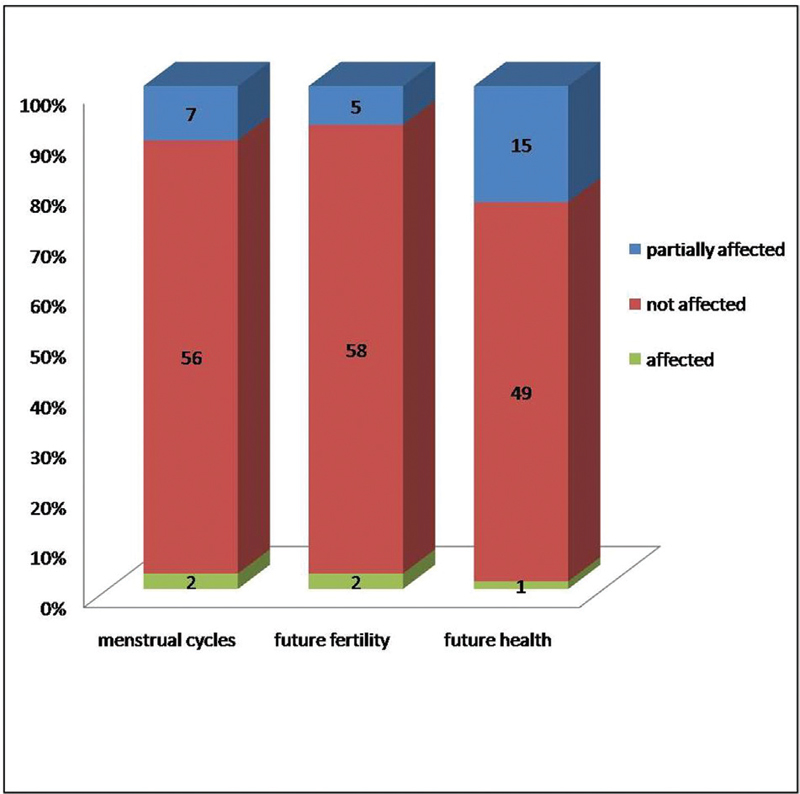
Our study includes data obtained from structured questionnaire of interview of 65 oocyte donors recruited in our study. Various demographic and physical characteristics of the donors are shown in Table 1. Donors were young adult females with mean age of 25 years. All of them were married with only four being divorced/widow. All donors had regular menstrual cycles. All had more than one living children. Most of our donors were housewives and 27% were working among whom mostly were in a salaried job. Most of the donors were from medium lower middle class income group; with average household income of 15,600. Most of the donors lived in rented accommodation. Donors were from all religious groups with distribution matching general population. Among Hindu donors majority (65.5%) were Dalits (lower social class).
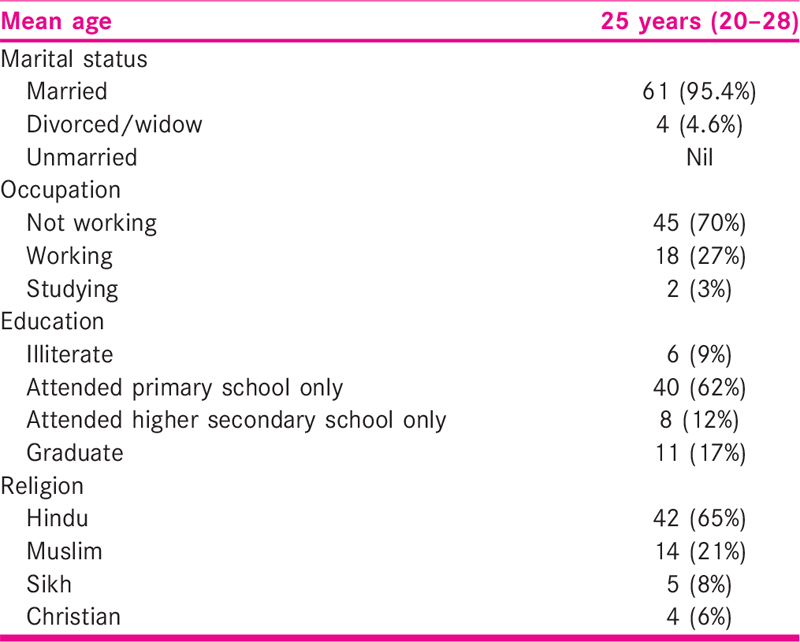
Most (63%) of our donors were introduced to the clinic by family or friends who had donated before. Twenty two donors were introduced directly by the recruiting agents. Only two donors got to know about the procedure through media. When asked whether the donation recruitment has been told to husbands, most (56) of the donors said that their husbands know about the donation, but this was hidden from the husband in five donors. Rest four donors were either widow or divorcee and their family knew about the donation. Although most (94%) of the donors were literate in our study, only few (17%) completed education till graduation, as shown in Table 1.
Studying the type of donors, we found that great majority (96%) were commercial donors with sole financial motives for the donation. Only two donors who claimed there are doing it for helping others apart from financial motive. Type of donors and number of previous donations is shown in Table 2.
In our study, donation cycles got cancelled in seven donors due to poor follicle development and hence were not rewarded any compensation amount. Various aspects of study like experiences and compensation were hence not obtained from these donors, were studied in rest 58 donors. Out of these 58 donors, 37 donors thought compensation was not adequate and 21 thought it was adequate. Amount of compensation amount received by the donors varied from minimum 15,000 to maximum 25,000 with average being 22,446. This variation was alleged to be due to many times there were multiple agents involved with the single donor, taking their share from the donor’s compensation.
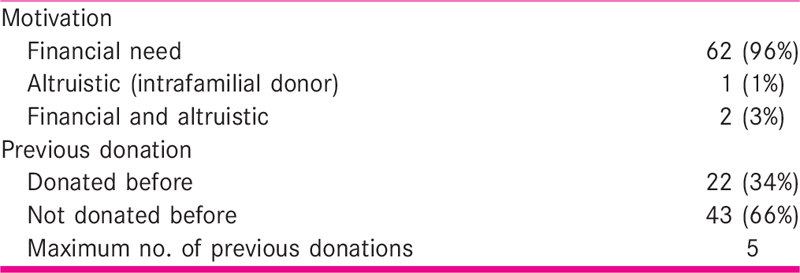
We studied perceptions of the oocyte donors about whether they knew about use of injectables, use of anesthesia and risks involved in the procedure. Almost all donors (62/65) knew about use of injectables for the procedure, that is 95.38%. Majority (50/65) of donors knew duration of injectables use is more than 9 days, that is 80.64%. Many (49/65) knew about use of anesthesia, that is 75.38%. Surprisingly 24.61% of our donors did not know about use of anesthesia. Only 12/65 (18.46%) of donors knew about the complications associated with the procedure, rest 53/65 (81.54%) had no idea about any complications. As shown in Figure 2.
- Perceptions of donors about use of injectables, anaesthesia and risks.
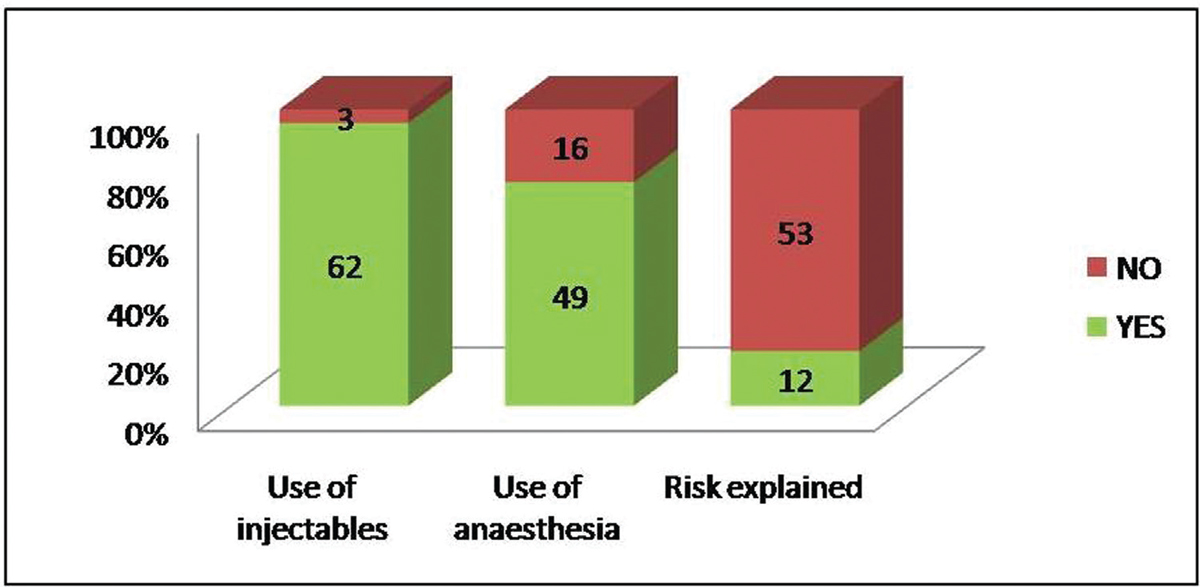
We also studied the perceptions of the donors about whether the procedure of oocyte donation affects menstrual cycles, future fertility and future health. Results were recorded as affected, not affected and partially affected. Most of the donors thought that oocyte donation does not affect the menstrual cycles (56/65), future fertility (58/65) and future health (49/65). These findings are shown in Figure 3.
- Perceptions of donors about menstrual cycles, future fertility and health.
Willingness of donors to declare their identity, to know about success of pregnancy and willingness to meet the child so born was also studied. Willingness about declaration of identity was found to be less common among our donors, only 29.2%, that is 19 donors, were willing to declare their identity. Nearly half of the donors, that is 36 donors (55.4%), were eager to know whether pregnancy has occurred or not from the oocyte donation. Those eager to know about pregnancy said this would make them feel good. Most (89.3%) of the donors (58/65) did not intend to think about or meet the child so born, because they feared it will break anonymity.
In seven out of sixty five donors (7/65), cycles were cancelled due to poor follicular development. This had severe implication on the donors, disheartening them emotionally and depriving them of compensation. No compensation was received upon cancellation even if injections for some days had been received. These seven were excluded from the data obtained regarding experiences of the donors on various aspects. Among the remaining 58 donors, 42 donors did not understand how to take the injections, 12 donors did not understand the need to take it timely and all 58 donors experienced mild abdominal pain after taking injections. Average amount of gonadotropins used for oocyte retrieval in these 58 donors was 1495 IU with minimum being 650 IU and maximum being 3875 IU. Among these 58 donors, average number of oocyte retrieved were 17.5 with minimum being 6 and maximum being 39.
When asked about the complications of oocyte retrieval procedure, 14 donors complained of abdominal pain, 4 had nausea, 1 had fever and rest 39 had no complications. Only one donor had extreme pain and nausea which required giving injectables medicines. None of the donors required admission for management of complications or need of blood transfusion.
When asked about how did the procedure affected donor’s life, significant disturbance in life was observed by 14/58 (24%) donors, no disturbance in life in 44/58 (76%) of donors. This is depicted in Figure 4.
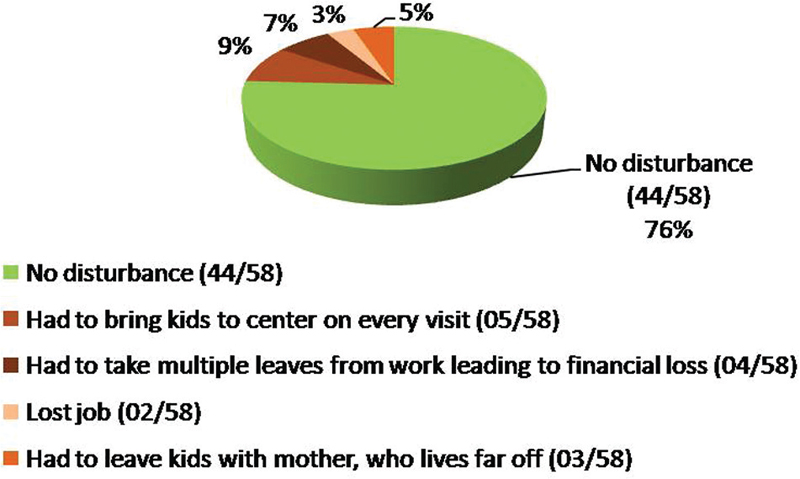
- Disturbances in lives of oocyte donors.
None of the donor felt exploited after the procedure and all were over all satisfied with the entire process. Only 4/58 donors admitted that they would have donated even if the family income was good, rest said they would not have donated. When asked how will the compensation money be used, donors had varied plans including using money for children, repaying debts, marriage in family, paying for room rent, etc. (as shown in Figure 5). Only seven among these 58 donors also expressed willingness to be surrogates, when asked.
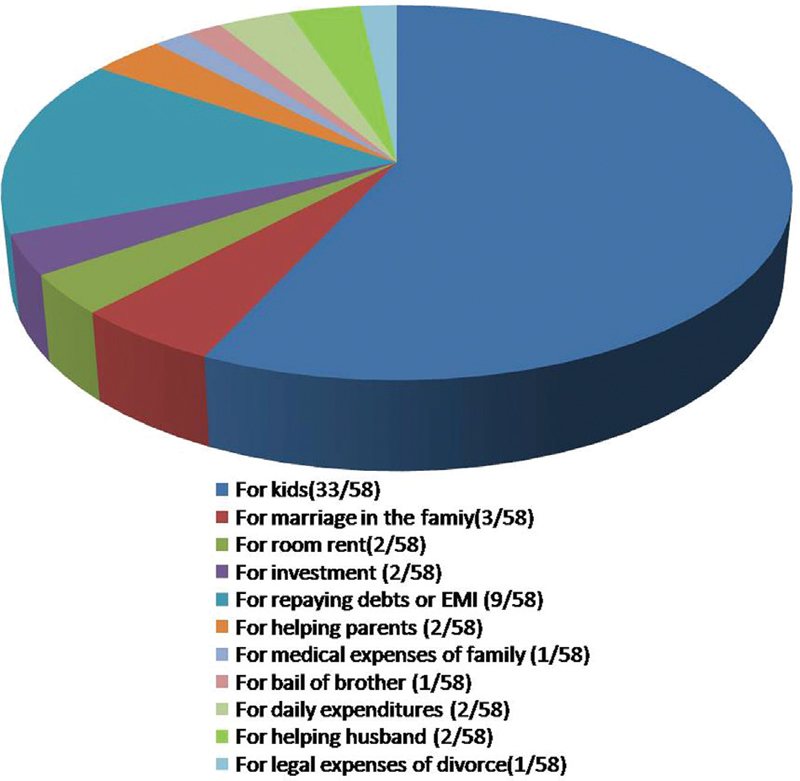
- Use of compensation money by donors.
When asked about the overall experience, all the donors were thankful and stated their satisfaction with procedure. Majority of donors, that is 53/58, admitted that they will recommend the procedure to others and also would like to donate again.
DISCUSSION
Present study was carried out in a large tertiary care IVF centre of northern India. This centre caters to population from Delhi, Jammu and Kashmir, Uttar Pradesh, Punjab and Haryana and similarly donors too come from nearby areas and represent large population from north India.
Our study is based on an in-depth personal interview of oocyte donors based on structured questionnaire. This methodology was chosen to encourage donors for coming up with easy and comfortable responses. Response rate in our study was hence 100% as opposed to 45% in Klock et al.[9] study and 49% in Kramer et al. study.[12] Purewal et al.[11] carried out a systematic review of oocyte donation which included 64 studies. Most (43/64) of the studies included were either from USA or UK. Hence results can be extrapolated mainly for western population. As India has different culture, heritage, religious beliefs and socioeconomic status, there was a need for a study in Indian context.
It was found in our study that all oocyte donors were married. 70% of our donor population were housewives, 27% were working and 3% were students and 9% were illiterate. In a study done by Jadva et al.[6] on 25 oocyte donors, 12% of their donor population was unmarried and 72% were working and none were illiterate. In our population 34% were repeat donors with maximum number of previous donations being five whereas 88% were repeat donors and maximum number of previous donations were seven in study done by Jadva et al. This difference in repeat donation could be the result of the changed time frame in which the studies were performed and the appearance of new guidelines on egg donation in 2017 limiting the number of egg donation to one. The difference in other demographic characteristics could be due to different populations catered by different fertility clinics.
Majority of donors, 96% in our study had financial motivation, only 1% had altruistic and 3% had both altruistic and financial motivation. In study done by Klock et al. in 2003, 40% of donors had donated for financial motive. In 2014, Pennings et al.[10] carried out a study in which motivation was pure altruism in 47.8%, altruism and financial in 33.9%, 10.8% pure financial, 5.9% altruism and own fertility and 2% own treatment only. In a study done by Jadva et al., the most common primary motivation given by 18 (72%) egg donors was financial need, with only one egg donor saying that she wished to help a childless couple. In a study done by Arora et al., 95% had financial motivation and 5% had altruistic motive. Reason for large financial motivation group in Indian studies could be existence of huge socioeconomic disparity. Another point of consideration here is many women in India do multiple donations to supplement their income leaving themselves in poor health, so clinics should discourage them to do multiple donations.
Most (63%) of our donors were introduced to the clinic by family or friends who had donated before. Twenty two donors were introduced directly by the recruiting agents. Only two donors got to know about the procedure through media. In a study done by Jadva et al., the majority (21, 84%) of egg donors had first heard about egg donation from family members, friends, neighbours or agents. We believe use of media in popularizing oocyte donation is underutilized. There is a need to make general public aware about oocyte donation through mass media. This will invite donors from all sections of society.
In a study done by Maxwell et al. in 2008,[13] serious complications occurred in 0.7% of cycles and minor in 8.5%. In our study, minor complications like pain abdomen, nausea were observed in 33% of donors, none of the donors experienced severe complications. Our observations reassure us that the risk involved in oocyte donation is relatively low but also emphasize that even when all care is taken complications do occur. Also, donors are not completely aware of possible complications. Here we can infer that there are loopholes in current practice of pre-donation counselling. More emphasis should be given on providing information about the complications and effect of procedure on the donors. This would help them to undergo the procedure more easily and without any stress.
In our study, willingness about declaration of identity was found to be less common, only 29.2% but 55.4% were eager to know about pregnancy. Those willing to know about pregnancy said this would make them feel good. However, most (89.3%) of the donors did not intend to think about or meet the child so born, because they feared it will break anonymity.
In 7 out of 65 donors (07/65), cycles were cancelled due to poor follicular development. This had severe implication on the donors, disheartening them emotionally and depriving them of compensation. Hence, we believe there is greater need of more meaningful counseling of donors explaining the possibility of failure of donation and this does not mean that there is something wrong with their own fertility.
In our study, 24% donors experienced difficulty in daily life during the oocyte donation cycle like carrying their kids daily to centre for long hours, bearing travel expenses, taking multiple leaves from work, losing job, etc. This shows that all donors have different challenges in life and fertility clinics should be sensitive and try to make injection and investigation schedule flexible according to their convenience.
Need for money varies among donors, most common need was expenditure for kids or paying debts. Similar were the needs observed in study done by Jadva et al. In today’s era when we talk of individualized controlled ovarian stimulation, individualized donor needs should also be taken care. We suggest instead of uniform compensation amount, remuneration should be structured to acknowledge the time, inconvenience, expenses, needs and discomfort associated with screening, ovarian stimulation and oocyte retrieval.
On assessing psychological aspects of oocyte donors, none of the oocyte donors felt exploited. Study conducted by Klock et al. found less psychological distress and average self esteem among donor population.
The overall experience of oocyte donors in our study was satisfactory, most of them said they would recommend it to others and would like to do it again. Such results depict centre policies and efficiency and can vary from centre to centre.
CONCLUSION
The egg donors from our center were young, married, housewives and had low family income. They came from vulnerable sections of society with main motivation being monetary compensation. Donors had little knowledge of the detailed procedure, risks involved and possibility of failure. Cancellation of procedure had significant impact on donors. Lack of knowledge and desperation for money expose them to exploitation and poor health. Mild complications such as abdominal pain were faced by donors but accepted well. Overall most donors were satisfied, did not feel exploited and would like to recommend this to others.
There is a need of an efficient and qualitative predonation counseling addressing various doubts and needs of oocyte donors. Also mass media can play a role in increasing awareness amongst oocyte donors so that they can undergo the procedure more satisfactorily and removing the stigma from minds of people regarding oocyte donation. Significant personal disturbances and challenges in life of oocyte donors need to be addressed. A strict government policy is a need of the hour in India in order to make procedure free from exploitation, stigma and poor health for oocyte donors and safeguard their interest.
Strengths of our study were in-depth interview-based study comprising large sample size of Indian donors and various steps were taken to reduce any bias.
Limitation was that subjects from only one ART center were included, further multicenter studies should be planned so that data can be more generalized on donor population.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- The huge burden of infertility in India − Are we crumbling underneath? Glob J Reprod Med. 2018;5:555670.
- [Google Scholar]
- National guidelines for accreditation, supervision and regulation of ART clinics in India. New Delhi: Ministry of Health and Family Welfare, Government of India; 2005.
- A study of recipient related predictors of success in oocyte donation program. J Hum Reprod Sci. 2012;5:252-7.
- [Google Scholar]
- Assisted reproductive technology in India: A 3 year retrospective data analysis. J Hum Reprod Sci. 2013;6:235-40.
- [Google Scholar]
- Pregnancies following egg donation associated with more than 3-fold higher risk of hypertension. ScienceDaily 2014 July 1 Available at: www.sciencedaily.com/releases/2014/07/140701091446.htm
- [Google Scholar]
- Indian egg donors’ characteristics, motivations and feelings towards the recipient and resultant child. Reproductive BioMedicine and Society Online. 2016;1:98-103.
- [Google Scholar]
- Oocyte donation in India − Characteristics of donors. P −771, 32nd Annual Meeting of ESHRE, Helsinki, Finland, 3 July-6 July, 2016
- Press Note on Poverty Estimates, 2011–12. Planning Commission; Report of the Expert Group to Review the Methodology for Estimation of Poverty Planning Commission. PRS 2009
- [Google Scholar]
- Psychological characteristics and factors related to willingness to donate again among anonymous oocyte donors. Fertility and Sterility. 2003;79:1312-16.
- [Google Scholar]
- Sociodemographic and fertility-related characteristics and motivations of oocyte donors in eleven European countries. Hum Reprod. 2014;29:1076-89.
- [Google Scholar]
- Systematic review of oocyte donation: Investigating attitudes, motivations and experiences. Hum Reprod Update. 2009;15:499-515.
- [Google Scholar]
- US oocyte donors: A retrospective study of medical and psychosocial issues. Human Reproduction. 2009;24:3144-49.
- [Google Scholar]
- The incidence of both serious and minor complications in young women undergoing oocyte donation. Fertility and Sterility. 2008;90:2165-217113.
- [Google Scholar]







