Translate this page into:
A prospective study to correlate serum progesterone levels and clinical pregnancy outcome in frozen embryo transfer cycles
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Methods:
Total 100 patients were included in the study and divided into two groups (A and B). Blood levels of p4 were measured when beginning progesterone and on the day of Frozen embryo transfer (FET) in one group and were supplemented if levels were less than 10 ng/mL. No measurement of serum p4 was undertaken in the other group (B). Statistical tests like chi square test and Mann-Whitney test were applied and SPSS version 23 was used.
Outcome:
Clinical pregnancy outcome.
Results:
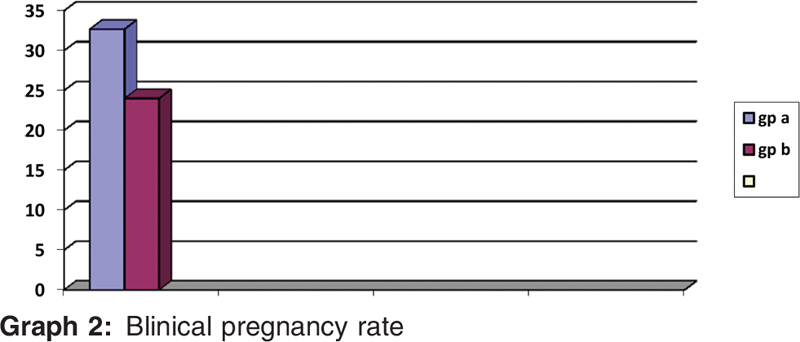
Clinical pregnancy rate was 32.69% in group A vs 24% in the other group which is non-significant.
Conclusion:
Serum p4 should be between 1.5 and 24 ng/mL on the starting day for a positive result. Level in blood on the day of starting progesterone to obtain a positive clinical pregnancy was 0.21 ng/mL and should not exceed 0.96 ng/mL.
Keywords
Clinical pregnancy rate
FET
serum progesterone
INTRODUCTION
Progesterone as a hormone is required for embryo implantation and carrying on a pregnancy. Progesterone is a sex steroid needed for maintaining pregnancy. Once the embryo prepares for implantation, progesterone comes into play and supports the process. Initially, in the first phase, corpus luteum provides support for embryo to implant and grow and later this role is taken over by the placenta.
In the era of assisted reproduction, during the process of ovum pick up, we remove the granulosa cells which leads to a progesterone deficiency. Also the increased use of gonadotropin analogues to prevent premature luteinising hormone (LH) surge adds to the deficit. Keeping this in mind, we need to provide progestational support.
Progesterone as pregnancy support has been extensively studied and co-related with achieving a successful clinical pregnancy. Serum progesterone levels on the day of embryo transfer (ET) in fresh donor in vitro fertilisation (IVF)/ICSI cycles were positively correlated with clinical pregnancy and live birth rates.[1]
World is increasingly moving towards frozen embryo transfer cycles due to various reasons. In Frozen embryo transfer (FET) cycles, the same phenomenon of luteal phase deficit continues. These patients, specifically, are unable to provide endogenous progesterone either due to hormone deficit or suppression and thus require supplementation to initiate and maintain the secretory endometrium thus leading to pregnancy.[2] There has been various previous researches into luteal phase support in frozen cycles, which has shown that supplementation of progesterone does impact cycle outcome in frozen ET. Hence, established that progesterone is of utmost importance, there is mixed data on optimal values for serum progesterone during luteal phase on the day of transfer.
This study aims to determine whether measuring serum progesterone affects clinical outcome in frozen embryo transfer and to establish an optimum value for it.
AIMS AND OBJECTIVES
This article aims to study the role of measuring serum progesterone levels in frozen embryo transfer cycles and to establish a cut-off value in optimising outcome.
MATERIALS AND METHODS
Setting: ARMC IVF Centre, Kerala.
Study design: Prospective case-control study.
Study period: August 2018 to December 2018.
Ethical clearance was obtained from the independent ethics committee (Indian Fertility Society)
SAMPLE SIZE
At our centre, around 25 to 30 patients are recruited for IVF every month. According to the previous literature, the pregnancy rate in patients in whom progesterone measurement was done at serial intervals during the IVF cycle was around 65%. Assuming a lesser pregnancy rate of 50% in a resource-limited setting like ours and patients undergoing IVF during the study period duration (population size), 80% power and 95% confidence interval, we calculated a sample size of 100 by the following formula:
4 pq/d2
where p = existing pregnancy rate (p = 50)
q = 100−p = 50
d = 20% of p = 10
Methodology
This is a prospective case-control study conducted in ARMC IVF, Kerala, from August 2018 to January 2019. All patients undergoing cryopreserved grade 1 and 2 quality day 2/3 and blastocyst transfer cycles were included in the study after considering the inclusion and exclusion criteria. Proper consent was taken from the patients.
Inclusion criteria
All embryos cryopreserved from women 20 to 40 years of age.
Cryopreserved cleavage stage embryos, morula and blastocyst.
Endometrial thickness on day of starting progesterone >7 mm.
PCO patients.
Tubal factor infertility.
Mild-to-moderate endometriosis.
Exclusion criteria
Age of patient >40 years.
Endometrial thickness on day of starting progesterone <7 mm.
Adenomyosis or intramural fibroid >4 cm.
History of recurrent implantation failures or RPL.
Severe male factor.
Stimulation protocols were chosen based on patient characteristics and baseline ovarian reserve tests. Mostly, we used recombinant FSH (follisurge/recagon) and antagonist (cetrolix) for ovarian stimulation. When at least two lead follicles reached ≥17 to 18 mm, a trigger was given based on serum estradiol values and the number of follicles at trigger. Ovum pick up was performed 35 hours after the trigger transvaginally.
Embryos on the day of ET were transferred into the inner catheter whereas the outer catheter was kept at the level of internal OS. The positioning of inner catheter was further confirmed by an abdominal ultrasound with the patients’ bladder partially filled.
The patients were divided into two groups − group A wherein serum progesterone was measured on two occasions and group B wherein serum progesterone was not measured. It was measured on the day of starting progesterone and on the day of transfer. Before embryo transfer, progesterone was admistered via oral route (tablet duphastone 10 mg bd) and post-transfer oral route (tablet duphastone 10 mg tds) and subcutaneous route (inj aqua susten 25 mg) daily if serum progesterone was <10 ng/mL in group A and only oral progesterone in group B pre- and post-transfer till patients were called on day 14 for measurement of serum beta human chorionic gonadotropin (hCG).
Outcome measures
Pregnancy rates between the two groups.
Optimal value of serum progesterone for a clinical pregnancy.
Pregnancy was seen by measuring serum beta hCG, that is value of more than 25 on day 14 of embryo transfer.
Clinical pregnancy rate was determined by presence of a gestational sac as in sixth week of pregnancy by a trans-vaginal ultrasound.
STATISTICAL ANALYSIS
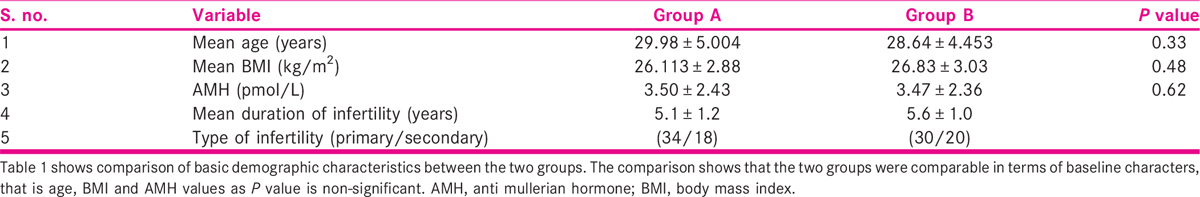
Fifty patients were recruited in both group A and group B. Both groups were comparable in terms of demographic measures.
For all descriptive and statistical analysis, statistical package for social sciences (SPSS) version 23 will be used. The distribution of data was analysed to assess for parametric vs non-parametric analysis. The values of all continuous variables was expressed in mean and standard deviation for each group separately. All categorical variables were expressed in number out of total and their respective percentages. Appropriate statistical tests including chi square test, Student t test or Mann-Whitney U test and Pearson’s correlation were used. For all tests, a P value of less than 0.05 was considered significant and confidence interval was kept at 95%.
RESULTS
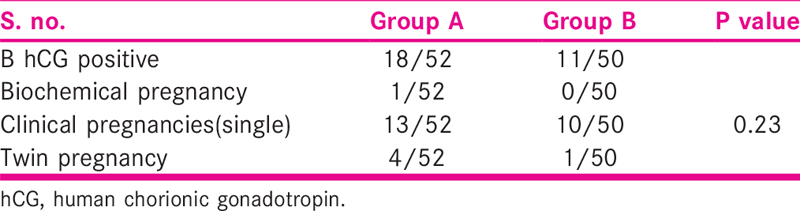
Clinical pregnancy rate was 32.69% in one group as compared to 22% in the other group [Table 4]. The probability value was 0.22. The result was non-significant.
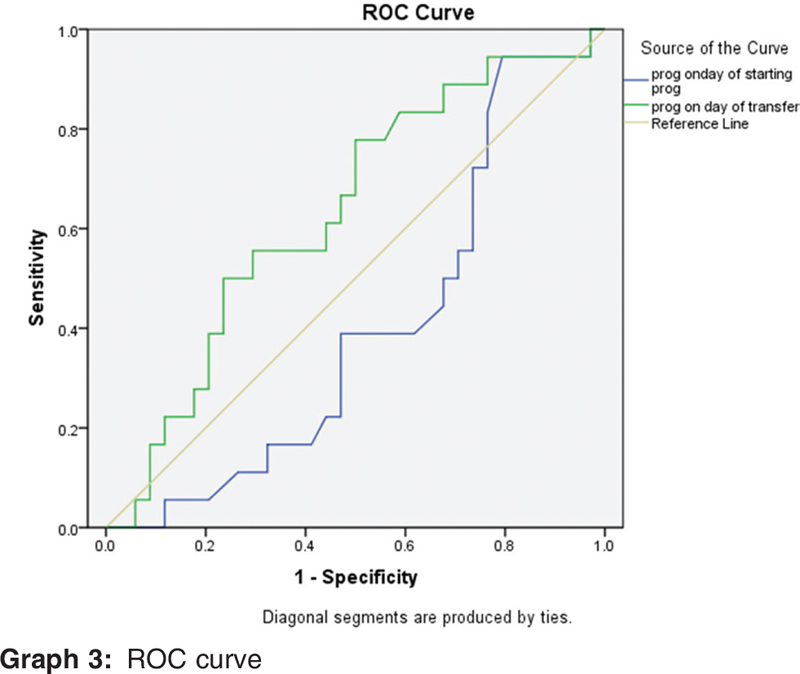
Receiver operating characterstic (ROC) curve showed that blood level when beginning progesterone in a cycle should be between 0.21 and 0.96 ng/mL for pregnancy to occur [Table 5].
Also we saw that value of level of progesterone on the day of frozen embryo transfer should be between 1.5 ng/mL and not exceed 24 ng/mL. However, values above 7.00 ng/mL were associated with 61% sensitivity and 47% specificity of attaining a clinical pregnancy.
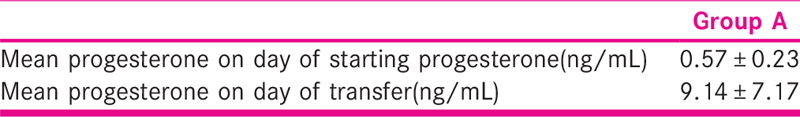
On the day of FET, mean blood progesterone was 9.14 ± 7.17 pg/mL in group A [Table 3].
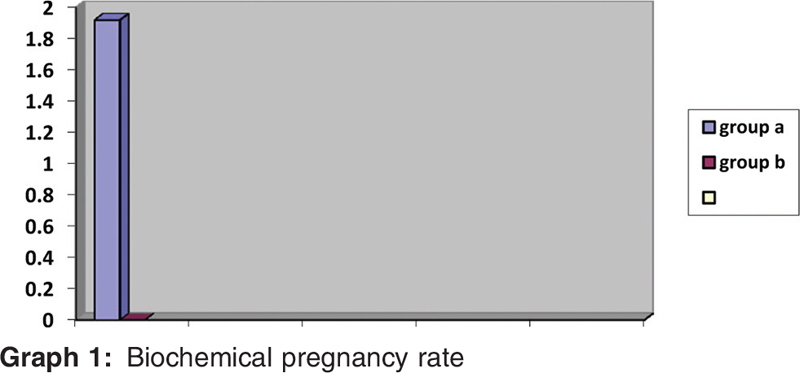
Biochemical rate of pregnancy was 1.92% in group A and 0% in group B [Graph 1].
CPR (rate of clinical preg) was 32.69% in group A and 22% in group B. The P value was 0.22. The result was non-significant [Graphs 2 and 3].
Level in blood on the day of starting progesterone to obtain a positive clinical pregnancy was 0.21 ng/mL and should not exceed 0.96 ng/mL [Table 5].
On the day of FET, blood level of P should be between 1.5 ng/mL and not exceed 24 ng/mL. However, values above 7.00 ng/mL were associated with 61% sensitivity and 47% specificity of attaining a clinical pregnancy.
DISCUSSION
It is already known that progesterone is pregnancy maintenance hormone. It is secreted by corpus luteum in a natural cycle. In IVF, our basic aim is trying to produce a similar microenvironment as inside the body. It has been seen that in mid-luteal phase, serum progesterone concentrations are between 10 and 20 ng/dL.[3]
Earlier belief was that high progesterone ensures a successful pregnancy; however, bovine studies concluded that there is actually a window for the optimum value.[4] Still, research is ongoing on this topic, but it has been shown that transfer done following serial p4 values has an advantage over following cycle day number.[5]
A study performed by Brady et al.[1] said that the results of CPR and live birth rate (LBR) varied with the blood levels of progesterone in fresh donor transfer.
A similar study performed by Venetis et al.[6] in 2015 found that when a multivariable analysis was performed on a cohort of fresh IVF/ICSI cycles, LBR had a fall when blood levels of progesterone rose on the day of trigger.
Nowadays most clinicians are moving towards frozen embryo transfer, be it for medical or elective reasons.
However, such data is deficient as to confirm whether serum progesterone is really required to be measured before a frozen transfer.
A study conducted by Dong et al.[5] in 2014 concluded that performing FET by monitoring mean progesterone level achieved higher pregnancy in comparison with response of ovary to stimulation in a group of patients with similar demographical characteristics.
In our study, we also measured serum progesterone when beginning it, specifically to see any increase before the transfer. Embryo transfer was not done if the value was more than 1 ng/mL.
The comparison showed that the two groups were similar in terms of baseline characters like their age, body mass index (BMI) as well as AMH value [Table 1]. Hence, the bias due to demographic characteristics was taken care of.
The total amount of gonadotropins used, the total number of eggs collected and the mean number of embryos that were being put into the uterine cavity for each patient were same in our two groups (P value non-significant) [Table 2]. Grade 1, two quality embryos and/or blastocysts were transferred after giving oral progestational support according to day of embryo.

Progesterone was administered via oral route (tablet duphastone 10 mg bd) and post-transfer oral route (tablet duphastone 10 mg tds) and subcutaneous route (inj aqua susten 25 mg) daily if serum progesterone is <10 ng/mL in case group A and only oral progesterone in control group B till patients are called on day 14 for measurement of serum b hCG. The patients were divided into two groups: group A (cases) − serum progesterone measured on day of starting progesterone and day of transfer, and group B (controls) − where serum progesterone was not measured.
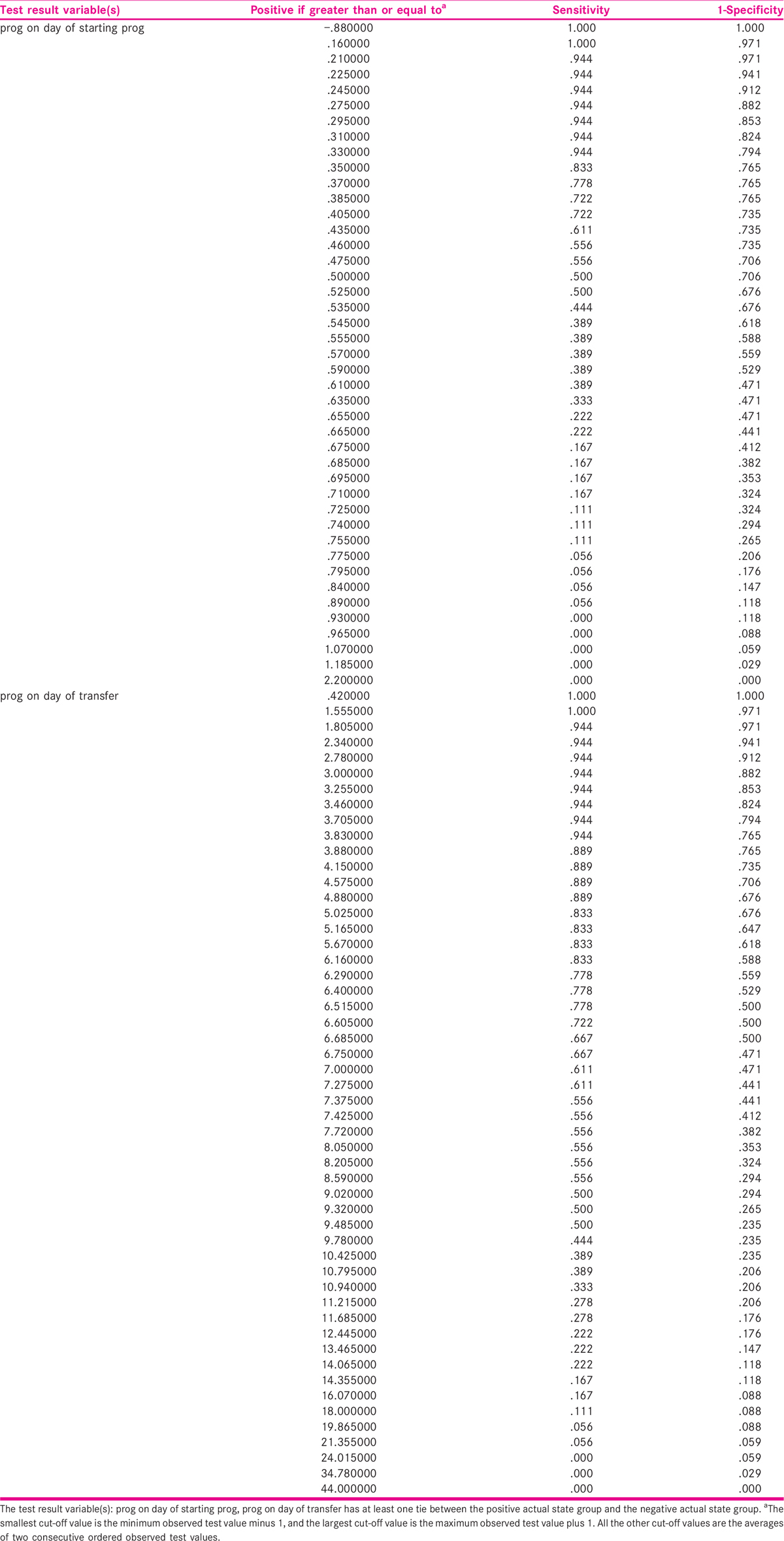
We observed that serum progesterone when beginning progesterone to obtain a positive clinical pregnancy was 0.21 ng/mL and should not exceed 0.96 ng/mL. Also its value on the day of frozen embryo transfer should be between 1.5 ng/mL and not exceed 24 ng/mL. However, values below 7.00 ng/mL were associated with 61% sensitivity and 47% specificity of attaining a clinical pregnancy.
Kofinas et al.[2] in 2015 also said that in transfer of frozen embryos, blood p4 of more than 20 ng/mL are associated with poor outcomes.
Contrastingly, Huang et al.[7] in 2016 published a study wherein they saw premature progesterone levels and concluded that when gonadotropin RH agonist cycles were used, progesterone rise had a bad effect on the outcome in fresh transfer. They also said that FET cycles were unaffected.
Our study showed that although with additional supplementation of progesterone in group A, clinical pregnancy rates were increased (32.69% in one group and 24% in the other); the probability value of this is 0.22. The result remains non-significant.
Looking at biochemical pregnancy rate, it was 1.92% in one group as compared to 0% in the other.
CONCLUSION
Progesterone levels in blood seems to be vital in FET cycles.
There is no consensus in relation to targeted levels of p4 for success of FET cycles.
Our study showed that although with additional supplementation of progesterone in group A if the blood levels of p4 on day of transfer was <10 ng/mL, clinical pregnancy rates were increased (32.69% in cases and 24% in controls) and the probability value was 0.22. The result was non-significant.
Serum p4 should be between 1.5 and 24 ng/mL on the starting day for a positive result.
However, it was a small study due to time restraints and more data may be needed to affirm the same.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Serum progesterone concentration on day of embryo transfer in donor oocyte cycles. J Assist Reprod Genet. 2014;31:569-75.
- [Google Scholar]
- Serum progesterone levels greater than 20 ng/dl on day of embryo transfer are associated with lower live birth and higher pregnancy loss rates. J Assist Reprod Genet. 2015;32:1395-9.
- [Google Scholar]
- Subtle progesterone rise on the day of human chorionic gonadotropin administration is associated with lower live birth rates in women undergoing assisted reproductive technology: a retrospective study with 2,555 fresh embryo transfers. Fertil Steril. 2012;98:347-54.
- [Google Scholar]
- Pregnancy rates relative to recipient plasma progesterone levels on the day of nonsurgical transfer of frozen/thawed bovine embryos. Theriognology. 1985;23:631-9.
- [Google Scholar]
- The frozen-thawed embryo transfer timing determined by serum progesterone level: a retrospective follow-up study. Eur J Obstet Gynecol Reprod Biol. 2014;181:210-3.
- [Google Scholar]
- Basal serum progesterone and history of elevated progesterone on the day of hCG administration are significant predictors of late follicular progesterone elevation in GnRH antagonist IVF cycles. Hum Reprod. 2016;8:1859-65.
- [Google Scholar]
- Premature progesterone rise negatively correlated with live birth rate in IVF cycles with GnRH agonist: an analysis of 2,566 cycles. Fertil Steril. 2012;98:664-70.
- [Google Scholar]