Translate this page into:
Training on transabdominal ultrasound guidance during embryo transfer and proficiency evaluation of training
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Embryo transfer (ET) is the crucial and final step in in-vitro fertilisation (IVF) process which has major impact on IVF outcome. ET technique has been standardized at present and done under ultrasound guidance. But there are no standardised steps described for the transabdominal ultrasound guidance during ET.
Aims:
To define the steps of transabdominal ultrasound guidance during ET using a training module; to evaluate the proficiency and learning curve of training; and to assess the impact on trial ET performance after training.
Settings and design:
A prospective study was conducted in a tertiary assisted reproductive technology (ART) centre, northern India between August 2018 and February 2019.
Materials and methods:
Ultrasound guidance during trial ET was evaluated for 12 doctors who participated in the study on 234 patients. Ultrasound guidance evaluation included scores for USG assessment of trajectory, catheter type prediction, difficulty prediction, ultrasound visualisation during trial ET and trial ET performance. Transabdominal ultrasound guidance training was given to all doctors after 10 pre-training evaluations followed by post-training evaluations. Pre- and post-training mean scores for each doctor and overall were compared using SPSS-21.
Results:
Mean scores showed improvement in all parameters, including trial ET performance for the doctors included in study. Overall, these differences were statistically significant. six doctors (50%) were declared trained in transabdominal ultrasound guidance during trial ET.
Conclusion:
The training module was effective in defining the steps of transabdominal ultrasound guidance during trial ET and improving the trial ET performance.
Keywords
Embryo transfer
training and evaluation
transabdominal ultrasound guidance
INTRODUCTION
Embryo transfer (ET) is the final and the most critical stage in an in-vitro fertilisation (IVF) cycle, having major impact on IVF outcome; it accounts for about 30% failures in case of poor technique.[1] ET involves accurate and atraumatic deposition of embryos by means of an ET catheter into the uterine cavity at an area with maximum implantation potential.[2] The superiority of USG guidance during ET over clinical touch technique has been proven in literature.[3,4,5,6,7,8] However, the technique of guidance has never been described. The current study was conducted with the aim to define the steps of transabdominal ultrasound guidance during ET with the help of Training Module, to evaluate the proficiency and learning curve of training by testing in trial ET and to assess the impact on trial ET performance.
STUDY DESIGN AND SUBJECT
A prospective study was conducted in a tertiary assisted reproductive technology (ART) centre in northern India at Chandigarh from August 2018 to February 2019. The study included two groups of subjects.
Subject 1: Patients
Inclusion criteria: All women who underwent Trial ET during study period (including patients of all categories from normal to obese BMI, H/O of pelvic surgery, endometriosis, PID, genital TB or any uterine pathology)
Exclusion criteria:
Those who did not give consent
Women undergoing fresh/frozen ET
Those who required anaesthesia
Subject 2: Trainees
It is a single centre study and we included all the doctors working at our centre with all levels of experience as trainees except head of our IVF unit who developed the training module. As the number of trainees was only 12, we did not categorise trainees according to the years of experience.
MATERIAL
A training module for transabdominal guidance (TAG) has been developed by the head of our IVF unit who had more than 25 years of experience in IVF. The details of module were demonstrated to all doctors through PowerPoint presentation and clinical demonstration after every doctor who participated in the study completed pre-training 10 evaluations. Post-training evaluations were also done until the doctor is trained (i.e. attained proficiency). The efficacy of training module was tested in this study.
Objectives of the training module
The training module describes how
to project the trajectory of catheter;
to estimate the level of difficulty to be encountered during ET;
to select the type of catheter to be used;
to facilitate the operator to deposit embryo at maximal implantation site.
Principle of training module
The module utilizes the principle of surface anatomy marked with the help of USG. The internal pelvic organs are detected accurately with the help of two-dimensional USG and a curvilinear probe (3.5 MHz). The probe is curvilinear and has a single two-dimensional image frame. When plane of the probe is accurately aligned with the sagittal plane of uterus, the probe position on abdomen overlies the position of uterus and cervix in pelvis. Looking at the probe position on external abdominal wall, the direction of uterine axis, the cervical axis and the angle between the two can be accurately mapped. Thus, a spatial image of relationship of uterus and cervix to pelvic cavity can be made [Figure 1].
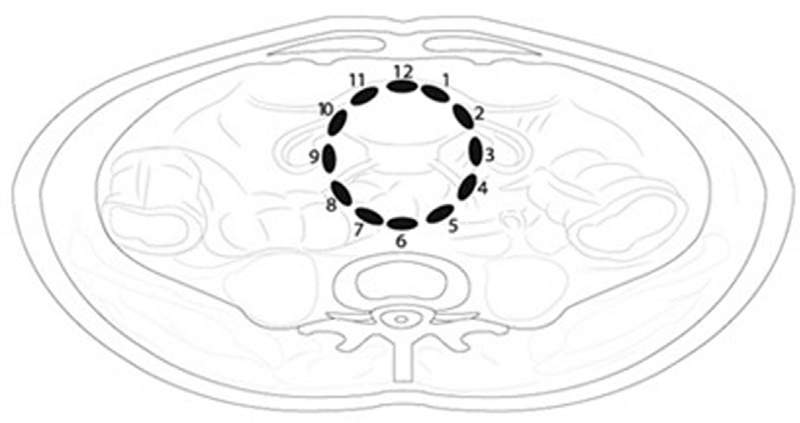
- Spatial image depicting the relationship of uterus & cervix to pelvic cavity
Reference points used in the module
Point A: External os.
Point B: Internal os.
Point C: Fundus of uterus.
-
Trajectory: It is the course of path which the ET catheter needs to traverse from external os (point A) to internal os (point B) and then to fundus of uterus (point C) [Figure 2].
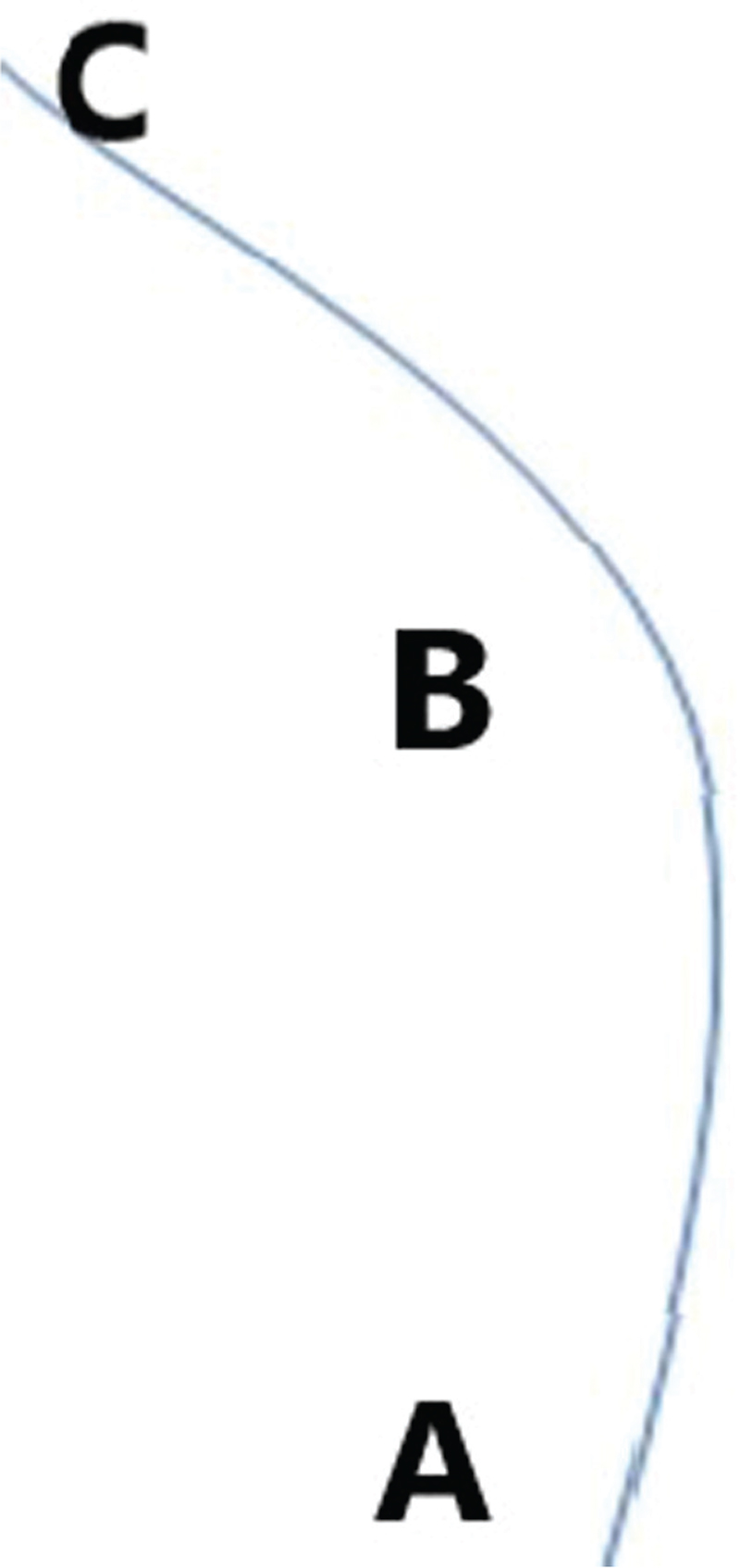 Figure 2
Figure 2- Trajectory
Uterine axis: It is the line joining point C and point B.
Cervical axis: It is the line joining the point A and point B.
Cervical curve: It is the curve of cervical axis between point A and point B.
-
Cervico-uterine angle (CUA) [Figure 3]: It is the angle between cervical axis and uterine axis. For uniformity sake, it would be measured on the anterior side towards bladder.
 Figure 3
Figure 3- Cervicouterine angle
Details of module include the following:
-
Steps to assess the trajectory of catheter: An example is given as pictorial representation [Figure 4a]–g].
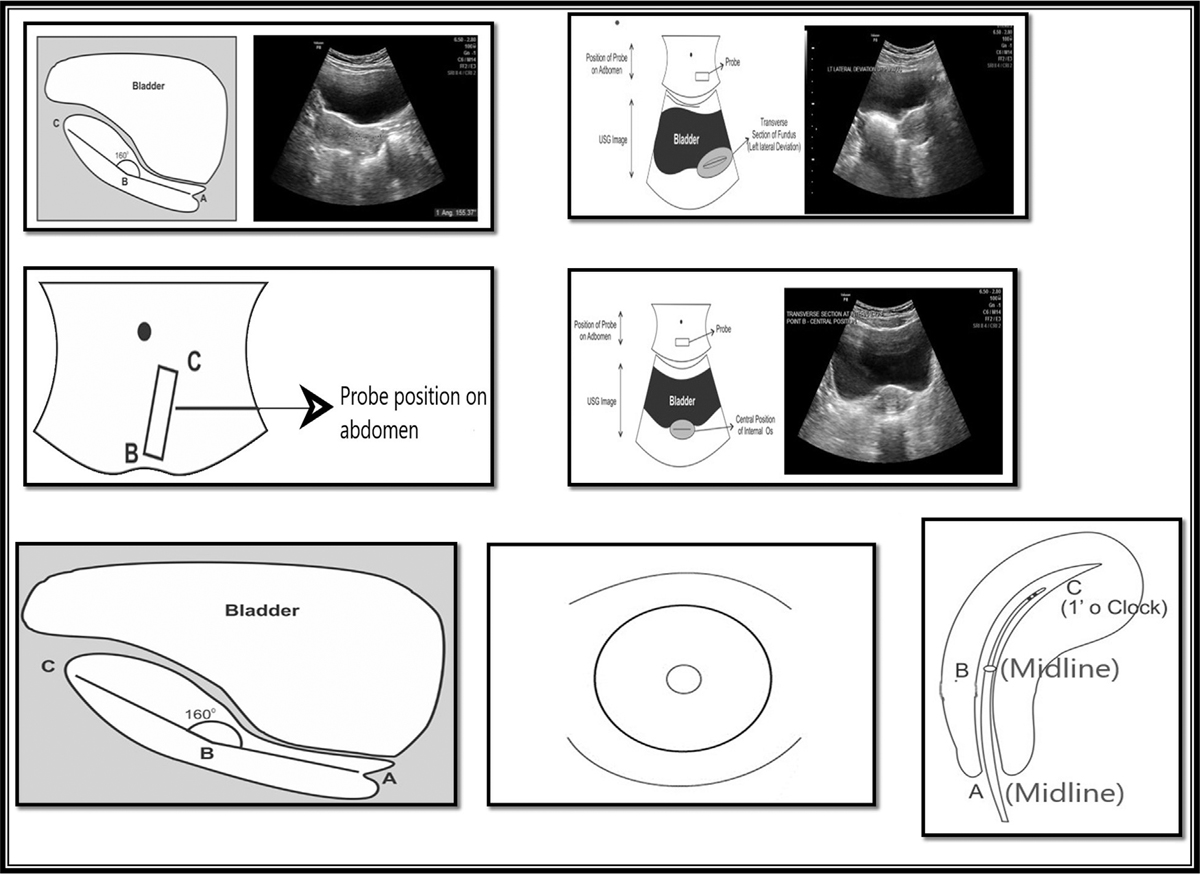 Figure 4
Figure 4- Pictorial representation of stepwise assessment of trajectory. Step 1: Sagittal plane of uterus. Step 2: Transverse section at point C(fundus) to see its relationship with bladder (Fundus is left side directed in the given picture). Step 3: Probe position on abdomen when sagittal image of uterus is focused, upper edge of probe corresponds to the direction of fundus (point C). Step 4: Transverse section at internal os (point B) and its relationship with bladder (Midline position of internal os in the given picture). Step 5: Sagittal image of cervix to look for cervical canal curvature. Step 6: Direction of External os (point A) on per speculum examination (Central position in the given picture). Step 7: Final trajectory (Point A-B-C)
-
Prediction of catheter type needed and the difficulty level:
Based on the cervico-uterine angle measurement and cervical curvature in trajectory assessment, the difficulty level and the appropriate catheter can be predicted.
In general, acute degree of anteflexion or retroflexion and irregular cervical curvature needs a metallic outer sheath to negotiate the internal os.
-
Deposition of embryos at maximum implantation (MIP) site:
Keep sagittal view of uterus and cervix in view.
Keep probe directly above the uterus. Do not tilt.
Stay stationary by putting little more than gentle pressure.
Don’t let the probe slip.
Don’t let the image move. Have very stringent hand–eye coordination. Your hand should move by reflex gently with the breathing.
The vaginal operator confirms and moves the catheter along the path projected.
Transabdominal sonography (TAS) should focus on cervix and external catheter in cervix.
Stay in line with the external catheter rather than the best plane of endometrium.
When the inner catheter comes out in line with external catheter, you can see the whole path.
Deposit 1 cm short of fundus.
METHODOLOGY
Written informed consent was obtained from both subject 1 (women who undergo trial ET) and subject 2 (doctor who does transabdominal USG guidance). Trial ET was done during midluteal phase of previous cycle of stimulation by an operator (respective doctor) under the USG guidance of assistant (any of the trainee doctors). Ultrasound guidance evaluation was done in all trial ETs.
Assistant doctor first performs transabdominal USG and assesses the following five parameters (pre-procedural USG Assessment):
Direction of fundus
Cervico-uterine angle and position of internal os
Cervical canal curvature
Cervical mucous
Cervical direction in vagina
Based on the assessment, pre-trial ET prediction of the following three factors is made:
Trajectory of catheter
Prediction of type of catheter needed: metallic outer sheath or soft
Difficulty level that can be encountered during ET on the basis of aforementioned five parameters over a continuous rating scale ranging from 1 to 10 in increasing difficulty level.
Predictions are kept confidential from the vaginal operator.
Operator then performs trial ET under TA-US guidance using Labotect soft ET catheter initially in all cases. (When there is difficulty in negotiation, then Gynetic metallic outer catheter is used.) Patient is put in dorsal lithotomy position with moderately full bladder. Perineal parts are prepared, bivalved Cusco’s vaginal speculum is inserted and cervix exposed. Mucus in ectocervix is cleaned with cotton swab. Outer sheath is passed through cervix till the bulb is seen beyond internal os and the length of outer sheath is measured. Inner catheter is then passed through outer sheath into uterine cavity 1 cm below the fundus, air bubbles are placed in uterine cavity and length of inner catheter is measured. Inner and outer sheaths are then removed. Positioning of air bubble from the fundus is confirmed by ultrasound.
Operator gives scores for ultrasound guidance after the procedure, which are as follows:
USG assessment score: By comparing actual findings with USG-assessed five parameters by assistant. Total score is 5.
TAG score: This is based on ultrasound visualisation of cervix, internal os, internal catheter, air flush, external and internal catheter with air flush in single window during trial ET. Every parameter is rated 0,1 or 2 score, depending on nil, partial or full visualisation, respectively. Total score is 10.
Trial ET performance score (TET score): Based on the trial ET performance under US guidance, two points are given for each of the following:
Prediction of appropriate catheter by assistant: correct = 2; wrong = 0
Site of deposition of air flush:
<1 cm = 0
1–2.5 cm = 2
>2.5 cm = 0
Blood on outer catheter: yes = 0; no = 2
Total score is 6.
Catheter prediction score: Based on wrong or correct prediction of catheter
Trial ET difficulty score (TED score): The score is given subjectively over continuous rating scale of 1–10 in increasing difficulty level. Because there is no clear definition to differentiate between easy, moderate, and very difficult levels in ET,
score 1–3 was considered as easy;
score 4–6 was considered as moderately difficult;
score 7–10 was considered as very difficult.
Difficulty prediction score: Difficulty score predicted by the assistant is compared with operator’s difficulty score and assessed whether it is correct or incorrect prediction in terms of easy, moderately difficult, and very difficult category.
Training module was taught to all trainees after each doctor completed 10 pre-training evaluations. Same evaluation continued in the post-training period.
When a trainee doctor scores ≥8 out of 10 in TAG in the 10 consecutive post-training evaluations, the doctor was declared trained/proficient in guidance and the number of attempts taken to be declared trained was considered as the learning curve.
USG assessment score, TAG score, TET performance score, catheter prediction and difficulty prediction scores for each of the trainees and overall during pre-training and post-training were compared and analysed in SPSS-21 using chi-square tests.
USG assessment score, TAG score, catheter prediction and difficulty prediction were correlated with TET performance score.
OBSERVATION AND RESULTS
A total of 12 doctors with varying level of experience participated in this training programme.
The total number of ultrasound guidance evaluations done in trial ET during the pre- and post-training periods was 110 and 124, respectively.
We found improvement in all five scores for each doctor but not statistically significant in all the parameters [Table 1].

OVERALL COMPARISON OF PRE- AND POST-TRAINING
-
Overall mean USG assessment score during pre- and post-training is shown in Figure 5.
Mean score of USG assessment was 3.16 in pre-training period and 3.95 in post-training period, which showed a significant improvement (24%, p-value <.001).
 Figure 5
Figure 5- Comparison of mean USG Assessment score pre and post training
-
Overall mean TAG score during pre- and post-training period is shown in Figure 6.
Mean value of TAG score in pre-training period was 7.76 and the mean value of TAG score in post-training period was 8.7. It showed significant improvement (12%, p-value <.001).
 Figure 6
Figure 6- Comparison of mean TAG score during pre and post training
-
Catheter type prediction in pre- and post-training period is shown in Figure 7.
Catheter type prediction was correct in 77% of cases during pre-training period and 91% correct during post-training period, which showed a significant improvement of 17% (p-value .004).
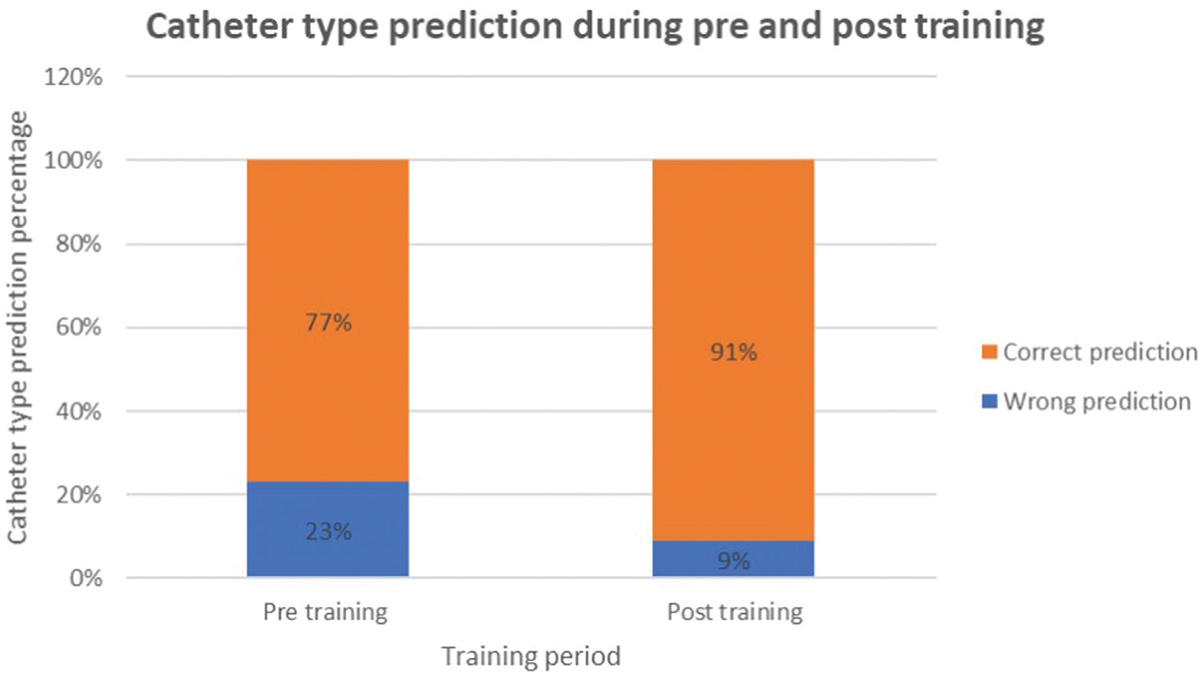 Figure 7
Figure 7- Comparison of percentage of correct catheter prediction during pre and post training
-
Overall mean TET performance score during pre- and post-training period is shown in Figure 8.
Mean value of TET performance score was 5.04 in pre-training period and 5.53 in post-training period, which showed a significant improvement of 9.8% (p-value .001).
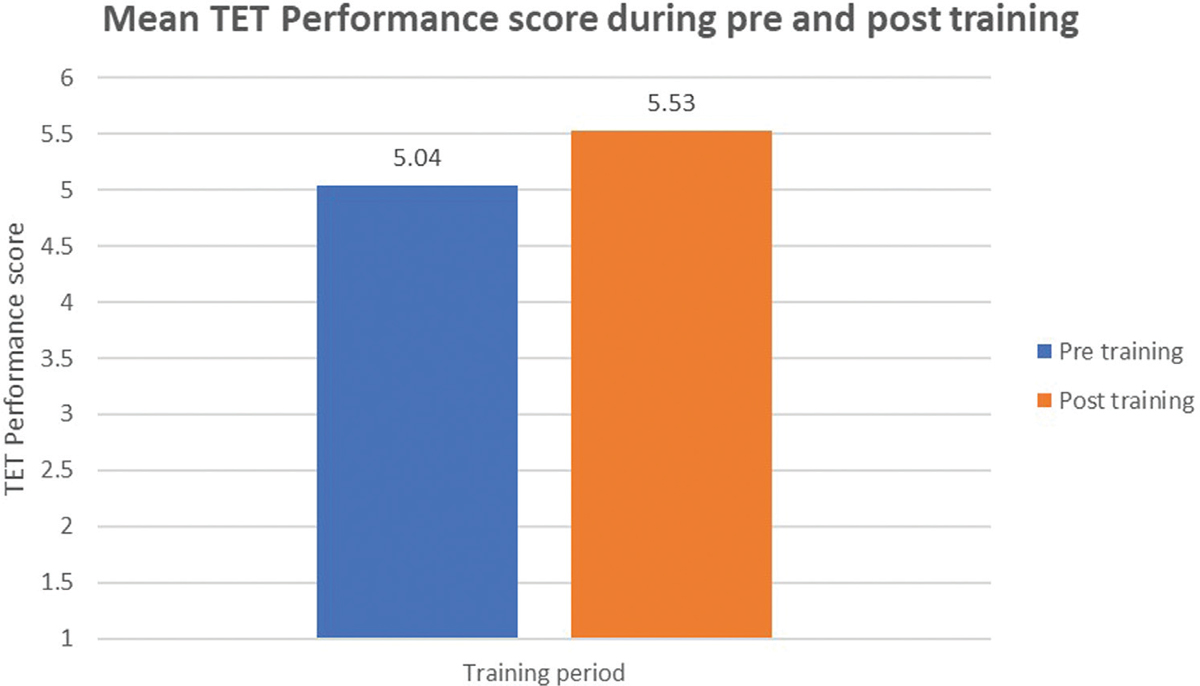 Figure 8
Figure 8- Comparison of mean Trial ET performance score pre and post training
-
Comparison of difficulty prediction during pre- and post-training period is shown in Figure 9.
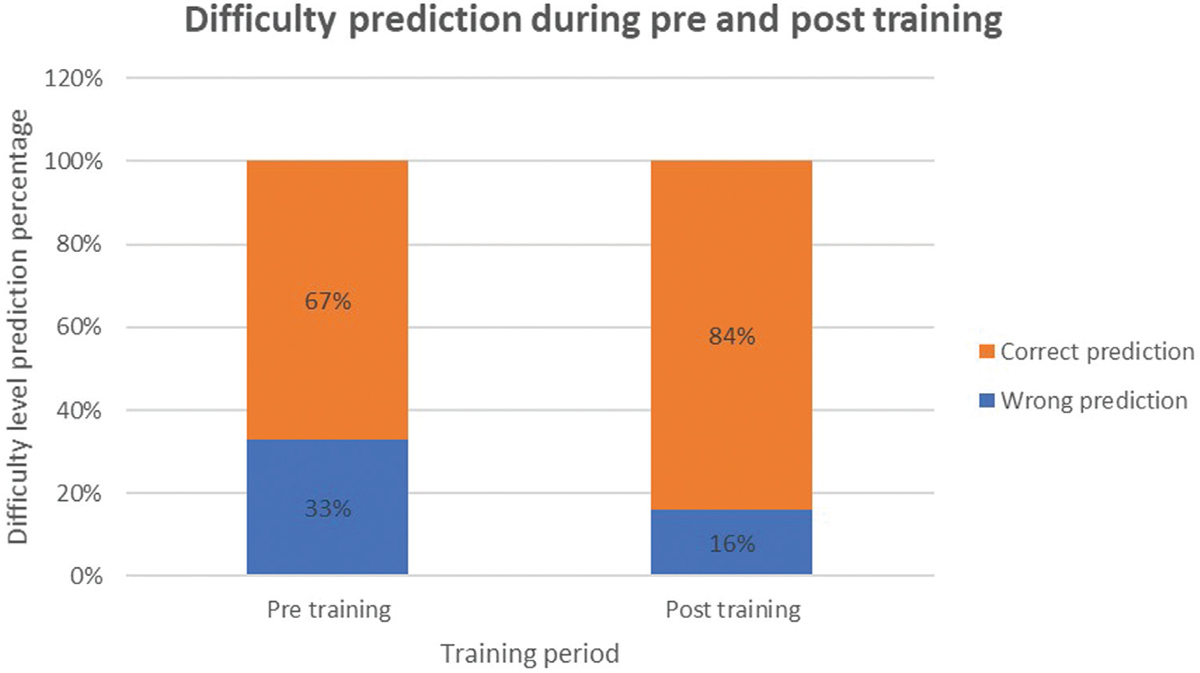 Figure 9
Figure 9- Comparison of difficulty prediction percentage pre and post training
Of the 110 total assessments in pre-training period, 74 predictions (67%) were correct. Of the 124 total assessments in post-training period, 104 predictions (84%) were correct. The difference was statistically significant (p-value .003).
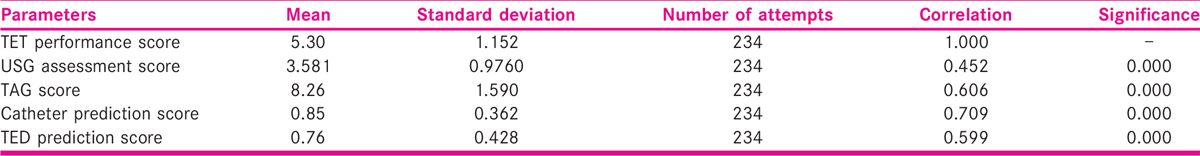
All the scores were positively correlated with TET performance score, which were statistically significant [Table 2].
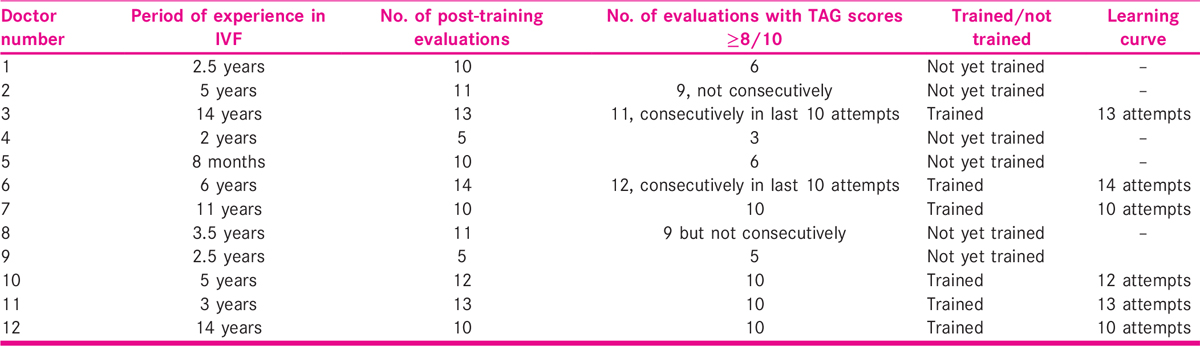
Out of 12 doctors, 6 doctors were declared trained/attained proficiency in transabdominal guidance during trial ET. Six doctors had not attained proficiency during this study period due to time constraint, so they need further more attempts to attain proficiency. Among the six doctors who were declared trained, learning curve ranged from 10 to 14 attempts [Table 3].
DISCUSSION
In 1985, Strickler et al.[9] first reported the use of USG guidance during ET and it was proven to have positive effect on success of ET. Many RCTs and meta-analysis have proven that the USG guidance during ET significantly improved the implantation rate and clinical pregnancy rate and made the procedure all the more easy.[3,4,5,6,7,8]
ASRM committee recommends TA ultrasound guidance during ET to improve clinical pregnancy rate and live-birth rate based on grade A evidence from 10 RCTs.[10] Although ET technique is standardized with the development of common protocol by ASRM, there was no standardized technique defined in literature for the USG guidance during ET. In our study, a training module, which was developed by the head of our IVF unit, defining the steps of transabdominal guidance during ET has been tested and validated. Transabdominal ultrasound guidance was evaluated before and after training during trial ET for each doctor and overall. Guidance evaluation was done with five different scores: USG assessment score, TAG score, catheter prediction score, TET performance score and difficulty prediction score.
In a prospective study by Ghaffari et al.,[11] effects of easy and difficult ETs on implantation and pregnancy rate were analysed in 706 ETs over 1 year period. They found a significantly higher implantation (21.7%) and pregnancy rate (38.1%) in easy group compared to difficult group (12.1% and 21.4% with p-value <.05). They concluded that difficult ETs adversely affect the IVF outcome and precautions must be taken to identify those difficult cases in advance. In another prospective study conducted during January 2017 to January 2018, Fayed et al.[12] investigated clinical and ongoing pregnancy rate in difficult ET cases among 417 women who underwent ET; they found that the biochemical, clinical and ongoing pregnancy rate were significantly reduced in difficult ET compared to easy ETs (ORs 0.5, 95% CI: 0.31–0.83); 0.48, 95% CI: 0.29–0.79; 0.36, 95% CI: 0.21–0.62, respectively).
However, there are no standard assessment techniques to predict these difficult cases beforehand; if these cases are encountered unexpectedly, it lowers the pregnancy rate. In our study, the training module defining steps of trajectory assessment, predictions of catheter type and difficulty level were tested and we found a statistically significant (p-value .003) improvement in difficulty prediction in post-training (84% correct prediction) compared to pre-training (67% correct prediction). Prediction of difficult cases beforehand and taking necessary precautions can minimise the difficulties during ET and improve pregnancy rate. A literature review was published by Schoolcraft et al.[13] on techniques and variables affecting the success of ET outcome. In the review, potential advantages of transabdominal ultrasonographic guidance during ET were reported as follows. It helps in assessment of endometrium and ovaries for any condition that precludes ET, facilitates placement of soft-type catheter, ensures that catheter has passed beyond internal os − especially in patients with elongated cervical canal, helps in directing the catheter along contour of uterine cavity, helps to avoid touching the fundus and thereby avoiding the initiation of uterine contractions and helps to avoid disrupting the endometrium and plugging of catheter tip with the endometrium and instigation of bleeding. However, the technique of transabdominal USG guidance during ET to achieve these potential advantages was not described.
In our study, the training module on transabdominal US guidance during ET has described the techniques to assess the trajectory of catheter from external os till upper uterine cavity, to predict the difficulty level, to select the type of ET catheter and to place the embryos at maximum implantation potential point. This module was tested in our study by comparing the mean scores of USG assessment, TAG, catheter type prediction, TET and difficulty prediction before and after training. We found improvement in all five scores in each individual trainee doctor but not statistically significant in all the parameters.
In the overall assessment, we found a statistically significant improvement in USG assessment score, TAG score, TET performance score, catheter type prediction and difficulty prediction with p-values of <.001, <.001, <.001, <.004 and <.003, respectively.
USG assessment score, TAG score, catheter prediction score and difficulty prediction score had a positive correlation with TET performance, which was statistically significant (p-value <.001 in all correlations).
Of the total doctors, 50% (n = 6) were declared trained in transabdominal guidance during trial ET. Six doctors had not attained proficiency during this study period due to time constraint, so they would need further more attempts to attain proficiency. Among the six doctors who were declared trained, learning curve ranged from 10 to 14 attempts.
We had tested the training module only in trial ET, so we did not include secondary outcome such as pregnancy rate. We are continuing this study in actual ET along with secondary outcome.
An interview was conducted among the participated doctors in the post-training period in which all the doctors said that they gained knowledge with USG guidance training programme in projecting the catheter during ET, selecting the type of catheter and prediction of difficulty level to be encountered during ET, although they are not fully trained. When they were asked how they want to teach their residents/fellows about the technique and guidance of ET, they said they all wanted to teach and train with this module as there is no other standardized US guidance technique described in literature.
Nearly 70% ET are straightforward and can be guided by ART practitioners with some experience. However, because of the importance of ET in the success of IVF procedure, fellows do not get much chance to do ET. This training module can shorten their learning curve. In ETs rated as moderately difficult, an expert guidance can make the procedure easy and help in accurate placement of embryos. In about 10% cases, ET are really difficult and the pre-procedure projection of trajectory, difficulty level, catheter selection, expert operator and USG assistant can make procedure successful and avoid disasters at the time of ET.
CONCLUSION
The training module on technique of transabdominal ultrasound guidance during ET was found to be effective overall in assessing the trajectory of catheter by USG, predicting appropriate catheter type, predicting difficulty level and improving trial ET performance. Hence, the training module can shorten the learning curve for ET among beginners in ART. The limitation of this study was that it is smaller study conducted in a single centre. Reproducibility needs to be validated on a larger sample size and at multicentres to include more number of operators. We are continuing this study on a larger sample size. A simulator can be developed for ultrasound guidance and added to ET simulator to teach both guidance and transfer aspects of ET which are equally important.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Embryo replacement technology. In: 31 Annual Post Graduate Course. San Francisco, CA: ASRM; 1998.
- [Google Scholar]
- Embryo transfer. New Delhi: Jaypee Brothers Medical Publishers; 2008. p. :558.
- Ultrasound guidance during embryo transfer: a systematic review and meta-analysis of randomized controlled trials. Ultrasound Obstet Gynecol. 2015;45:139-48.
- [Google Scholar]
- Ultrasound guided soft catheter embryo transfers will improve pregnancy rates in in-vitro fertilization. Hum Reprod. 2000;15(1):107-12.
- [Google Scholar]
- Embryo transfer under ultrasound guidance improves pregnancy rates after in-vitro fertilization. Hum Reprod. 2000;15(3):616-20.
- [Google Scholar]
- The echoguide embryo transfer maximizes the IVF results. Acta Eur Fertil. 1995;26:113-5.
- [Google Scholar]
- Ultrasound-guided embryo transfer significantly improves pregnancy rate in women undergoing oocyte donation. Int J Gyn Obstet. 1999;66:281-4.
- [Google Scholar]
- Ultrasound versus ’clinical touch’ for catheter guidance during embryo transfer in women. Cochrane Database Syst Rev. 2007;24(1):D006107.
- [Google Scholar]
- Comparison of easy and difficult embryo transfer outcomes in in vitro fertilization cycles. Int J Fertil Steril. 2013;6(4):232-7.
- [Google Scholar]
- Pregnancy outcome after difficult embryo transfer in IVF-ET cycles. Egypt J Hosp Med. 2018;71(2):2564-72.
- [Google Scholar]
- Embryo transfer: techniques and variables affecting success. Fertil Steril. 2001;76(5):863-70.
- [Google Scholar]







