Translate this page into:
Adjuvant therapy in assisted reproduction treatment (ART): Current evidence and recommendations for clinical practice
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
There is an ever-growing list of a wide variety of pharmacological agents and interventions being implicated as adjuvant therapies alongside the core fertilization techniques—IVF or ICSI. Most of the data to support use of these adjuvant therapies are based on anecdotal, heterogeneous, and underpowered studies and associated with controversial results. Clinicians should be fully aware of the best available current evidence and patients must be informed about the experimental nature of any adjuvant therapy being offered to them, when there is no robust evidence of its safety and/or effectiveness. Any adjuvant therapy should be offered only if there is potential for cost-effective, physiological, and psychological benefit and a minimum risk of harm. Further research in the form of good quality preferably RCTs on a large number of infertile couples is required to establish true effectiveness and safety of various adjuvant therapies.
Keywords
Adjuvant therapy
clinical practice
current evidence
in vitro fertilization-art
recommendations
Despite remarkable improvement in IVF technology and resulting pregnancy rates over last four decades, a significant proportion of infertile couples still fail to conceive. Inability to achieve success, especially after repeated attempts, is devastating for the infertile couple and a huge clinical challenge for the infertility specialists. Several additional therapies and new techniques have been proposed in last few years to meet these challenges. While there is a natural inclination for both infertile couples and specialists to try any new pharmacological agent/intervention having potential to improve pregnancy chances, it is extremely important that the clinicians are fully aware of the best available evidence about clinical effectiveness and safety profile of any empirical therapy/intervention, before offering same to the patients.[1,2,3]
The term “adjuvant therapy” (also termed as adjunct therapy or add-on therapy) is used for the agents, tools or procedures that can be implemented alongside the core assisted reproduction technique—IVF or ICSI with the aim of improving fertility outcomes. According to the HFEA’s most recent national fertility patient survey, three quarters of patients who had fertility treatment in the last two years had at least one type of treatment add-on.[1,2,3] However, most of the data supporting these adjuvant therapies are based on anecdotal, heterogeneous and underpowered studies, leading to debatable interpretation.[4,5,6]
This article summarizes the current scientific evidence and international recommendations on the use of various adjuvant therapies in ART cycles. While numerous adjuvants have been proposed to improve IVF success rates, the more commonly used adjuvant therapies in current practice can broadly be grouped under following subheadings (Adapted and modified from Zemyarska MS 2019)[4]:
Adjuvants for ovarian response/oocyte
Androgens—Dehydro-epiandrostenedione (DHEA) and Testosterone
Growth hormone (GH)
Metformin
Antioxidants
Artificial oocyte activation (AOA)
Adjuvants for sperm
Sperm DNA Fragmentation tests and Antioxidants
Advanced sperm selection techniques including
Intracytoplasmic Morphologically Selected Sperm Injection (IMSI)
Physiological Intracytoplasmic Sperm Injection (PICSI)
Adjuvants for embryos
Time-lapse embryo imaging
Embryo Glue
Assisted hatching (AH)
Elective “freeze all” cycle
Preimplantation Genetic Screening (PGS)/Preimplantation Genetic Testing for Aneuploidy (PGT-A)
Autologous Endometrial co-culture
Adjuvants for endometrium/implantation
Estrogen
Aspirin
Heparin
Vasodilators—Nitroglycerine (NTG), Sildenafil, L-arginine.
Uterine relaxants—β 2 adrenergic antagonists, Piroxicam, Atosiban.
Endometrial scratching/Endometrial injury (EI)
Reproductive immunology testing and potential therapies
Corticosteroids
Intravenous Immunoglobulin (IVIG)
Anti-Tumour Necrosis Factor-α (TNF-α) agents
Intralipid infusion
Granulocyte-Colony Stimulating Factor (G-CSF)
Autologous Platelet Rich Plasma (PRP) therapy
Intrauterine hCG administration
Autologous Peripheral Blood Mononuclear Cells (PBMC)
Alternative therapies as adjuvants
Acupuncture
Yoga
ADJUVANTS FOR OVARIAN RESPONSE/OOCYTE
Androgens
Dehydro-epiandrostenedione (DHEA). DHEA is one of the most commonly used adjuvants in poor ovarian responders. DHEA is a dietary supplement widely available online and is unlicensed in Europe.[5] It is thought to enhance follicular function in older women with diminished follicular reserve by increasing the production of insulin-like growth factor-1 (IGF-1) and augmenting estradiol production in granulosa cells, acting as a precursor of androstenedione and testosterone in the theca cells.[5]
It has been suggested that DHEA improves the number of antral follicles available for stimulation, since it is believed to have a role in antral follicle development[7]; however, reports on the potential benefits have been mixed.[8] Initial observational studies showed improved ovarian response and increased numbers of oocytes retrieved, however, the cohorts were heterogeneous and generally small.[8] DHEA is usually recommended as 75 mg/day for a period of 2–3 months.
A Cochrane review[9] showed higher live birth rates (LBRs) following the use of DHEA (OR 1.88, 95% CI 1.30 to 2.71). However, no benefit was apparent when studies with high risk of performance bias were excluded.[9] The included RCTs in this review were of moderate quality and the safety data were insufficient. Although minor androgenic side effects have been reported, long term risk of DHEA administration remains unknown.
Testosterone. Testosterone has an important role in reproductive process and intrafollicular physiology and has been advocated as adjuvant in poor ovarian responders. It is usually administered trans-dermally (testosterone gel 12.5 mg once daily for 21 days or 2.5 mg testosterone patch for 5 days prior to ovarian stimulation for IVF). Few studies have reported higher clinical pregnancy rate and live birth rate in poor responders undergoing ovarian stimulation for IVF, after pretreatment with transdermal testosterone.[10,11] However more RCTs with larger sample size are needed to reach further conclusions.
Recommendation(s): In poor responder women undergoing ART, pre-treatment with DHEA or testosterone may be associated with improved live birth rates. However, the overall quality of the evidence is moderate. Definitive conclusion regarding clinical role of either androgen awaits evidence from further well-designed studies.[9]
Growth hormone (GH)
GH regulates the effect of FSH on the granulosa cells of the ovary by increasing the synthesis of IGF-I and has role in ovarian function including follicular development, estrogen synthesis, and oocyte maturation.[12,13]
Several studies have shown the beneficial effect of GH therapy to improve ovarian response. GH is usually started on the first day of ovarian stimulation and is administered either daily or on alternate days. The doses used in the studies have varied from 8 to 24 IU/day.[5] More recently, a prospective study reported a low-dose (0.5 IU/ day) of GH to be sufficient to improve the clinical pregnancy rates (CPR) in poor responders.[14] A Cochrane review of 10 RCTs demonstrated significantly higher CPRs and live birth rates (LBRs) when GH was added in women suspected of having a low ovarian response.[15] However, this review also put a caution in interpreting the result as the RCTs included in the meta-analyses were too few in number and too small in sample size to draw a definitive conclusion. Only the CPRs were significantly better, but not LBRs, in the sub-group of women who showed a low response in the previous treatment cycle.[15] No benefit was apparent when GH as an adjuvant was used in normal responders.
A subsequent RCT showed no difference in clinical pregnancy rate and live birth rate when GH was added to a gonadotrophin-releasing hormone (GnRH) antagonist protocol in poor responders.[16] Thus there is no clear evidence of benefit in supplementing IVF cycles routinely with GH. There may be a positive effect in the use of GH supplementation in poor responders; however, studies have been weak and heterogeneous, and larger trials are needed.
Recommendation(s): The usefulness of GH as an adjuvant in IVF cycles remains inconclusive.[5] The available evidence does not support the routine use of GH as an adjuvant in IVF cycles.[8]
Metformin
Both obese and non-obese women with Poly Cystic Ovary Syndrome (PCOS) are more insulin-resistant and hyperinsulinemic than age- and weight-matched women with normal ovaries.[8] Thus there appear to be factors in women with PCOS which promote insulin resistance that is independent of obesity.[8] Women with PCOS who are oligomenorrheic are more likely to be insulin resistant than those with regular cycles, irrespective of their body mass index.[8] These Women with polycystic ovaries are also at increased risk of ovarian hyperstimulation syndrome (OHSS). Insulin-sensitizing agents such as metformin were thought to have potential in the management of PCOS.
The first RCT[17] to compare metformin with placebo in IVF cycles in women with PCOS comprised a randomized group of 101 consecutive cycles using a conventional long GnRH agonist protocol and metformin 850 mg twice daily for 4 weeks before oocyte retrieval.[8] There were no differences in total FSH dose, number of oocytes retrieved or overall fertilization rate; however, a significant increase in clinical pregnancy rate beyond 12 weeks (38.5% vs 16.3%, P = 0.023) and a clinically significant reduction in severe OHSS were reported (3.8% vs. 20.4%, P = 0.023). Metformin was also shown to attenuate the ovarian secretion of vascular endothelial growth factor (VEGF), which is thought to be crucial in the pathophysiology of OHSS. A Cochrane review[18] concluded that the main benefit of metformin in the context of IVF for women with PCOS was for the prevention of OHSS (OR: 0.27, 95%Cl: 0.16–0.47).
Few studies suggested that metformin may achieve a reduction in miscarriage, but this has since been shown not to be the case.[19] Women with PCOS are prone to increased risk for complications in pregnancy including gestational diabetes, pregnancy-induced hypertension, pre-eclampsia, and neonatal morbidity.[20] A large Norwegian multi-center RCT[21] found no improvement in these complications with continued use of metformin throughout pregnancy, although there appeared to be a reduction in late miscarriage and pre-term delivery rates. Metformin so far has a good safety profile in healthy women and early pregnancy with no evidence of teratogenicity, although gastrointestinal side effects occur in approximately 10% of patients.[8]
Recommendations(s): The available evidence suggests that metformin may have some beneficial effects in women with PCOS undergoing IVF by reducing the risk of developing OHSS and increasing the pregnancy rates.[8]
Antioxidants
Oxidative stress can lead to cell membrane lipid peroxidation, cellular protein oxidation, and DNA damage, causing a negative effect upon the oocyte, the embryo, and implantation.[22] Antioxidants are expected to counteract the negative impact of oxygen-free radicals by acting as free radical scavengers. A Cochrane review on “Antioxidants for female subfertility” (2017) extracted the data from 50 trials wherein the investigators compared oral antioxidants, including combinations of antioxidants, Nacetyl-cysteine, melatonin, L-arginine, myo-inositol, D-chiro-inositol, carnitine, selenium, vitamin E, vitamin B complex, vitamin C, vitamin D+calcium, CoQ10, pentoxifylline and omega-3-polyunsaturated fatty acids versus placebo, no treatment/standard treatment or another antioxidant.[23] In this review, very low-quality evidence suggested an increased clinical pregnancy rate (OR 1.52, 95% CI 1.31 to 1.76, P < 0.001) and increased live birth rate (OR 2.13, 95% CI 1.45 to 3.12, P > 0.001) among women using antioxidants compared with placebo or no treatment/standard treatment. There was insufficient evidence to draw any conclusions about adverse events.[23]
In the same Cochrane review, very low-quality evidence suggested that pentoxifylline may be associated with an increased clinical pregnancy rate compared with placebo or no treatment (OR 2.07, 95% CI 1.20 to 3.56, P = 0.009).[22] The authors concluded that in this review, there was very low-quality evidence to show that taking an antioxidant may provide benefit for subfertile women.[23]
CQ-10 is also one of the antioxidants that has been studied to have a role in improving female infertility. Mitochondrial dysfunctions have been associated with ovarian aging both in animal and human studies. Preliminary works suggest that supplementing CQ-10 may rejuvenate mitochondrial energy store in the granulosa cells and defer ovarian aging.[24] At present, there are only very few clinical trials on the application of CQ-10 in assisted reproduction. Further evidence is required before CQ 10 can be recommended for all low responders.[5]
Recommendation(s): At this time, there is limited evidence in support of antioxidants as adjuvants to improve pregnancy rate in subfertile women undergoing IVF.[23]
Artificial oocyte activation (AOA)
The use of calcium ionophore to artificially induce oocyte activation at the time of fertilisation in an IVF/ ICSI cycle has recently attracted attention.[5] It increases calcium ion concentration around the ooplasm immediately following sperm-oocyte fusion and thereby has been shown to increase fertilisation rates, subsequent to a low or total failed fertilisation in previous ICSI cycle(s).[5] Initial publications on AOA were in forms of case-reports, case series or retrospective analyses showing inconsistent results. Recent RCTs did not find any advantage of calcium ionophore for oocyte activation in women with diminished ovarian reserve[25] or male-factor infertility.[26] A subsequent systematic review concluded that there was insufficient evidence to prove effectiveness of AOA.[27]
Recommendation(s): In the few studies done to date, AOA using calcium ionophores may improve fertilization rates in ICSI cycles, where the oocyte and sperm have failed to activate in previous treatment cycles. However, there are no RCTs to prove effectiveness or safety of this procedure.[2,5]
ADJUVANTS FOR SPERM
Sperm DNA fragmentation tests and anti-oxidants
The sperm DNA fragmentation tests include TUNEL, Comet, SCD assay, SCSA, and 8-OhdG test.[28] There are clear differences between assays in terms of the type of DNA damage being measured and their relative sensitivity.[29] However, no particular assay has yet emerged as being of greater diagnostic value than any other.[6]
The Practice Committee of the ASRM has concluded that “current methods for assessing sperm DNA integrity do not reliably predict treatment outcomes and cannot be recommended routinely for clinical use”.[30] In a recently updated Cochrane review on “Antioxidants for male subfertility” (2019), there was low-quality evidence of significant improvement in live births (OR 4.85;95% CI 1.92–12.24, P = 0.0008) based on seven small RCTS when antioxidants were given to men whose partner was undergoing IVF for male factor infertility.[31] There was no evidence of increased risk of miscarriage, however antioxidants may give more mild gastrointestinal upsets but the evidence is of very low quality. The authors concluded that subfertile couples should be advised that overall, the current evidence is inconclusive based on serious risk of bias due to poor reporting of methods of randomization, failure to report on the clinical outcomes, live birth rate and clinical pregnancy, often unclear or even high attrition, and also imprecision due to often low event rates and small overall sample sizes. Further large well-designed randomized placebo-controlled trials reporting on pregnancy and live births are still required to clarify the exact role of antioxidants.[31]
Recommendation(s): Neither sperm DNA fragmentation tests nor antioxidant therapy is routinely recommended based on current evidence.[2,6,30,31]
Advanced sperm selection techniques
It has been widely recognized that standard semen analysis is a crude assessment of male reproductive potential because it does not evaluate the functional capacity of sperm.[5] Advanced sperm selection methods have been described to improve fertilisation rates, even when ICSI is performed.[5] Fertilisation of oocytes by sperms of high DNA integrity or genetic competence is expected to improve embryo quality and thereby pregnancy outcomes.[5] Advanced sperm selection techniques include sperm surface charge selection, non-apoptotic sperm selection, sperm birefringence, intracytoplasmic morphologically selected sperm injection, (IMSI), physiological intracytoplasmic sperm injection (PICSI) or Hyaluronic acid binding.[5] Of these, only IMSI and PICSI have been assessed through RCTs. Cochrane reviews including two RCTs on PICSI and nine RCTs on IMSI failed to find any improvement in CPRs when these methods are compared with standard ICSI.[32,33]
Intracytoplasmic morphologically selected sperm injection (IMSI). IMSI is a sperm selection technique which involves using a microscope to view sperm under very high magnification (over 6000x). It is a non-invasive test performed on a semen sample as an additional step in the ICSI process. The risk associated with the use of ICSI also apply to IMSI and there are no significant additional risks to the patient or embryo.[2]
There have been several RCTs within the last decade and few systematic reviews suggest the IMSI could be beneficial in specific situations such as previously failed ICSI attempts.[2,32] However, the overall evidence does not support the use of IMSI over standard ICSI for infertile men. One small study found that IMSI has improved pregnancy outcomes in older women, however this study was carried out with a small number of women and the link, if any between IMSI and older eggs is not fully understood.[2]
Physiological intracytoplasmic sperm injection (PICSI). Physiological Intracytoplasmic sperm injection (PICSI) is a technique used to select sperm for use in ICSI treatment. It involves placing sperm with hyaluronic acid (HA), a natural compound in the body. PICSI identifies sperm that can bind to HA and these sperm are selected for use in treatment.[2] It is a non-invasive procedure performed on a semen sample as an additional step in the ICSI process.
There have been a number of studies comparing PICSI with standard ICSI, however there is very little evidence to suggest any benefit of using it. A multi-center RCT that compared PICSI with standard ICSI found a 12% rise in CPRs with PICSI, which is clinically significant.[34] This RCT also found a significant reduction of pregnancy loss in the PICSI group. Evidence on PICSI is still in the formative stage and, with limited experience. No serious additional risk (over ICSI) has been reported yet. A large randomized study[35] was recently carried out which showed that using PICSI did not increase the clinical pregnancy rate.
Recommendation (s): Currently there is not enough evidence to support the routine use of advanced sperm selection techniques over standard ICSI.[2,6]
ADJUVANTS FOR EMBRYOS
Time-lapse (TL) embryo imaging
The usefulness of TL imaging in human IVF has been well debated. Among the proposed benefits that have been put forward are “not missing important events during culture”, quality control, teaching applications, more information to the patient and, an increase in live birth rates (LBR).[6]
Multiple sequential imaging of the dividing embryos without bringing them out of the incubator and analysis of the time interval of certain developmental mile-stones (“morpho-kinetic assessment”) provide more information about their developmental competence, and may predict the clinical outcomes.[5] Time-lapse imaging also limits repeated embryo exposures outside the incubator and thereby may avoid embryo damage due to temperature variation. It has added the advantage of reproducibility and flexibility of laboratory work.[5] At the same time concern is raised on repeated light (ultra-violet ray) exposure while taking the images.[5] This new technology has been tested as a predictor of blastocyst development, implantation success, as well as aneuploidy detection with debatable interpretation.[5] After publication of a series of encouraging studies,[5,36] no difference in LBRs, CPRs and miscarriages could be found in a recent Cochrane review[37] of 2 published RCTs and 1 study presenting interim analysis. The review concluded that there was insufficient evidence to choose between Time-Lapse imaging and conventional morphological assessment.
Recommendation(s): There is not enough evidence to show that time-lapse imaging improves birth rates.[2,6,37]
Embryo glue
The use of fibrin sealants to reduce ectopic pregnancy rate and increase live birth rates was first proposed in 1990 by Feichtinger et al.[6,38] More recently, the focus has shifted to the use of a specific embryo transfer (ET) medium enriched with the glycoprotein hyaluronan.[6] It is well reported that hyaluronic acid (HA) is naturally present in the female reproductive tract and endometrium and forms a viscous solution which could enhance the ET process and prohibit embryo expulsion[39]
The published data surrounding the use of adherence compounds are highly varied in quality and robustness of study design and as a result, the use of HA supplemented media for ET is still regarded as controversial.[39] The Cochrane review of 3898 participants from 17 RCTs demonstrated moderate quality evidence for an improvement in CPR and LBR, with an associated increase in multiple pregnancy rate, when transfer medium was supplemented with HA.[39] The authors concluded that further high-quality studies were required, in particular where an elective single embryo transfer procedure was performed, in part to alleviate concerns over the reported increase in the multiple pregnancy rate. A subsequent RCT by Fancsovits et al.[40] looked at 581 cycles and did not show a benefit in implantation rate, CPR or LBR, but found a higher birth-weight in the HA group.
Recommendation(s): The published evidence may be suggestive of a beneficial effect of the use of HA supplemented ET media. However, further high-quality studies are needed to confirm the effectiveness of embryo glue.[2,6,39]
Assisted hatching (AH)
Cochen et al.[41] proposed that making a breach in the zona pellucida may help implantation in some patients.[6] Assisted hatching (AH) is usually performed on Day 3, 5, or 6 of embryo development using a non-contact laser, but mechanical or acidic solutions have also been used.[6] Clinics use AH for patients of advanced maternal age, smokers or patients with a raised FSH, or when transferring embryos that have been cryopreserved.[6] However, still there is no consensus on its use. Chemical or laser-assisted hatching has been proposed to help a hardened zona break and create channels for exchange of metabolites, growth factors and signals between the embryos and endometrium. AH has not shown to be beneficial in unselected or good prognosis patients.[42] No advantage was observed in women with advanced age either. A systematic review of 28 studies found higher CPRs in the subgroup of patients who had previous IVF failure(s).[42] A Cochrane review of 31[43] RCTs found a significant but marginal improvement in CPRs (OR 1.13, 95% CI 1.01 to 1.27) with AH, but no difference in the LBRs (OR 1.03, 95% CI 0.85 to 1.26). The included studies were significantly heterogeneous. Although higher CPRs have been noted in the sub-group of women who had AH due to previous IVF/ICSI failure, it was concluded that the evidence is insufficient to offer AH in the above group of patients.[43] Both the above meta-analyses identified significantly higher multiple pregnancy rates with the AH technique. A retrospective study of a large data-base (422,949 fresh first ICSI cycles) from the United States found lower LBRs with AH when performed because of diminished ovarian reserve.[44]
Recommendation(s): The National Institute for Clinical Excellence (NICE) guidelines (2013) state that “assisted hatching is not recommended because it has not been shown to improve pregnancy rates”.[45]
Elective “Freeze all” cycle
Elective freeze all cycles involve creating embryos using IVF or ICSI and then freezing all of them so no embryos are transferred in the “fresh” cycle. The embryos are thawed a few months later and transferred to the women’s uterus as part of a frozen embryo transfer (FET) cycle.[2]
Research into freeze all cycles is progressing quickly.[2] Some research suggests that pregnancy rates are increased by using frozen embryo transfers (FETs) rather than fresh transfer, and that the risks to mother and baby are lower.[2] These include the risk of OHSS (above) and of low birth-weight.[2] So far, the study result (trials and meta-analysis) have been inconsistent. In a large multicenter RCT from China,[46] there was improvement in outcome in general IVF patient population. However, in a recent multicenter RCT (460 IVF patients at eight clinics in Denmark, Sweden, and Spain), it was concluded that in normally ovulating patients, there is no apparent benefit from a freeze-all strategy in IVF.[47] There is only sufficient evidence to recommend freeze-all for patients diagnosed with polycystic ovary syndrome. Recommendation(s): There is conflicting evidence at present that whether freeze all cycles are safer and more effective than conventional IVF or ICSI.[2] Further high-quality studies on large number of infertile couples are awaited.
Preimplantation genetic screening (PGS or PGT-A)
Numerical chromosomal abnormalities of either meiotic or mitotic origin in pre implantation embryos have been regarded as the main reason for implantation failure, miscarriage and prolonged time to pregnancy in IVF.[48] It was consequently postulated that selection of euploid embryos for transfer would increase the likelihood of pregnancy and thereby IVF success rates.[48] Although pre implantation genetic testing for aneuploidy (PGT-A), previously known as PGS, has been widely applied at the cleavage state, randomized clinical trials (RCTs) clearly showed that PGT-A did not increase pregnancy rates, and in some instances even lowered them.[49,50] This was later explained by the high rate of mosaicism at cleavage stage embryos and by the failure of the FISH technology to detect all chromosomal abnormalities present.[6,48]
With the advent of new technology allowing comprehensive chromosome screening (CCS) with comparative genomic hybridization (CGH)-array of Day 5 biopsied trophectoderm cells has raised renewed hope in PGS / PGT-A. Biopsy at the blastocyst stage rather than in cleavage stage very much reduces errors due to mosaicism.[6]
A multinational, multicenter, pragmatic, randomized clinical trial with intention-to-treat (ITT) analysis, to estimate the effectiveness of PGT-A in broad routine clinical practice[48] was initiated in 2012 under the name the Evaluation of oocyte Euploidy by Microarray analysis (ESTEEM). However, the much anticipated ESTEEM trial concluded that the preimplantation genetic testing for aneuploidy (by comprehensive chromosome screening of the first and second polar body to select euploid embryos for transfer) does not substantially increase the live birth rate following ICSI in women aged 36 to 40 years.[48]
Recommendation(s): Although some studies may serve to provide evidence supporting PGS, the current RCTs do not provide sufficiently robust evidence to consider PGS / PGT-A as an effective adjuvant therapy to improve pregnancy rates.[2]
Autologous endometrial co-culture
Since the early days of embryo culture in vitro, various modifications to the culture system have been explored in an attempt to optimize embryo development.[51] Research studies have been conducted using either cumulus cells or endometrial cells for co-culture. Autologous cumulus cells are routinely available in IVF cycles and have been studied both with mature[52] and immature oocytes[53] for co-culture. However, the studies are small, heterogenous and experimental at this stage.
Autologous endometrial co-culture (AECC) has been investigated, including a large study reported by Spandorfer et al.[54], in 1,030 consecutive cycles of in vitro fertilization-embryo transfer. Embryos were randomly grown on endometrial co-culture or conventional media. The study results demonstrated a significant improvement in embryo quality with endometrial co-culture. Endometrial cell co-culture was also reported to benefit a cohort of patients with repeated implantation failure.[55] A subsequent retrospective study indicated that patients with various forms of infertility had significantly improved blastocyst formation (56.0% vs 45.9%), pregnancy (39.1% vs 27.5%), and implantation (33.3% vs 20.9%) with endometrial co-culture compared with a sequential culture media.[56]
Recommendation(s): Further RCTs are needed to establish the effectiveness and safety of endometrial co-culture.[54,55]
Adjuvants for endometrium/implantation
Estrogen. Estrogen has been used as an adjuvant for follicular priming and endometrial development in women undergoing IVF cycles.[8] One rationale for the use of estrogen priming before the commencement of ovarian stimulation is that this may synchronize antral follicle development allowing for the use of reduced gonadotropin dosage in high responders and improved follicle numbers in poor responders.[8] However, there is lack of evidence for the use of estrogen priming or the combined oral contraceptive pill (COCP) in IVF cycles.[57] A Cochrane review[58] evaluated the effect of the COCP, estrogen only and progesterone only supplementation in IVF cycles on pregnancy outcomes and the incidence of OHSS. Twenty-three studies involving a total of 2596 subjects were included. The studies were heterogeneous in design and outcome measures, and the authors concluded that there was insufficient evidence to comment on the primary outcome measure of live birth rates for any of the interventions and too little data to understand any effect on OHSS.
The role of estrogen in the luteal phase for the preparation of a favorable endometrium is also unclear. Earlier studies showed that a drop in estradiol and progesterone levels in the luteal phase of IVF cycles was associated with reduced pregnancy and implantation rates.[59] Subsequently, some investigators reported that luteal phase support with estradiol and progesterone was associated with higher pregnancy rates per embryo transfer[60]; however, others failed to observe any beneficial effects.[61]
The Cochrane meta-analysis[62] reported no difference in live birth/ongoing pregnancy rate (9 RCT, OR 1.12, 95% CI 0.91–1.38, 1651 women) or OHSS (2 RCT, OR 0.58, 95% CI 0.20–1.68, 461 women) between progesterone with estradiol supplementation and progesterone alone.[62]
Recommendation(s): Follicular priming with estrogen or the COCP cannot be recommended as an adjuvant in IVF cycles. In addition, available evidence does not recommend routine estradiol supplementation for endometrial development in the luteal phase support of fresh IVF cycles.[8]
Aspirin. Acetylsalicylic acid (Aspirin) is a non-steroidal anti-inflammatory agent that works by inhibition of cyclooxygenase enzyme in platelets and reduction of prostaglandin synthesis.[8] The research studies observed that daily administration of aspirin caused a shift from thromboxane A2 to prostacyclin, thereby leading to vasodilation and increased peripheral blood flow.[8] Aspirin also increases uterine blood flow[63] that in turn may enhance endometrial receptivity and improve implantation rates.
Although use of aspirin has a beneficial effect in women with Anti-phospholipid (APL) syndrome and recurrent miscarriage and in prevention of pre-eclampsia, the evidence supporting its use in women undergoing IVF cycles is controversial.[8] Various studies and seven meta-analysis[64,65,66] have provided conflicting evidence.[8] A Cochrane review (Siristatidis et al. 2011) concluded that the use of aspirin in IVF does not improve pregnancy rates.[64] A subsequent meta-analysis of 268 pregnancies from four studies showed that pre-conception administration of low-dose aspirin in IVF patients does not confer benefits in sustaining pregnancy.[65]
Recommendation(s): There is lack of proven efficacy for routine use of aspirin as an adjuvant in IVF cycles.[8,64,65]
Heparin. Both unfractionated and low molecular weight heparin (LMWH) with or without low-dose aspirin have been used to promote successful invasion of trophoblasts in the presence of antiphospholipid syndrome. Few research groups found that thrombophilia is more common in women with repeated implantation failure compared with that in healthy fertile controls.[8] Heparin is a poly-sulphated glycosaminoglycan that interacts with positively charged amino acids. LMWH is the depolymerised form of unfractionated heparin with similar action but increased bioavailability and half-life. Heparin exerts its anti-thrombotic effect by inhibition of factor Xa and thrombin.[8]
Some studies[67,68] showed that unfractionated heparin and low-dose aspirin do not improve pregnancy rates, whereas others demonstrated a significant improvement in pregnancy rates in women with thrombophilia receiving heparin treatment with or without low-dose aspirin.[69,70,71] The evidence on the effectiveness of combined heparin and aspirin therapy is conflicting and not without risks such as bleeding and thrombocytopenia.[5]
There is emerging evidence that heparin modulates endometrial receptivity and decidualization of endometrial stromal cells, and improves implantation.[8] It is postulated that these effects are exerted by various mechanisms including inhibition of production of insulin-like growth-factor binding protein (IGF-BP), regulation of heparin-binding epidermal growth factor (hb-EGF), reduction in expression of adhesion molecules such as, E-cadherin which promotes trophoblastic invasion and blockage of complement activation and modulation of inflammatory responses. Further, research using adequately powered RCTs is required to confirm or refute the beneficial effect of Heparin.[8]
Recommendations(s): Evidence for the efficacy of LMWH is weak such that its routine use in the wide population of women undergoing IVF treatment is not warranted. However, it should be carefully considered in women with thrombophilia.[5,8]
Vasodilators. Several pharmacological agents classed as vasodilators have been tried in IVF cycles with an objective to improve endometrial blood flow and thereby improve implantation rates.
Nitroglycerine (NTG) is a Nitric oxide (NO) donor, and has been investigated in a RCT which assessed its efficacy in inducing uterine vasodilation and thereby endometrial receptivity.[72] A total of 138 women with good-quality embryos were randomised the day before embryo transfer into receiving a 5-mg NTG patch, or placebo, daily until pregnancy test. The RCT did not find improvement in implantation rates, CPRs or uterine artery indices between the NTG and placebo groups.[72]
Sildenafil Citrate is a vasodilator with potential to increase uterine and endometrial blood flow and thus increase endometrial thickness. It has been used empirically (25 mg qid vaginally from stimulation Day 1 to HCG day)[73] to improve endometrial thickness in women undergoing IVF treatment. It is a type-5 phosphodiesterase inhibitor that prevents breakdown of c-GMP and potentiates the effect of NO on vascular smooth muscle. Studies on the role of sildenafil in improving endometrial thickness reported conflicting results.[73]. In a prospective study[74] of 61 patients with a thin endometrium (8mm) and high uterine radial artery resistance index (RA-RI) it was found that sildenafil improved RA-RI in 12 patients and endometrial thickness in 11 of those 12 patients. By contrast, Check and colleagues (2004) failed to demonstrate an increase in endometrial thickness or blood flow following addition of sildenafil to an estrogen supplemented regime in women undergoing fresh IVF or frozen embryo transfer.[75]
L-arginine is an essential amino acid that plays a crucial role in multiple physiological functions, such as regulating vasodilation and vascular flow, activating the immune system and the inflammatory process. Takasaki et al.[74] evaluated the impact of arginine on nine women with a recurrent thin endometrium at doses of 6 mg/day. They described an increased vascular flow of the radial uterine arteries in 89% of their patients and endometrial growth >8 mm in 67%. However, solid data are still lacking to validate the usefulness of L-arginine in improving live births / clinical pregnancy rate.
Recommendation(s): Current evidence does not support any significant beneficial effects of vasodilators on IVF outcome, and their routine use as adjuvants in IVF cycles is not recommended.[5,8]
Uterine relaxants. At the time of IVF uterine activity is increased compared with that in natural cycle conception.[76] This adverse uterine activity at the time of embryo transfer can occur as a result of a number of factors, including early timing of transfer in the luteal phase, mechanical stimulation and supra-physiological hormonal milieu.[77] It has been suggested that embryo transfer being an invasive procedure, may induce endometrial inflammatory reaction and augmented myometrial contractility.[78] In an attempt to optimise IVF success rates, different investigators tried using uterine smooth muscle relaxants.
Nitroglycerine. NTG is a NO donor and along with its vasodilatation action, it relaxes the uterine smooth muscle. No difference has been observed with its use 3 min before embryo transfer in the ease of transfer or the pregnancy rates.[79]
β2–Adrenergic antagonists. Selective β2-adrenergic blockers (Ritodrine, Terbutaline and Salbutamol) are known uterine smooth muscle relaxants. In a study by Pinheiro et al.[80] administration of these agents for two weeks following oocyte retrieval failed to improve implantation and pregnancy rates, whilst causing adverse effects such as hypotension and tachycardia.
Piroxicam. Uterine contractions are induced by prostaglandin which is synthesized from arachidonic acid by cyclo-oxygenase (COX).[81] Piroxicam is an NSAID which has been used before embryo transfer (10 mg dose orally 30 minutes to 2 hours before embryo transfer) in various studies with controversial results. Its mechanism of action is not completely understood, but may be related to prevention of prostaglandin synthesis by a reversible inhibition of the cyclooxygenase enzyme.[82]
While few studies found pregnancy rate to be higher after using Piroxicam, others did not observe any benefit.[78,81,82] Sohrabvand[81] concluded that Piroxicam administration 30 minutes prior to embryo transfer can prevent or reduce uterine cramps after the procedure, but it cannot increase pregnancy rates.
Atosiban. Atosiban is a receptor antagonist for vasopressin V1a and oxytocin. It selectively acts on the uterus to suppress uterine contractions and was initially used solely to prevent premature delivery.[83] Pierzynski et al.[84] were the first to apply atosiban in IVF–ET in a clinical setting. The impact of atosiban on pregnancy outcomes in women undergoing IVF has been investigated in recent years, however the findings failed to reach a consensus.[83] In a meta-analysis by Qian-Yi Huang et al.[83] it was concluded that “Atosiban may be more appropriate for women undergoing recurrent implantation failure (RIF) and play only a limited role in improving pregnancy outcomes in the general population of women undergoing IVF. These conclusions should be verified in large and well-designed studies”.
Recommendation (s): There is insufficient evidence to support the use of uterine relaxant agents around the time of embryo transfer in routine clinical practice.[8,85]
Endometrial scratching/injury (EI). Endometrial scratching is a simplified version of endometrial curettage, usually performed with a soft plastic Pipelle cannula during luteal phase of cycle prior to IVF cycle.
For the past decade or more, there has been a steady increase in the use of endometrial scratching so much so that in 2015, 83% of clinicians from the United Kingdom, Australia, and New Zealand were recommending it.[86,87] Yet, there has never been a satisfactory explanation of the mechanism of action underpinning any improvement in implantation[88] or high quality evidence of benefit.[89]
The first study suggesting a therapeutic effect from endometrial scratching was published in 2003, and the first randomized controlled trial was published in 2008.[87] When the Cochrane review was published in 2015,[88] the authors concluded, “Although current evidence suggests some benefit of endometrial injury, we need evidence from well-designed trials that avoid instrumentation of the uterus in the preceding three months, do not cause endometrial damage in the control group, stratify the results for women with and without recurrent implantation failure and report live birth”.[88] In February 2019, a randomized controlled trial of endometrial scratching in 1,364 women having an IVF cycle was published in the New England Journal of Medicine.[90] Results showed that clinical pregnancy rate in the endometrial scratch group was 31.4% and in the control group 31.2%. The live-birth rate was the same in each arm: 26.1% for the scratch group and 26.1% for the control group. There was also enough power to rule out an effect for women with two or more implantation failures in a planned subgroup analysis. This study also reported that only 5% did not experience any pain at all and 3% of women had significant bleeding.[87]
In a recent review by van Hoogenhuijze et al.,[91] the authors searched the effect of endometrial scratching in patients with or without prior failed ART cycles on live birth (LBR) and clinical pregnancy rates (CPR). Fourteen RCTs involving 2537 participants were included.. Results of pooled analysis showed no significant difference for LBR, but CPR was significantly improved after endometrial scratching. The authors concluded that it remains unclear if endometrial scratching improves the chance of pregnancy for women undergoing ART and, if so, for whom.
Recommendation(s): At present there is conflicting body of evidence. Endometrial scratching should not be offered in daily practice until results from large and well-designed RCTs and an individual patient data analysis become available.[87,88,90]
Reproductive immunology testing and treatment. Maternal immune modulation in the peri-implantation window has been postulated to play an important role in acceptance of the embryo as a semi-allograft 5. Natural Killer (NK) cells, cytokines, growth factors, tissue necrosis factor- α (TNF- α), macrophages and a balance between T-helper 1 (Th-1) and T-helper 2 (Th-2) cells play an important role in the implantation process.[5] Couples seeking a reason for IVF failure find the rationale of immune rejection very appealing.[5] A plethora of expensive tests are available to identify such immune dysfunctions, including peripheral blood NK (pNK) cell number and activity and uterine NK (uNK) cell number and activity. However, there is no consensus on what constitutes a definitive normal range for either of these tests although < 12% to < 16% pNK cells and < 5% to < 13.8% uNK cells are considered to be normal values in various studies.[5]
The evidence for an association between elevated NK cell levels and implantation failure comes from retrospective and observational studies, which have yielded conflicting results.[5] A systematic review found no significant difference in the pNK cell number and activity in women with or without implantation failure (OR 1.35, 95% CI 0.28–6.46) or miscarriage after ART (OR 2.48, 95% CI 0.50–12.32) and thus concluded that routine testing for pNK cells is of uncertain prognostic significance.[92,5]
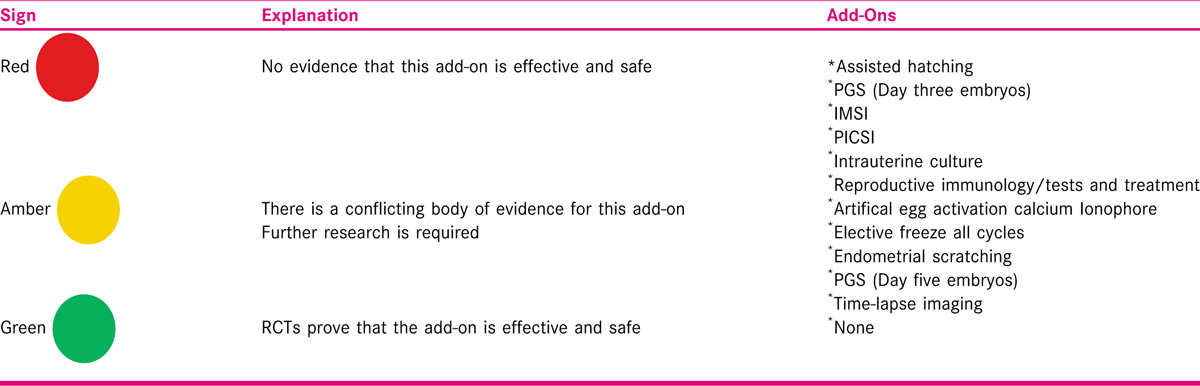
Various strategies have been proposed to reduce the pNK cell levels including intravenous immunoglobulins (IVIG), TNF-α inhibitors, granulocyte-colony stimulating factor, lymphocyte immune therapy, leukaemia inhibitory factor, peripheral blood mononuclear cells, intralipids, glucocorticoids and vitamin D supplementation.[5] However, HFEA 2019[2,3] recommends that not only reproductive immunology treatments do not improve pregnancy chances, there are risks attached to these treatment, some of which are very serious. Zemyarska[4] summarized the cost and health risks of five adjuvants used for reproductive immunology treatment [Table 1].[4]

Intravenous immunoglobulin (IVIG). IVIG has been used for the treatment of recurrent implantation failure after IVF either empirically or for patients in whom immunological testing has shown increased number of peripheral natural killer (NK) cells or cytotoxicity, abnormal T helper (Th)1:Th2 ratio, positive anti-thyroid antibody or anti-phospholipid antibody (APL) test, or increased TNF- α level or human leukocyte antigen (HLA) antigens similarity, in the hope of improving IVF outcomes.[8,93,94,95]
The proposed mechanisms of action of IVIG include inhibiting NK cell production and/or activity, correcting abnormal Th1:Th2 ratio and non-specific immunomodulation leading to enhancement of immunological tolerance.[8]
In a review by Li et al.,[8,96] they included 10 studies published between 1994 and 2012, in which 1,477 women received IVIG as adjuvant therapy during their IVF treatment. The authors reported that the use of IVIG was associated with a significantly higher implantation rate (RR 2.708, confidence interval 95%CI: 1.302–5.629), clinical pregnancy rate (RR 1.463, 95%CI:1.075–1.991) and live birth rate (RR 1.616, 95%CI: 1.243–2.101), and a significantly lower miscarriage rate (RR 0.352, 95%CI: 0.168–0.738). However, most of the studies included were retrospective, poorly designed, clinically heterogeneous and had a number of methodological flaws that could introduce bias.[8] Apart from the lack of randomization, the studies included a mixture of patients with recurrent implantation failure, unexplained infertility and recurrent miscarriage, used multiple adjuvant interventions and a variety of IVIG doses and regimes, and compared their results with historical controls.[8,96] In addition, cost effective analysis was not part of any of these studies.[8]
It is also important to emphasize that IVIG is a pooled blood product and therefore its use carries the potential risks of anaphylaxis and infection.[8,97] IVIG is also associated with other complications in up to 35% of cases.[8,98] Majority of such side effects are mild and transient, including itching, headache, flushing, low backache, nausea, fatigue and skin reaction, and are often related to the rate of infusion, total dose and brand of IVIG infused. Serious side effects such as aseptic meningitis, severe anaphylactic reaction, acute renal failure and thrombotic events are rare.[8,99]
Recommendation (s): There is no convincing evidence for the use and safety of IVIG as adjuvant in women with recurrent implantation failure embarking on IVF.[2,8]
Corticosteroids. Corticosteroids have anti-inflammatory and immune-suppressive activity and hence it has been postulated that it might improve the intrauterine environment by reducing endometrial pro- inflammatory cytokines production and NK cell activity.[8] The use of corticosteroids in women known to have an abnormal immunological test, such as elevated NK cells or presence of auto-antibodies including ACA, anti-thyroid, ANA and anti-ovarian antibodies, has also been examined.[8]
A Cochrane review[100] investigated whether empirical use of corticosteroids in women undergoing IVF or ICSI, could improve treatment outcomes. Fourteen studies involving a total of 1879 couples were included. Pooling of the results showed no evidence that corticosteroids improved the clinical pregnancy rate odds ratio (OR: 1.16, 95%CI: 0.94–1.44) or live birth rate (OR: 1.21, 95%CI: 0.67–2.19).
The British Fertility Society Policy and Practice Committee report (2015) concluded that there is a lack of robust evidence to support the routine use of corticosteroids empirically as an adjuvant in IVF cycles. There is limited evidence that corticosteroids may improve pregnancy rates in women undergoing conventional IVF and in the subgroup of women with auto-immunity or unexplained implantation failure.[8]
Recommendation(s): There no convincing evidence to support the routine use of corticosteroids empirically as an adjuvant in ART cycles.[8,100]
Intravenous lipids. It has been suggested that 20% intravenous lipid solution can improve implantation in women with repeated implantation failure and raised Th1 response.[8] Intravenous lipid therapy contains glycerin, soybean oil and egg phospholipids. Whilst the precise immune-modulatory mechanism of action remains unknown, it is postulated that intralipids inhibit pro-inflammatory factors such as Th1 cytokines and that the fatty acids work as ligands to activate peroxisome proliferator activated receptors expressed by the NK cells, which in turn reduces the cytotoxic effects of NK cells.[8] It reduces Th1/Th2 ratio and suppresses abnormal NK cytotoxicity, thus enhancing the likelihood of implantation and clinical pregnancy.
Singh et al.[101] showed a statistically significant increase in implantation rate and live birth rate in women who received intravenous intralipid with prior implantation failure after IVF/ ICSI. The dosage used in the study was 4 ml in 250 ml normal saline over 30–60 min intravenous infusion during fresh cycle, on day of oocyte pickup (after retrieval). The infusion was repeated within one week of positive pregnancy test and then every two weeks until the end of the first trimester.[101] However, there been no randomized controlled studies to prove the effectiveness of intralipid therapy in improving IVF success rates.
Recommendation(s): At present, there is lack of strong evidence to recommend intralipid infusion therapy as an adjuvant in IVF cycles.[8]
Anti-tumor necrosis factor-α (TNF-α) agents. An exaggerated Th1 response is thought to be detrimental to the process of implantation and has been linked to infertility.[8] TNF- α is a pro-inflammatory Th1 cytokine implicated in endometriosis-related infertility and IVF failure.[8] The potential reproductive benefit of anti −TNF- α agents [Adalimumab (Humira), Entanercept (Enbrel) and Infliximab (Remicaid)] has been studied in infertile patients with a raised Th1:Th2 cytokine ratio.[8,102,103,104]
A small retrospective case-control study of women with Th1:Th2 cytokine elevation reported a live birth rate of 73% in 41 patients who received IVIG and Adalimumab; 50% in 6 patients who received Adalimumab alone and no live birth in 5 patients who received neither.[95]
Side effects can include infection, lymphoma, demyelinating disease, autoantibody induction, congestive heart failure, injection site reactions and lupus-like syndrome.[4]
Recommendation(s): There is a lack of evidence to support the effectiveness and safety of using anti- TNF- agents as adjuvant in IVF cycles.[8]
Granulocyte colony-stimulating factor (G-CSF). G-CSF, initially described as a hematopoietic growth factor, has been shown to have important functions in non-hematopoietic cells, including the endometrium.
Gleicher et al.[105] hypothesized that G-CSF might have a direct role in promoting endometrial growth, and reported a case series of four patients with thin endometria between 3 and 6.5 mm who failed to improve with oral and vaginal estrogen as well as with vaginal sildenafil (in one of the patients). All four patients had intrauterine G-CSF infusion (300 mcg) 2–9 days before ET, and had a significant increase to at least 7 mm within 48 h. All four patients conceived, one of which had an ectopic. Two years later, the same group[106] performed a prospective pilot cohort study of 21 patients. Overall, endometrium thickness increased from an average of 6.4 ±1.4 mm to 9.3 ±2.1 mm (P <0.001) after G-CSF treatment, but did not differ between those who conceived and those who did not. The overall clinical pregnancy rate in the cohort was 19.1%.
Since then, there have been controversial results with Kunicki et al.[107] and Barad et al.[108] reporting no difference in clinical pregnancy rates within the G-CSF and control groups, and Li et al.[109] and Xu et al.[110] reporting better clinical pregnancy rates with G-CSF treatment.
Recommendation(s): Although case series and non-randomized studies are encouraging but RCTs have failed to confirm benefit on clinical outcome. The best available evidence on hypothetical beneficial effect of G-CSF enhancing endometrial receptivity is not very supportive.[111]
Autologous platelet-rich plasma. Platelet-rich plasma (PRP) collected from a peripheral vein, through activating platelets by clotting, releases cytokines and growth factors, including VEGF, transforming growth factor, platelet-derived growth factor and epidermal growth factor.[111] It has been used in other therapeutic areas of medicine to improve tissue regeneration.[111] More recently evidences[112,113,114] have shown its positive effects in promoting endometrial and follicular growth and gestation in assisted reproduction cycles.
Despite its widespread uses in medicine, the mechanisms through which PRP exerts its regenerative effects are only postulated, not based on scientific data.[112] There is an unmet need for advanced research to corroborate present findings in the clinical scenario.
Recommendation(s): Further evidence on the molecular basis of PRP treatment and well-designed RCTs are necessary to obtain solid evidence. Till that time PRP is experimental.[112,113,114]
Intrauterine hCG administration. Human chorionic gonadotropin (hCG) is the key molecule to initiate the communication between the embryo and the endometrium, contributes to maternal tolerance of the embryo through interactions with immune cells within the receptive endometrium and plausibly in systemic circulation.[115] A Cochrane review including 12 RCTs of 4038 women analyzed the efficacy of the intrauterine administration of hCG in ART.[116] The study, which also suffered from a considerable degree of heterogeneity, reported an increase in clinical pregnancy (RR 1.41, 95% CI 1.25 to 1.58) and live birth rates (RR: 1.57, 95% CI 1.32 to 1.87) in the subgroup of women having cleavage-stage embryo transfers with intrauterine hCG administration compared with women with no hCG treatment.[115,116] However, they concluded that the current evidence for intrauterine hCG treatment does not support its use in ART cycles due to the small size and the variable quality of the trials and the fact that positive findings were extracted from a subgroup analysis. The other systematic review and meta-analysis on the subject analyzed eight RCTs that included 3087 women and found no difference in the live birth (RR 1.13; 95% CI 0.84 to 1.53) and spontaneous abortion rates (RR 1.00, 95% CI 0.74 to 1.34) in women who received intrauterine hCG and those who did not.[115,117]
A more recent meta-analysis[118] analyzed six RCTs to evaluate the effects of intrauterine hCG administration before fresh embryo transfer and found no-significant difference in clinical pregnancy (RR 1.11), implantation (RR 1.17), miscarriage (RR 0.91), ectopic (RR 1.65) or live birth rates (RR 1.13) between the hCG groups and control group.
Recommendation(s): The current evidence for intrauterine injection of hCG before fresh ET does not support its use in an assisted reproduction cycle.[118]
Intrauterine peripheral blood mononuclear cell (PBMC). In 2006, researchers reported that women with recurrent implantation failure (RIF) who received intrauterine peripheral blood mononuclear cells (PBMCs) cultured with human chorionic gonadotropin (hCG) experienced increase in implantation rates.[115,119] PBMCs are defined as any blood cell with a round nucleus, such as B and T lymphocytes, monocytes or macrophages.[115,120]
Various mechanisms have been proposed to explain the implantation-promoting effects of PBMCs. PBMC treatment induces the production of several cytokines, such as IL-1α, IL-1ß, and TNF- α, which can have positive impacts on endometrial receptivity and actively contribute to blastocyst attachment and invasion.[115,120] Further, hCG activates PBMC in vitro and promotes trophoblastic invasion through enhancement of LIF and IL-1 ß secretion.[115] PBMCs cultured with hCG might modulate the implantation site and infiltrate into endometrial stroma, serving as a guide for the invading blastocyst[115].
A recent systematic review and meta-analysis by Yakin K et al.[115] summarized the current evidence regarding the intrauterine administration of PBMCs in cases with RIF. The results from the included studies demonstrated that intrauterine administration of PBMCs with or without hCG culture fails to improve live birth rates when compared to controls. However, PBMCs were associated with an improvement in clinical pregnancy rates, which was more prominent in women with ≥3 failures.[115]
Based on the results of this meta-analysis, there is limited evidence suggesting that intrauterine administration of PBMCs with or without hCG culture improves LBRs in women with RIF. However, the reliability of the data is limited by the observational nature of the available studies. Furthermore, there is a lack of long-term safety data of PBMC administration that is needed.
Recommendation(s): Whether intrauterine PBMC administration significantly improves live birth and miscarriage rates requires further investigations.[115]
ALTERNATIVE THERAPIES AS ADJUVANTS TO IVF
Acupuncture
Acupuncture has become a frequently used adjunctive treatment prior to and during IVF treatment.[121] In the USA, 30% of a patient cohort engaged in acupuncture prior to IVF treatment and 47% during IVF treatment.[121] Acupuncture involves needle insertion and manipulation into specifically chosen acupuncture points located in the subcutaneous tissue. Early trials indicated that a short course of acupuncture administered prior to and immediately following embryo transfer (embryo transfer) may provide benefits in improving reproductive outcomes.[122,123]
A recent systematic review and meta-analysis[124] has examined the efficacy, effectiveness and safety of acupuncture as an adjunct to embryo transfer compared with controls to improve reproductive outcomes. The primary outcome was clinical pregnancy. Twenty trials and 5130 women were included in the review. The meta-analysis found increased pregnancies (risk ratio [RR] 1.32, 95% confidence interval [CI] 1.07–1.62, 12 trials, 2230 women), live births (RR 1.30, 95% CI 1.00–1.68, 9 trials, 1980 women) and reduced miscarriage (RR 1.43, 95% CI 1.03–1.98, 10 trials, 2042 women) when acupuncture was compared with no adjunctive control. There was significant heterogeneity, but no significant differences between acupuncture and sham controls. The findings suggest acupuncture may be effective when compared with no adjunctive treatment with increased clinical pregnancies, but is not an efficacious treatment when compared with sham controls, although non-specific effects may be active in both acupuncture and sham controls.
Recommendation(s): Future research examining the effects of acupuncture for women with poor IVF outcomes is warranted.[124]
Yoga
Stress can be a contributor to infertility and can adversely affect the treatment success.[125] Yoga has been found to be effective in treating anxiety and depression, reducing stress and improving the overall quality of life in the general population.[126] The relationship between stress and infertility remains a subject of controversy. Women undergoing infertility treatments exhibit high anxiety and/or high depressive scores at the start of treatment as well as over the course of treatment.[127] Stress may also have a negative impact on pregnancy rates in women undergoing IVF.[127] Only few studies are available on the effect of stress-management programs in IVF patients. Owing to the diversity of conditions treated, the poor quality of most studies, and the different assessment tools used to evaluate the psychological state, it is difficult to draw definite conclusions.[126]
In a prospective RCT at Boston IVF, the women who were randomized to a mind/body program before starting their first IVF cycle were found to have higher pregnancy rates (52%) then for the control group (20%).[127] In a literature review by Darbandi et al.[128] it was concluded that Yoga can help couples overcome infertility and increase the ART success rate by improving the physiological and psychological states of both men and women. In a RCT by Nayar et al.[129] the clinical pregnancy rate was significantly better in group A women (N=52) who attended three months of Yoga sessions involving asana (exercises) and pranayama (regulated breathing) before undergoing frozen embryo transfer than group B women (N=53) who underwent frozen embryo transfer without Yoga therapy.
Recommendation(s): Yoga has been used as a stress reliever in several areas of health care. However, there is lack of robust good quality evidence to draw conclusions.[126] Further well designed randomized clinical studies in larger population are needed to confirm the effectiveness of Yoga as adjuvant to improve pregnancy rates in couples undergoing ART.
CONCLUSION
The Human Fertilisation and Embryology Authority (HFEA) has rated 11 adjuvant laboratory and clinical procedures (“add-ons”) using a traffic light system.[2] The green rating is reserved for procedures or techniques that have been shown to be effective and safe by at least one good-quality, randomized clinical trial. None of the 11 treatments have received a green rating [Table 2].[130]
The HFEA and 10 leading professional and patient fertility groups in UK agreed a consensus statement after growing concern that patients are being frequently offered, and charged for optional extras to their treatment which claim to improve their chances of having a healthy baby.[1,3] The statement says: “Offered responsibly, they can be a sign of healthy innovation in the fertility sector. However, there is currently no conclusive evidence that any of the add-ons increase the chance of a pregnancy or live birth.”[1,3]
In the absence of any convincing evidence, any adjuvant therapy should be offered only after fully informed consent of the patients based on up-to-date scientific information, and only if there is potential for cost-effective, physiological and psychological benefit and a minimum risk of harm. Clinicians should be fully aware of the best available current evidence and patients must be informed about the experimental nature of any adjuvant therapy being offered to them, when there is no robust evidence of its safety and/or effectiveness.[1,2,3] Further, research in the form of good quality preferably RCTs on a large number of patients is required to establish true effectiveness and safety of various adjuvant therapies.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Wise Jacqui. Show patients evidence for treatment “add-ons, ” fertility clinics are told. BMJ. 2019;364:l226. doi: 10.1136/bmj.l226.
- [Google Scholar]
- Treatment add-ons. www.hfea.gov.uk/treatments/explore-all-treatments/treatment-add-ons
- 2019. The responsible use of treatment add-ons in fertility services: a consensus statement. www.hfea.gov.uk/media/2792/treatment-add-ons-consensus-statement-final.pdf
- Is it ethical to provide IVF add-ons when there is no evidence of a benefit if the patient requests it? J Med Ethics. 2019;45:346-50. Doi: 10.1136/medethics- 2018-104983.
- [Google Scholar]
- Adjuncts in the IVF laboratory: where is the evidence for ‘add-on’ interventions? Hum Reprod. 2017;32:485-91. Doi: 10.1093/humrep/dex004
- [Google Scholar]
- Effect of androgen supplementation or modulation on ovarian stimulation outcome in poor responders: a meta-analysis. Reproductive Biomedicine Online. 2011;22:545-55.
- [Google Scholar]
- British Fertility Society Policy and Practice Committee: Adjuvants in IVF: evidence for good clinical practice. Human Fertility. 2015;18:2-15. DOI: 10.3109/14647273.2015.985454.
- [Google Scholar]
- Androgens (dehydroepiandrosterone or testosterone) for women undergoing assisted reproduction. Cochrane Database Syst Rev. 2015;11:CD009749.
- [Google Scholar]
- The effect of transdermal testosterone gel pretreatment on controlled ovarian stimulation and IVF outcome in low responders. Fertil Steril. 2011;95:679-83.
- [Google Scholar]
- Effect of pretreatment with transdermal testosterone on poor ovarian responder undergoing IVF/ICSI: a meta-analysis. Experimental and Therapeutic Medicine. 2014;8:187-94.
- [Google Scholar]
- Does growth hormone-releasing factor assist follicular development in poor responder patients undergoing ovarian stimulation for in-vitro fertilization? Human Reproduction. 1999;14:1939-43.
- [Google Scholar]
- Growth hormone co-treatment within a GnRH agonist long protocol in patients with poor ovarian response: a prospective, randomized, clinical trial. Journal of Assisted Reproduction and Genetics. 2008;25:123-27.
- [Google Scholar]
- Low-dose growth hormone supplementation increases clinical pregnancy rate in poor responders undergoing in vitro fertilisation. Gynecol Endocrinol. 2015;31:565-68.
- [Google Scholar]
- Growth hormone for in vitro fertilization. Cochrane Database Syst Rev 2010:CD000099.
- [Google Scholar]
- Adjuvant growth hormone therapy in antagonist protocol in poor responders undergoing assisted reproductive technology. Archives of Gynecology and Obstetrics. 2013;287:1017-21.
- [Google Scholar]
- The use of metformin for women with PCOS undergoing IVF treatment. Human Reproduction. 2006;21:1416-25.
- [Google Scholar]
- Metformin treatment before and during IVF or ICSI in women with polycystic ovary syndrome. Cochrane Database of Systematic Reviews. 2009;2:CD006105.
- [Google Scholar]
- Effect of preconceptional metformin on abortion risk in polycystic ovary syndrome: a systematic review and meta-analysis of randomized controlled trials. Fertility & Sterility. 2009;92:1646-58.
- [Google Scholar]
- A meta-analysis of pregnancy outcomes in women with polycystic ovary syndrome. Human Reproduction Update. 2006;12:673-83.
- [Google Scholar]
- Metformin versus placebo from first trimester to delivery in polycystic ovary syndrome: a randomized, controlled multicenter study. Journal of Clinical Endocrinology & Metabolism. 2010;95:448-55.
- [Google Scholar]
- Oxidative stress and antioxidants: exposure and impact on female fertility. Human Reproduction Update. 2008;14:345-57.
- [Google Scholar]
- Antioxidants for female subfertility. Cochrane Database of Systematic Reviews 2017 Art. No.: CD007807 DOI: 10.1002/14651858.CD007807.pub3.
- [Google Scholar]
- Coenzyme Q10 restores oocyte mitochondrial function and fertility during reproductive aging. Aging Cell. 2015;14:887-95.
- [Google Scholar]
- Can calcium ionophore “use” in patients with diminished ovarian reserve increase fertilization and pregnancy rates? A randomized, controlled study. Fertil Steril. 2015;104:1168-74.
- [Google Scholar]
- Effect of oocyte activation with calcium ionophore on ICSI outcomes in teratospermia: a randomized clinical trial. Iran J Reprod Med. 2013;11:875-82.
- [Google Scholar]
- Artificial oocyte activation to improve reproductive outcomes in women with previous fertilization failure: a systematic review and metaanalysis of RCTs. Hum Reprod. 2015;30:1831-41.
- [Google Scholar]
- Sperm DNA integrity assays: diagnostic and prognostic challenges and implications in management of infertility. J Assist Reprod Genet. 2011;28:1073-85.
- [Google Scholar]
- The presence of a truncated base excision repair pathway in human spermatozoa that is mediated by OGG1. J Cell Sci. 2013;126:1488-97.
- [Google Scholar]
- The clinical utility of sperm DNA integrity testing: a guideline. Practice Committee of the American Society for Reproductive Medicine. Erratum Fertil Steril. 2014;101:884.
- [Google Scholar]
- Antioxidants for male subfertility. Cochrane Database of Systematic Reviews 2019:CD007411. Art. No.
- [Google Scholar]
- Regular (ICSI) versus ultra-high magnification (IMSI) sperm selection for assisted reproduction. Cochrane Database Syst Rev. 2013;7:CD010167.
- [Google Scholar]
- Advanced sperm selection technique for assisted reproduction. Cochrane Database Syst Rev. 2014;10:CD010461.
- [Google Scholar]
- Use of hyaluronan in the selection of sperm for Intracytoplasmic sperm injection (ICSI): significant improvement in clinical outcomes −multicenter, double-blinded and randomized controlled trial. Hum Reprod. 2013;28:306-14.
- [Google Scholar]
- Sperm selection for assisted reproduction by prior hyaluronan binding: the HAB select RCT. Gene Pharma.com 2019
- [Google Scholar]
- Selection of competent blastocysts for transfer by combining time-lapse monitoring and array CGH testing for patients undergoing intracytoplasmic genetic screening: a prospective study with sibling oocytes. BMC Med Genomics. 2014;7:38.
- [Google Scholar]
- Time-lapse systems for embryo incubation and assessment in assisted reproduction. Cochrane Database Syst Rev. 2015;2:CD011320.
- [Google Scholar]
- The use of two-component fibrin sealant for embryo transfer. Fertil Steril. 1990;54:733-4.
- [Google Scholar]
- Adherence compounds in embryo transfer media for assisted reproductive technologies. Cochrane Database Syst Rev 2014:CD007421. DOI:10.1002/14651858.CD007421.pub3.
- [Google Scholar]
- Effect of hyaluronan-enriched embryo transfer medium on IVF outcome: a prospective randomized clinical trial. Arch Gynecol Obstet. 2015;291:1173-1179.
- [Google Scholar]
- Impairment of the hatching process following IVF in the human and improvement of implantation by assisting hatching using micro-manipulation. Hum Reprod. 1990;5:7-13.
- [Google Scholar]
- Assisted hatching of human embryos: a systematic review and meta-analysis of randomized controlled trials. Hum Reprod Update. 2011;17:438-53.
- [Google Scholar]
- Assisted hatching on assisted conception (in vitro fertilisation (IVF) and ntracytoplasmic sperm injection (ICSI) Cochrane Database Syst Rev. 2012;12:CD001894.
- [Google Scholar]
- Assisted hatching and intracytoplasmic sperm injection are not associated with improved outcomes in assisted reproduction cycles for diminished ovarian reserve: an analysis of cycles in the United States from 2004 to 2011. Fertil Steril. 2014;102:1041-7.
- [Google Scholar]
- Fertility: assessment and treatment for people with fertility problems. NICE Clinical Guideline updated (2013). https://www.nice.org.uk-evidence-full-guideline-pdf-188539453
- Frozen versus fresh single blastocyst transfer in ovulatory women: a multicenter, randomized controlled trial. Lancet 2019 doi:org/10.1016/S0140-6736(18)32843-4
- [Google Scholar]
- Freeze-all versus fresh embryo transfer in ART: A multicenter randomized controlled trial in normo-ovulatory women. Hum Reprod. 2019;34(4):679-88.
- [Google Scholar]
- Preimplantation genetic testing for aneuploidy by microarray analysis of polar bodies in advanced maternal age: a randomized clinical trial. Hum Reprod. 2018;33:1767-76.
- [Google Scholar]
- Preimplantation genetic screening: a systematic review and meta-analysis of RCTs. Hum Reprod Update. 2011;17:454-66.
- [Google Scholar]
- Preimplantation genetic screening: back to the future. Hum Reprod. 2014;29:1846-50.
- [Google Scholar]
- Optimizing the culture environment and embryo manipulation to help maintain embryo developmental potential. Fertil Steril. 2016;105:571-87.
- [Google Scholar]
- Cumulus coculture and cumulus-aided embryo transfer increases pregnancy rates in patients undergoing in vitro fertilization. Fertil Steril. 2006;86:839-47.
- [Google Scholar]
- Effect of human granulosa cell co-culture using standard culture media on the maturation and fertilization potential of immature human oocytes. Fertil Steril. 2008;90:1674-9.
- [Google Scholar]
- Autologous endometrial coculture in patients with IVF failure: outcome of the first 1,030 cases. J Reprod Med. 2004;49:463-7.
- [Google Scholar]
- Beneficial effect of autologous endometrial cell coculture in patients with repeated implantation failure. Fertil Steril. 2010;93:769-73.
- [Google Scholar]
- Embryologic outcome and secretome profile of implanted blastocysts obtained after co-culture in human endometrial epithelial cells versus the sequential system. Fertil Steril. 2010;93:774-82.
- [Google Scholar]
- Oral contraceptive pretreatment significantly reduces ongoing pregnancy likelihood in gonadotrophin releasing hormone antagonist cycles: an updated meta-analysis. Fertility & Sterility. 2010;94:2382-84.
- [Google Scholar]
- Oral contraceptive pill, progestogen or estrogen pre-treatment for ovarian stimulation protocols for women undergoing assisted reproductive techniques. Cochrane Database of Systematic Reviews 2010:CD006109.
- [Google Scholar]
- Human chorionic gonadotropin, estradiol, and progesterone profiles in conception and non-conception cycles in an in vitro fertilization program. Fertility & Sterility. 1989;52:441-45.
- [Google Scholar]
- Comparison of pregnancy outcomes of progesterone or progesterone estradiol for luteal phase support in ICSI-ET cycles. Gynecologic and Obstetric Investigation. 2004;58:140-44.
- [Google Scholar]
- Inhibition of progesterone secretion by oestradiol administered in the luteal phase of assisted conception cycles. Medical Journal of Malaysia. 2003;58:187-95.
- [Google Scholar]
- Luteal Phase support for assisted reproduction cycles. 2015. Cochrane Database Systematic Review. https://doi.org/10.1002/14651858. CD009154.pub3
- [Google Scholar]
- The benefits of low-dose aspirin therapy in women with impaired uterine perfusion during assisted conception. Human Reproduction. 1994;9:1954-57.
- [Google Scholar]
- Aspirin for in vitro fertilisation. Cochrane Database of Systematic Reviews. 2011;8:CD004832.
- [Google Scholar]
- Preconceptional low-dose aspirin for the prevention of hypertensive pregnancy complications and preterm delivery after IVF: a meta-analysis with individual patient data. Human Reproduction. 2013;28:1480-88.
- [Google Scholar]
- Effect of antiphospholipid antibodies in women undergoing in-vitro fertilization: role of heparin and aspirin. Human Reproduction. 1997;2:1171-75.
- [Google Scholar]
- Heparin and aspirin treatment yields higher implantation rates in IVF patients with antiphospholipid antibodies seropositivity compared to untreated seronegative patients (abstract) Proceedings of the Annual Meeting of the American Society of Reproductive Medicine, Boston, USA 1996
- [Google Scholar]
- A randomized, double-blind, placebo-controlled trial of heparin and aspirin for women with in vitro fertilization implantation failure and antiphospholipid or antinuclear antibodies. Fertility & Sterility. 2003;80:376-83.
- [Google Scholar]
- High fecundity rates following invitro fertilization and embryo transfer in antiphospholipid antibody seropositive women treated with heparin and aspirin. Human Reproduction. 1994;9:2278-83.
- [Google Scholar]
- The selective use of heparin/aspirin therapy, alone or in combination with intravenous immunoglobulin G, in the management of antiphospholipid antibody-positive women undergoing in vitro fertilization. American Journal of Reproductive Immunology. 1998;40:74-82.
- [Google Scholar]
- Low-molecular-weight heparin in the treatment of recurrent IVF-ET failure and thrombophilia: a prospective randomized placebo-controlled trial. Human Fertility. 2008;11:246-53.
- [Google Scholar]
- Nitric oxide donors for patients undergoing IVF. A prospective, double-blind, randomized, placebo-controlled trial. Human Reproduction. 2002;17:2615-20.
- [Google Scholar]
- Effect of vaginal sildenafil on the outcome of in vitro fertilization (IVF) after multiple IVF failures attributed to poor endometrial development. Fertility & Sterility. 2002;78:1073-76.
- [Google Scholar]
- Endometrial growth and uterine blood flow: a pilot study for improving endometrial thickness in the patients with a thin endometrium. Fertility & Sterility. 2010;93:1851-58.
- [Google Scholar]
- Neither sildenafil nor vaginal estradiol improves endometrial thickness in women with thin endometria after taking oral estradiol in graduating dosages. Clinical and Experimental Obstetrics & Gynecology. 2004;31:99-102.
- [Google Scholar]
- Uterine junctional zone contractions during assisted reproduction cycles. Human Reproduction Update. 1998;4:440-45.
- [Google Scholar]
- A functional and structural study of the innervation of the human uterus. American Journal of Obstetrics & Gynecology. 1989;160:218-28.
- [Google Scholar]
- Endometrial wave like activity in the non-pregnant uterus. Hum Reprod Update. 2003;9:131-38.
- [Google Scholar]
- Assessments of embryo transfer after in-vitro fertilization: effects of glyceryl trinitrate. Human Reproductio. 1993;8:1426-28.
- [Google Scholar]
- Administration of beta2-adrenergic agonists during the peri-implantation period does not improve implantation or pregnancy rates in intracytoplasmic sperm injection (ICSI) cycles. Journal of Assisted Reproduction and Genetics. 2003;20:513-16.
- [Google Scholar]
- Effect of Piroxicam on ART Outcome: a Pilot Study. International Journal of Fertility and Sterility. 2014;8:243-8.
- [Google Scholar]
- Effect of Piroxicam administration before embryo transfer on IVF outcome: a randomized controlled trial. Repord Biomed Online. 2009;19:604-09.
- [Google Scholar]
- The impact of atosiban on pregnancy outcomes in women undergoing in vitro fertilization-embryo transfer: a meta-analysis. PloS One. 2012;12:e0175501. https://doi.org/10.137/journal.pone.0175501
- [Google Scholar]
- Oxytocin antagonists may improve infertility treatment. Fertil Steril. 2007;88:213.e19-22.
- [Google Scholar]
- The effect of peri-implantation administration of uterine relaxing agents in assisted reproduction treatment cycles: a systematic review and meta-analysis. Repro Biomed Online. 2016;32:362-76.
- [Google Scholar]
- Endometrial scratching for subfertility: everyone’s doing it. Hum Reprod. 2016;31:1241-4.
- [Google Scholar]
- Endometrial scratching: how much evidence do you need to stop offering this to women having in vitro fertilization. Fertil Steril. 2019;111:1092-3.
- [Google Scholar]
- Endometrial injury in women undergoing assisted reproductive techniques. Cochrane Database Syst Rev 2015:CD009517.
- [Google Scholar]
- Fertile ground: human endometrial programming and lessons in health and disease. Nat Rev Endocrinol. 2016;12:654-67.
- [Google Scholar]
- A randomized trial of endometrial scratching before in vitro fertilization. N Engl J Med. 2019;380:325-34.
- [Google Scholar]
- Endometrial scratching prior to IVF; does it help and for whom? A systematic review and meta-analysis. Human Reproduction Open 2019:1-18. (doi:10.1093/hropen/hoy025)
- [Google Scholar]
- Natural killer cells and pregnancy outcomes in women with recurrent miscarriage and infertility: a systematic review. Hum Reprod. 2011;26:1971-80.
- [Google Scholar]
- Treatment of recurrent IVF failure and human leukocyte antigen similarity by intravenous immunoglobulin. Repro Biomed Online. 2005;11:745-49.
- [Google Scholar]
- Is intravenous immunoglobulins (IVIG) efficacious in early pregnancy failure? A critical review and meta-analysis for patients who fail in vitro fertilization and embryo transfer (IVF) Journal of Assisted Reproduction and Genetics. 2006;23:1-13.
- [Google Scholar]
- Treatment with adalimumab (Humira) and intravenous immunoglobulin improves pregnancy rates in women undergoing IVF. Am J Reprod Immunol. 2009;61:113-20.
- [Google Scholar]
- Intravenous immunoglobulin treatment for repeated IVF/ICSI failure and unexplained infertility: a systematic review and a meta-analysis. American Journal of Reproductive Immunology. 2013;70:434-47.
- [Google Scholar]
- Adverse reactions and pathogen safety of intravenous immunoglobulin. Current Drug Safety. 2007;2:9-18.
- [Google Scholar]
- Not all intravenous immunoglobul in preparations are equally well tolerated. Acta Dermato-Venereologica. 2010;90:494-7.
- [Google Scholar]
- The safety profile of home infusion of intravenous immunoglobulin in patients with neuroimmunologic disorders. Journal of Clinical Neuromuscular Disease. 2011;12:S1-10.
- [Google Scholar]
- A meta-analysis of pregnancy outcomes in women with polycystic ovary syndrome. Human Reproduction Update. 2006;12:673-83.
- [Google Scholar]
- The effect of administration of intravenous intralipid on pregnancy outcomes in women with implantation failure after IVF / ICSI with non-donor oocytes: A randomized controlled trial. European Journal of Obstetrics & Gynaecology and Reproductive Biology. 2019;240:45-51.
- [Google Scholar]
- First successful pregnancy after addition of enoxaparin to sildenafil and etanercept immunotherapy in woman with fifteen failed IVF cycles − case report. American Journal of Reproductive Immunology. 2010;64:93-96.
- [Google Scholar]
- Degree of TNF- α/IL-10 cytokine elevation correlates with IVF success rates in women undergoing treatment with Adalimumab (Humira) and IVIG. American Journal of Reproductive Immunology. 2011;65:610-18.
- [Google Scholar]
- Die-off ratio correlates with increased TNF- α:IL-10 ratio and decreased IVF success rates correctable with humira. American Journal of Reproductive Immunology. 2012;68:428-37.
- [Google Scholar]
- Successful treatment of unresponsive thin endometrium. Fertil Steril. 2011;95:e13-17.
- [Google Scholar]
- A pilot cohort study of granulocyte colony-stimulating factor in the treatment of unresponsive thin endometrium resistant to standard therapies. Hum. Reprod. 2013;28:172-77.
- [Google Scholar]
- Evaluation of granulocyte colonystimulating factor effects on treatment resistant thin endometrium in women undergoing in vitro fertilization. Biomed Res Int 2014:913235.
- [Google Scholar]
- A randomized clinical trial of endometrial perfusion with granulocyte colony stimulating factor in in vitro fertilization cycles: impact on endometrial thickness and clinical pregnancy rates. Fertil Steril. 2014;101:710-5.
- [Google Scholar]
- Granulocyte colonystimulating factor administration forinfertile women with thin endometrium in frozen embryo transfer program. Reprod Sci. 2014;21:381-5.
- [Google Scholar]
- Two protocols to treat thin endometrium with granulocyte colony-stimulating factor during frozen embryo transfer cycles. Reprod Biomed Online. 2015;30:349-58.
- [Google Scholar]
- Strategies to manage refractory endometrium: state of the art in2006. Repro Biomed Online. 2016;32:474-89.
- [Google Scholar]
- Autologous platelet rich plasma promotes endometrial growth and improves pregnancy outcome during in vitro fertilization. Int J Clin Exp Med. 2015;8:1286-90.
- [Google Scholar]
- Platelet-rich plasma therapy and reproductive medicine. J Assist Reprod Genet. 2018;35:753-6.
- [Google Scholar]
- Effect of autologous platelet-rich plasma treatment on refractory thin endometrium during the frozen embryo transfer cycle: a pilot study. Front Endocrinol. 2019;10:61. doi: 10.3389/fendo.2019.00061
- [Google Scholar]
- Intrauterine administration of peripheral mononuclear cells in recurrent implantation failure: a systematic review and metaanalysis. Scientific Report. 2019;9:3897. https://doi.org/10.1038/s41598-019-40521-w
- [Google Scholar]
- Intrauterine administration of human chorionic gonadotropin (hCG) for subfertile women undergoing assisted reproduction. Cochrane Database Syst Rev. 2016;20:D011537.
- [Google Scholar]
- The effect of intrauterine HCG injection on IVF outcome: a systematic review and meta-analysis. Reprod Biomed Online. 2016;33:350-59.
- [Google Scholar]
- Effect of intrauterine injection of human choronic gonadotropin before fresh embryo transfer on IVF and ICSI outcomes: a meta-analysis. Archives of Gynecology and Obstetrics. 2018;298:1061-9.
- [Google Scholar]
- Intrauterine administration of autologous peripheral blood mononuclear cells promotes implantation rates in patients with repeated failure of IVF-embryo transfer. Hum Reprod. 2006;21:3290-94.
- [Google Scholar]
- Do circulating blood cells contribute to maternal tissue remodeling and embryo-maternal cross-talk around the implantation period? Mol Hum Reprod. 2009;15:335-43.
- [Google Scholar]
- Lifestyle behaviors in women undergoing in vitro fertilization: prospective study. Fertil Steril. 2012;97:697-701.
- [Google Scholar]
- Effect of acupuncture on the outcome of in vitro fertilization and intracytoplasmic sperm injection: a randomized, prospective, controlled clinical study. Fertil Steril. 2006;85:1347-5.
- [Google Scholar]
- Influence of acupuncture on the pregnancy rate in patients who undergo assisted reproduction therapy. Fertil Steril. 2002;77:721-4.
- [Google Scholar]
- Acupuncture performed around the time of embryo transfer: a systematic review and meta-analysis. Repro Biomed Online. 2019;38:364-79.
- [Google Scholar]
- Stress and infertility: a review. Int J Reprod Contracept Obstet Gynecol. 2016;5:940-3.
- [Google Scholar]
- A prospective study using Hatha Yoga for stress reduction among women waiting for IVF treatment. Reprod Bio Med Online. 2015;30:542-8.
- [Google Scholar]
- Impact of a group mind/ body intervention on pregnancy rates in IVF patients. Fertil Steril. 2011;95:2269-73.
- [Google Scholar]
- Yoga can improve assisted reproduction technology outcomes in couples with infertility. Alternative Therapies in Health and Medicine. 2018;24:50-5.
- [Google Scholar]







