Translate this page into:
To study the impact of blood and mucus on embryo transfer catheter tip and IVF outcome
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
To study the impact of blood and mucus on embryo transfer (ET) catheter tip and in vitro fertilisation (IVF) outcome.
Aims:
To compare the implantation rate and clinical pregnancy rate of blood and mucus on ET catheter tip.
Study setting:
Ajanta Hospital and IVF Centre, Lucknow, Uttar Pradesh.
Study design:
Prospective observational comparative study.
Study period:
August 2019 to March 2020.
Material and methods:
In this prospective observational comparative study, 60 patients undergoing IVF-ET were included in the study. Patients were observed for the presence of blood or mucus on the ET catheter tip. The tip of the ET inner catheter was examined under the microscope for the presence of blood or mucus. Statistical analysis: Statistical analysis was performed by the SPSS program of Windows, version 17.0 (SPSS, Chicago, Illinois). Continuous variables being presented as mean ± SD. Normally distributed continuous variables were compared by unpaired t test, whereas the Mann-Whitney U test used for not normally distributed variables. Categorical variables are analyzed by chi square test or Fisher test. P < 0.05 was taken as statistically significant.
Results:
By this study, it is observed that the implantation rate for mucus group was 66%, whereas for blood group is 20.6% (P value < 0.001). It is observed that the clinical pregnancy rate for mucus group was 66.7%, whereas for blood group was 29.2% (P value = 0.004).
Conclusion:
A successful ET needs to be smooth, easy to transfer, and have an atraumatic path through cervix and slow transfer of embryos in the endometrium for good implantation rate. This study showed that when blood was present on the ET catheter, there was decreased clinical pregnancy rate and implantation rate, whereas implantation rate (IR) and clinical pregnancy rate (CPR) were unaffected when mucus was present on catheter
Keywords
IVF
ET
IR
CPR
INTRODUCTION
Embryo transfer (ET) is the most important and crucial step in assisted reproductive technologies by which the ET is done in the endometrial cavity through the cervix. It is very important for a successful ET to have a viable embryo, receptive endometrium, good endometrial thickness, and expertise in ET technique is required. The ET technique plays a very important role in in vitro fertilisation (IVF) results. There is a significant difference among different people performing ET within the same setup of IVF depending upon their expertise. ET was performed for the first time in 1978 and is still being updated at every point of time. Many research and improvements have been done to improve an outcome and to have an atraumatic transfer of the embryo. The implantation rate is still low in ART in spite of many recent advancements. Expulsion of embryos that are transferred can be due to many factors that include uterine contractions, uterine peristalsis, site of ET, presence of blood and mucus, and negative pressure during ET.[1] ET technique largely influence IVF outcome, as good clinical pregnancy rate cannot be achieved without correct and expertise while doing the procedure of ET.[2] Hence, a great importance is being given to ET that is why it is important to understand about the factors that influence the success of ET
Factors affecting ET outcome:
Cervical mucus
Uterine contractions
Intrauterine lesions
Presence of blood on ET catheter
Endometrium
Mock ET
Ultrasound during ET
Type of media
Type of catheters
Presence of mucus on ET catheter tip: The cervical mucus is secreted by the cervix, under the influence of estrogen. The amount and quality of cervical mucus vary according to the menstrual cycle. There is more production of cervical mucus at the time of ovulation, under the estrogenic influence. After ovulation, under the effect of progesterone, the quantity of cervical mucus declines and becomes thicker in consistency. If cervical mucus is present at the time of ET, there are more chances of a retained embryo and increased embryo expulsion rate and may also cause bacterial contamination, hence it is advised to remove the cervical mucus before ET. According to many studies, vigorous cleaning of the cervix before ET is not advisable as it causes the start of uterine contractions and poor implantation rates. There are few studies that indicate that the removal of cervical mucus done just before ET had no effect on the clinical pregnancy rate.[3] However, according to other studies, it has been shown that the removal of cervical mucus before ET decreased implantation rates.[4]
There are many studies that have shown that aspiration of cervical mucus can decreases the bacterial infection rate and in turn improves the implantation rates.
According to a large retrospective study that included 470 ET, it is found that with blood and mucus, there was no effect on clinical pregnancy and implantation rates.[5] Enough evidence is there from different studies that it was beneficial to remove cervical mucus before ET to improve IVF outcome. Also, according to a Cochrane review, there was no evidence of benefit when the cervical mucus was removed before ET.[1]
Presence of blood on Embryo transfer catheter tip: Presence of blood indicates that it may come on ET catheter from two different sites:
Cervical bleeding is one of the most common causes. It can occur due to trauma caused while passing of catheter from the cervix or may be due to subclinical infection like bacterial vaginosis due to which cervix becomes friable and bleeds on touch.
Uterine bleeding is due to trauma occurring between the contact of the uterine wall and ET catheter. After trauma there is interference with embryo deposition and in turn implantation. Uterine contractions and increased peristalsis occur due to the presence of blood that further decreases the implantation rate.[6] Other studies are controversial about the presence of mucus and blood on ET catheter tip, whereas many studies found that there is a significant decrease in pregnancy rate,[7,8,9,10,11,12,13] whereas others have found no effect of blood or mucus. This study looks into the association of mucus or blood with success after IVF.
Methodology
The study was conducted in the ART department of Ajanta Hospital and IVF Centre, Lucknow (Uttar Pradesh) and the study subjects were women attending infertility clinic of 23 to
38 years of age from August 2019 to March 2020.
Study Design
The study was a prospective observational comparative study.
Inclusion Criteria:
Women undergoing IVF-ET aged 23 to 38 years.
Easy and difficult transfer.
Exclusion Criteria:
History of Cervical surgery
Uterine malformation
Coagulation disorder
On Oral anticoagulants/Heparin
In the present study, 60 women undergoing IVF-ET, aged 23 to 38 years, after taking proper informed consent and fulfilling inclusion criteria were recruited. After ET, ET catheter tips were observed for the presence of blood and mucus
Sample Size
We chose a 25% baseline ratio of implantation rate based on previous studies.[5] Thus, a sample size of 328 patients per group provided an 80% power for detecting a significant difference between the two groups at an alpha level of 0.05.
The formula for calculating sample size is given below:
Sample size of convenience: Sixty patients were included in the study. Because the study is time bound and as per the patient load in a private hospital, all consecutive patients who meet the eligibility criteria during the study period were enrolled in the study. Sample of convenience was taken less than the calculated sample size.
Statistical Methods
Statistical analysis was performed by the SPSS program of Windows, version 17.0 (SPSS, Chicago, Illinois). Continuous variables were presented as mean ± SD. Normally distributed continuous variables were compared by unpaired t test, whereas the Mann-Whitney U test was used for not normally distributed variables. Categorical variables were analyzed by chi-square test or Fisher test. P < 0.05 was taken as statistically significant.
Method of Recruitment
All women of age group 23 to 38 years who were undergoing IVF-ET from primary or secondary infertility attending Ajanta hospital and IVF Centre asked to participate in the study. They were fully informed about the study objectives and procedures. Only women who signed a consent form were enrolled in the study. The patient information sheet was given to the patients. Proper ethical clearance is well taken from hospital. For all the patients, complete history evaluation and physical examination were done.
Data Collection
All the data were collected by the investigator on a predesigned Performa.
PROCEDURE
In the present study, 60 women undergoing IVF-ET, aged 23 to 38 years, after taking proper informed consent and fulfilling inclusion criteria were recruited. All patients had gone through mock ET in the previous cycle for assessment of the position of the uterus. For ET procedure, the patient is laid in the dorsal lithotomy position, Perineum is cleaned with normal saline and draped. Under all aseptic precautions Cusco”s bivalved speculum is inserted into the vagina and the cervix is cleaned with normal saline to minimize contamination, Outer sheath of ET catheter is inserted gently in the cervix under USG guidance,[14] embryos are loaded into ET catheter by the embryologist, and then under transabdominal ultrasound guidance, embryos are transferred into the endometrium. It is very important to avoid touching the fundus and keep a distance of 1 to 2 cm from the ET catheter tip. After doing an ET, the catheters are given back to and checked by embryologists for outer and inner catheters for the presence of mucus and blood. Light microscopy is used to examine the tip of the inner transfer catheter for the presence of mucus or blood. Fluid present inside the inner catheter is examined for blood, mucus, or retained embryos Figures 1 and 2.
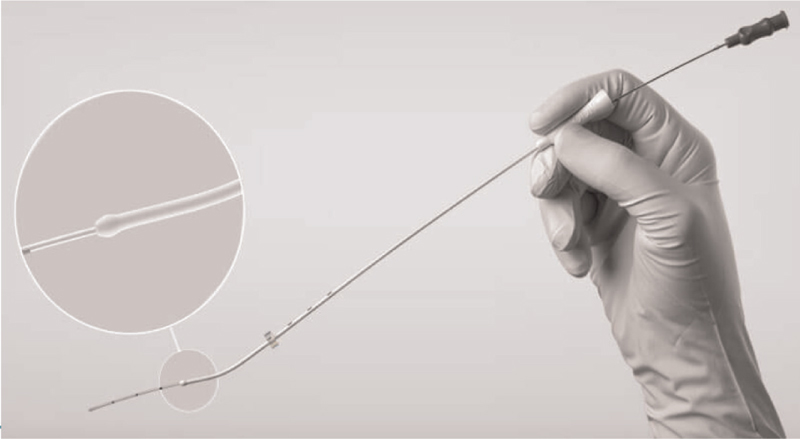
- Embryo transfer catheter
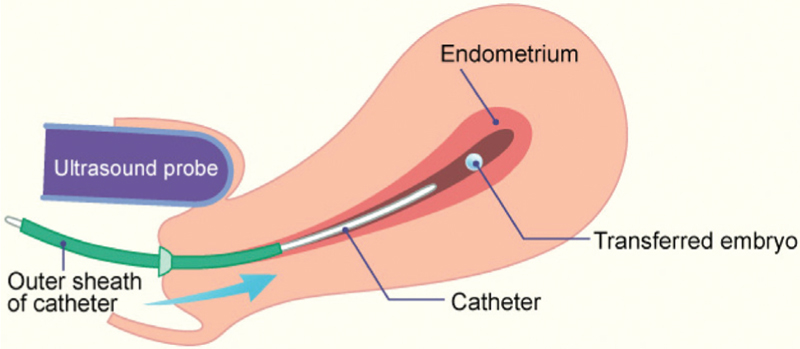
- Embryo transfer technique
Outcome Variables
Primary objective: Implantation rate. “The number of gestational sacs seen divided by the number of embryos transferred (in%).”
Secondary objective: Clinical pregnancy rate. “The number of clinical pregnancies expressed per 100 initiated cycles or ET cycles. When clinical pregnancy rates are recorded, the denominator (initiated or aspirated or ET cycles) must be specified. The main independent variable will be mucus and or blood on the transfer catheter. The other demographic and clinical variables to be studied as potential confounders are age, type of infertility, cause of infertility, type of ART, type of stimulation, type of embryo, quality of embryo, number of embryos transferred, and so forth.
ETHICAL CONSIDERATIONS
Ethical issues were addressed as follows:
Informed written consent was taken from all couples. No pressure was exerted on subjects for participation in the study.
Confidentiality and privacy was ensured at all levels.
The subject was free to leave the study at any time and no questions were asked further. However, they were not debarred from getting any medical services as being provided to the other participants.
Ethical clearance was taken.
RESULTS AND OBSERVATION
Table 1 shows the group distribution of the patients under the study. Sixty percent of patients were included in group I, that is, mucus group, and 40% of patients were included in group II, i.e., blood group.
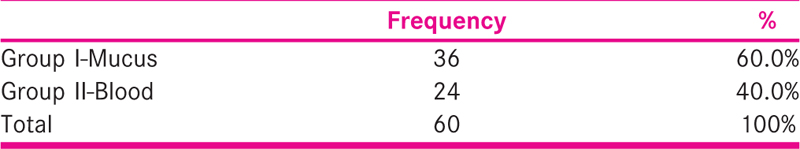
Table 2 shows the comparison of the age distribution of the patients between the two groups under the study. It was observed that under the group Mucus, 47.2% of the patients were in the age group of 26 to 30 years, 30.6% were in 31 to 35 yrs, 13.9% patients were in 36 to 40 years, and 8.3% patients were in 21 to 25 yrs age group. Under the blood group, 29.2% of the patients each were in the age group of 21 to 25 years and 31 to 35 years, respectively, and 20.8% of the patients each were in 26 to 30 years and 36 to 40 years of age group.
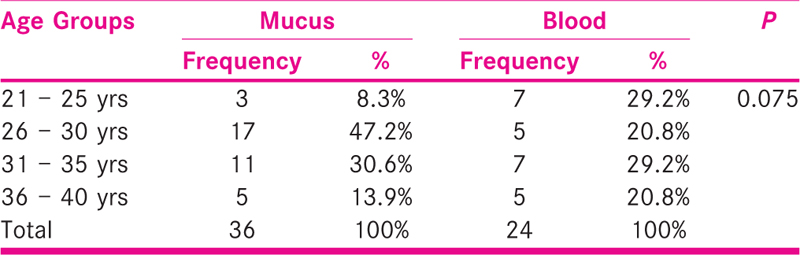
Further, it is observed that there is no statistically significant difference in the distribution of patients between the two groups (P value = 0.075)
Table 3 shows that the mean age under group mucus was 30.22 ± 4.13 years, whereas the mean age in group blood was 30.25 ± 5.21 years.

Further, it is observed that there is no significant difference in mean age between the two groups (P value = 0.982).
Table 4 shows the comparison of various parameters under the Male Factor between the two groups under the study. It was observed that under the group Mucus, 13.9% of the patients had azoospermia, 5.6% had asthenospermia, and 2.8% had OAT. Under the Blood group, 12.5% of the patients had azoospermia, and 4.2% of the patients each had OAT, oligospermia, and teratospermia.
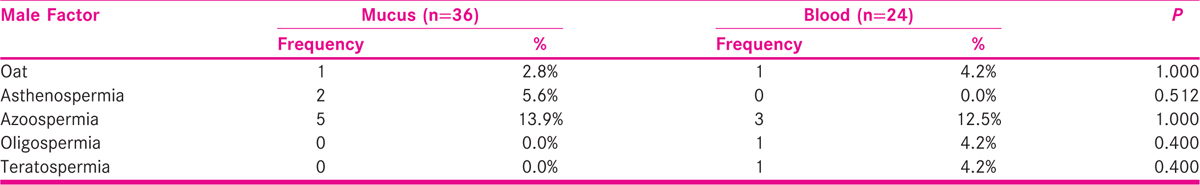
Further, it is observed that there is no significant statistical difference in the Male Factors between the two groups.
Table 5 shows the comparison of various parameters under the Female Factor between the two groups in the study. It was observed that in the group Mucus, 22.2% of the patients each had poor ovarian reserve and bilateral tubal block, 11.1% patients had endometriosis grade 4 and BTB, 8.3% patients had severe PCOS, and 2.8% had secondary. Under the Blood group, 25% of the patients had poor ovarian reserve, 16.7% of patients had Endometriosis Grade 4 and BTB, 8.35 had severe PCOS, and 4.2% had Secondary.

Further, it was observed that there is no statistically significant difference across the Female Factors between the two groups.
Table 6 shows the comparison of the unexplained factor between the two groups. It was observed that under group Mucus, 19.4% of the patients had unexplained factor, whereas for the group Blood, 12.5% of the patients had the unexplained factor.
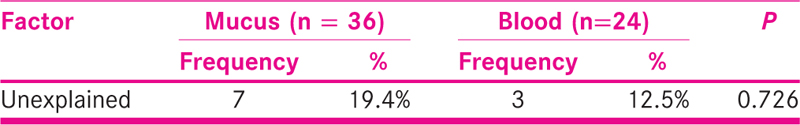
Further, it is observed that there is no statistically significant difference between the two groups (P = 0.726)
[Table 7] shows the comparison of the distribution of patients according to the type of stimulation between the two groups. Under the group mucus, 80.6% of the patients had an antagonist type of stimulation while 19.4% had an agonist type of stimulation. Under the group blood, 75% of the patients had an antagonist type of stimulation, whereas 25% had an agonist type of stimulation.
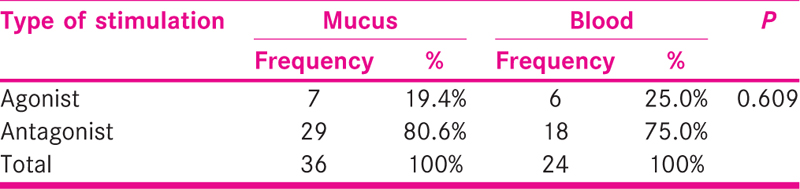
Further, it was observed that there is no statistically significant difference between the two groups (P = 0.609).
Table 8 shows the comparison of the distribution of patients according to the type of embryo between the two groups. Under the group Mucus, 58.3% of the patients had D3 type of embryo, whereas 41.7% of patients had D5 type of embryo. Under the group Blood, 50% of the patients had D3 and 50% of patients had D5 type of embryo.
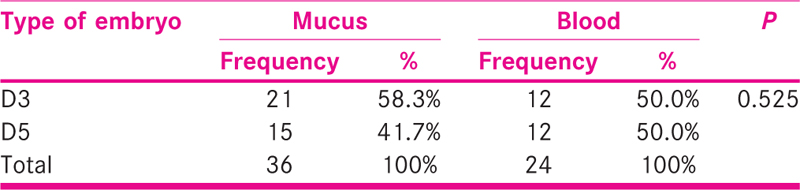
Further, it was observed that there is no statistically significant difference in the distribution of patients according to the type of embryo between the two groups (P = 0.525).
Table 9 shows the comparison of the distribution of patients according to the type of embryo between the two groups. Under the group Mucus, 52.8% of the patients had frozen embryo, whereas 47.2% of patients had fresh embryo. Under the group Blood, 50% of the patients had fresh and 50% of patients had frozen embryo.
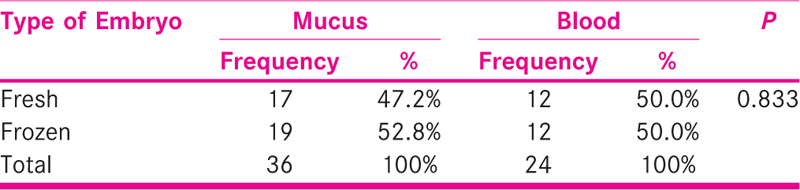
Further, it was observed that there is no statistically significant difference in the distribution of patients according to the type of embryo between the two groups (P = 0.833).
Table 10 shows the comparison of the distribution of patients according to Easy/Difficult with Tenaculum between the two groups. Under the group Mucus, 100% of the patients were Easy. Under the group Blood, 95.8% of the patients had Difficult with Tenaculum, whereas 4.2% of patients had Easy with Tenaculum.
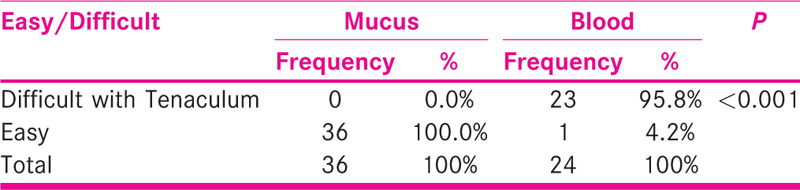
Further, it was observed that there is a statistically significant difference in the distribution of patients according to Easy/Difficult with Tenaculum between the two groups (P < 0.001).
Table 11 shows the number of gestational sac under the study. It was observed that the gestational sac 0 was 46.7%, gestational sac 1 was 40%, and gestational sac 2 was 13.3%.

Table 12 shows the comparison of the distribution of patients according to TVS cardiac Activity (for clinical pregnancy rate) between the two groups. Under the group Mucus, 69.4% of the patients had positive TVS Cardiac activity, whereas 30.6% had negative activity. Under the group Blood, 20.8% of the patients had positive TVS cardiac activity, whereas 79.2% had negative activity.
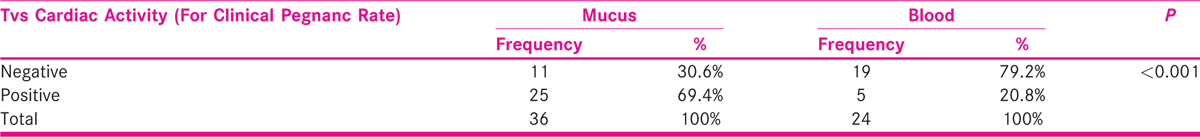
Further, it was observed that there is a statistically significant difference in the distribution of patients according to TVS Cardiac activity between the two groups (P < 0.001)
Table 13 shows that the implantation rate was 47.6% for gestational sac with respect to embryo transferred.
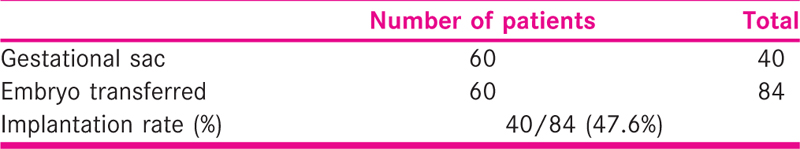
Table 14 shows that the pregnancy rate (%) was 51.7% for cardiac activity present with respect to the number of embryos transferred.

Table 15 shows a comparison of implantation rate with respect to the number of embryos transferred and gestational sac between the two groups under the study. It was observed that the implantation rate for the Mucus group was 66%, whereas for the Blood group was 20.6%.
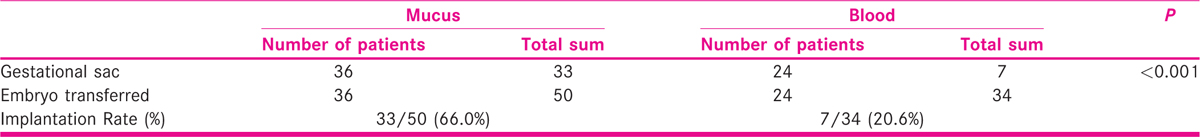
Further, it was observed that there is a statistically significant difference in implantation rate when compared between the two groups (P < 0.001).
Table 16 shows the comparison of pregnancy rate (%) present with respect to number of embryos transferred and cardiac activity between the two groups under the study. It was observed that the pregnancy rate for the Mucus group was 66.7%, whereas for the Blood group was 29.2%.

Further, it was observed that there is a statistically significant difference in the pregnancy rate when compared between the two groups (P = 0.004).
DISCUSSION
ET is the most integral step for ART. Hence, all possible factors that can affect implantation rates while doing an ET have been extensively studied.[9,15] Among all the factors, mucus and blood on ET catheter have shown different results in implantation rate (IR) and clinical pregnancy rate (CPR), which otherwise tells IVF OUTCOME. This study evaluates the implantation rate and clinical pregnancy rate when blood or mucus on the ET catheter tip was present. While looking into the pathology, blood on ET catheter might arise from two sources. Either it can be due to Cervical bleeding, which is a more common cause, or can be uterine bleeding, which shows that trauma and contact occurred between ET catheter and the endometrium, therefore, shows difficult ET. When mucus is present on the catheter tip it shows a simple pathophysiology. It involves contamination of the cervix and hence the presence of mucus on the catheter does not influence the success rate of IVF. An adverse effect of mucus is the retention of embryos that causes a block of catheter opening.[6] Hence, it is advisable to remove the extra amount of cervical mucus before ET to reduce the probability of retained embryos. The result of this study regarding the effect of mucus and blood on ET catheter and IVF outcome, supported by previous studies describes decreased IR and CPR with blood on catheter.[2] As the difficulty in ET increases, there are more chances that blood may appear on the ET catheter, presence of blood on the ET catheter, leads to a decrease in IR (20.6%) and CPR (29.2%), whereas mucus on the tip of the ET catheter does not affect IR (66%) and CPR (66.7%), this finding is similar to previously published data.[18] According to this study, it was observed that the implantation rate for the Mucus group was 66%, whereas for the Blood group was 20.6%. It is observed that there is a significant difference in implantation rate when compared between blood and mucus groups (P < 0.001. It is observed that the CPR for the Mucus group was 66.7%, whereas for the Blood group was 29.2%. It was found that there is a statistically significant difference in clinical pregnancy rate when it is compared between the two groups (P = 0.004). This study showed decreased IR, CPR in ETs in which blood is present on the catheter whereas IR and CPR remained unaffected in mucus on the catheter.
The pregnancy rate was significantly decreased as reported by Awonuga et al.[2] when blood was present on the catheter. The presence of mucus or blood suggests difficult ET. There are increased chances of embryos to get retained when ET catheter had contamination with mucus (17.8 versus 3.3%) or blood (12 versus 3.3%). Significant reduction was seen in pregnancy when there was contamination of ET catheter with blood (15.5% versus 27.1%; P = 0.002), which was statistically significant.[2] When blood on the catheter was found it had decreased IR and CPR in ART. According to Alvero et al.,[17]no significant differences in IR or CPR were not found when mucus was present on the transfer catheter. The analysis confirmed that the presence of blood on ET catheter was considered an important factor in predicting CPR (P = 0.018) and IR (P = 0.042).[16]
Visschers et al.[3] studied the outcome of ET when cervical mucus was removed before ET in IVF on the birth rate. A total of 317 couples were taken in the study. Fifty-two of 220 (24%) cycles in the treatment group had live birth as compared to 42 of 205 (21%) in the control group. By this study, it is clear that if cervical mucus was removed before ET, it has significantly increased live birth rate. In another study by Dasig et al.[6] They conducted a study on 775 women undergoing IVF-ET and found the effect of blood or mucus on the ET catheter. They found that 11% (84/775) cycles had blood and mucus on ET catheter and significant lesser ongoing pregnancy rates when blood or mucus was present on the tip of ET catheters.
Cervical mucus covers the ET catheter while it is passed from the cervical canal and it interferes with the correct transfer of the embryo in the uterine cavity. Hence, to remove, cervical mucus before ET has an insignificant effect on the birth rate.[3] Atraumatic ET procedure and avoiding bleeding while doing an ET contributes toward improved pregnancy rate in IVF.[17] According to Alvero et al.[16] avoiding blood on ET catheter leads to good CPR. ET associated with blood on the catheter usually suggests difficulty and is at increased risk of uterine bleeding as compared to bleeding from the cervix. The presence of Blood in the endometrial cavity hinders embryo implantation and causes contractions arising due to trauma and causes a significant decrease in CPR and IR. Always it is not possible to find out the exact cause of bleeding. It may be due to bleeding diathesis, medications or endometrium abnormalities.[1] According to Snehlata et al.,[18] they included 81 cycles planned for IVF and pregnancy rate was comparatively less in cases where blood was found on ET catheter than without blood ET catheter (16.00% versus 53.57%; P = 0.839), pregnancy and IR where mucus was present on ET catheter, there was no significant difference (60.86% versus 51.72%; P = 0.456)
CONCLUSION
ET is one of the important and final rate-limiting step in ART. ET should be easy and have an atraumatic passage of the ET catheter in the lower uterine segment through the cervix that is followed by slowly transfer of the embryos in the endometrium.[15] The expert technique of procedure of ET is very important to provide appropriate conditions that ultimately favors implantation of the embryo to have a successful outcome. ET is a very important and expert procedure, it is an integral and final step of ART. Although other factors affect the final success of an IVF cycle, inadequate ET technique causes a negative effect on implantation and pregnancy. Optimizing the steps of ET will maximize the successful embryo-endometrium interaction, which in turn leads to a viable pregnancy. According to this study, blood present on ET catheter is detrimental to IR and CPR. On the other hand, mucus does not have any effect on IR and CPR.
Financial support and sponsorship
NIl.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Effect of blood and mucus on the success rates of embryo transfers. Eur J Obstet Gynecol Reprod Biol. 2012;165:239-42.
- [Google Scholar]
- Contamination of embryo transfer catheter and treatment outcome in in vitro fertilization. J Assist Reprod Genet. 1998;15:198-201.
- [Google Scholar]
- Removal of cervical mucus: effect on pregnancy rates in IVF/ICSI. Reprod Biomed Online. 2007;15:310-5.
- [Google Scholar]
- Removal of cervical mucus prior to embryo transfer improves pregnancy rates in women undergoing assisted reproduction. Reprod Biomed Online. 2007;14:308-13.
- [Google Scholar]
- Effect of macroscopic or microscopic blood and mucus on the success rates of embryo transfers. Fertil Steril. 2010;93:570-3.
- [Google Scholar]
- IVF outcomes: effects of blood or mucus on the tip of a soft embryo transfer catheter after embryo transfer. Fertil Steril. 2011;95:S26.
- [Google Scholar]
- Does the presence of blood in the catheter or the degree of difficulty of embryo transfer affect live birth. Reprod Sci. 2017;24:726-730.
- [Google Scholar]
- The role of uterine straightening by passive bladder distension before embryo transfer in IVF cycles. J Assist Reprod Genet. 1997;14:32-34.
- [Google Scholar]
- Dummy embryo transfer: a technique that minimizes the problems of embryo transfer and improves the pregnancy rate in human in vitro fertilization. Fertil Steril. 1990;54:678-81.
- [Google Scholar]
- Embryo afterloading: a refinement in embryo transfer technique that may increase clinical pregnancy. Fertil Steril. 2005;83:710-714.
- [Google Scholar]
- Uterine junctional zone contractions during assisted reproduction cycles. Hum Reprod Update. 1998;4:440-5.
- [Google Scholar]
- Evolution of a culture protocol for successful blastocyst development and pregnancy. Hum Reprod. 1998;13:169-77.
- [Google Scholar]
- The influence of the depth of embryo replacement into the uterine cavity on implantation rates after IVF: a controlled, ultrasound-guided study. Hum Reprod. 2002;17:341-6.
- [Google Scholar]
- Impact of transabdominal ultrasound guidance on performance and outcome of transcervical uterine embryo transfer. J Assist Reprod Genet. 2003;20:318-22.
- [Google Scholar]
- A meta-analysis of ultrasound-guided versus clinical touch embryo transfer. Fertil Steril. 2003;80:1037-41.
- [Google Scholar]
- The presence of blood in the transfer catheter negatively influences outcome at embryo transfer. Hum Reprod. 2003;18:1848-52.
- [Google Scholar]
- Blood on the embryo transfer catheter is associated with decreased rates of embryo implantation and clinical pregnancy with the use of in vitro fertilization-embryo transfer. Fertil Steril. 1998;70:878-2.
- [Google Scholar]
- Effect of mucous, blood and bacterial contamination at the time of embryo transfer, and its impact on the IVF pregnancy outcome. Glob J Reprod Med. 2017;3:55-59.
- [Google Scholar]








