Translate this page into:
An unusual case of Mullerian anomaly: “accessory cavitated uterine mass”
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The present study presents a case report of a rare anomaly called accessory cavitated uterine mass (ACUM). The patient, 26 years old, had presented with severe dysmenorrhea which was refractory to the medical treatment. The hysteroscopic examination was normal and laparoscopic examination showed a subserosal bulge, present over anterior and lateral fundal region above the attachment of the round ligament. Chromo-pertubation was performed and dye came freely from both the tubes but not from the cavity of this uterine mass. The chocolate-colour material was drained during excision of the mass. The final histopathology report showed myometrial tissue lined by collection of hemosiderin laden macrophages as well as endometrial cuboidal lining and occasional endometrial glands.
Keywords
Accessory cavitated uterine mass (ACUM)
dysmenorrhoea
juvenile cystic adenoma (JCA)
mullerian anomalies
INTRODUCTION
Accessory cavitated uterine masses (ACUM) with a functional endometrium represent a new variety of Mullerian anomaly that is generally located at the level of insertion of round ligament and is possibly related to a dysfunction of the female gubernaculum.[1] In these women, the whole uterus develops normally by fusion of the two Mullerian ducts into a single uterine cavity with both the fallopian tubes, yet a cavitated mass present in one of the lateral sides of the uterus, lined by proper endometrium. The diagnosis of ACUM is generally made on the following findings: it should be an isolated accessory cavitated mass lined by endometrial epithelium with glands and stroma within a normal musculature of the uterus with its own endometrial cavity with normal fallopian tubes and ovaries. On surgical excision, it contains thick chocolate-brown color fluid within, and on histology, there is no evidence of adenomyosis of the wall, although there could be small foci of adenomyosis in the myometrium around the accessory cavity.[2] In literature, ACUMs have been described as accessory uterine cavities, isolated, or juvenile cystic adenomyomas (JCAs), or as uterus-like masses. There is a paucity of data in the literature of such cases especially from the Indian perspective. The purpose of this case report is to bring alertness of this rare diagnostic dilemma, having broad differential diagnosis that can be easily confused with other Mullerian anomalies. Awareness and widespread publications of such cases encountered will eventually find a place in the regular textbooks for postgraduate students, describing this condition as a new variety of Mullerian duct anomalies and will help to consider preoperative diagnosis of ACUM more accurate. In 2010, Acien et al.[2] reviewed the literature and found 18 cases including four of their own cases and considered them to be ACUMs but had been described as uterine-like masses. Further, Acien et al.[1] again reported their four new cases of ACUM along with 15 more cases described as juvenile cystadenoma (JCA). Out of these, nine cases were reported by Takeuchi et al.[3] in 2010 in women under 30 years of age that was possibly the highest number reported by any one person so far.[4,5] After the two literature reviews in 2010 and 2011, four more cases were found in the literature by various clinicians.[6,7,8] Paul et al.[9] from Kerala reported three additional cases of ACUM who presented with severe dysmenorrhea refractory to the medical treatment. Now, we also report one more case of ACUM, which was diagnosed preoperatively as a functional rudimentary horn.
CASE
Twenty-six-year-old women married for 3 months, presented to us with complaints of pain in the lower abdomen for the past 6 years. She had regular menstrual cycles, which were associated with dysmenorrhea right from the time of menarche. This dysmenorrhea had become more severe from the past 6 years and was refractory to analgesics. The patient had an MRI report suggesting the diagnosis of a unicornuate uterus with a well-developed right horn and a rudimentary cavitatory noncommunicating left horn. The rudimentary horn showed the presence of hemorrhagic contents. A pelvic ultrasound was done to reconfirm the diagnosis, which instead showed a bulky uterus with a subserosal cystic lesion along the left lateral aspect of the uterus measuring 46 × 38 mm across. Application of color Doppler showed increased peripheral vascularity suggesting the diagnosis of subserosal cystic adenomyotic focus or the possibility of a degenerative fibroid. We further investigated the patient for surgery and took her for hystero-laparoscopic evaluation and treatment. On hysteroscopy, the uterine cavity was normal with both ostia seen in the same plane, hence the possibility of the unicornuate uterus was ruled out. A primary umbilical 5-mm port and two ancillary 5-mm trocars, lateral to the right and left epigastric vessels were put. On laparoscopic evaluation, uterus was asymmetrically enlarged and both tubes were seen attached to the two sides of the posterior lateral wall of the fundus in the same plane unlike in a unicornuate uterus. Bilateral fallopian tubes and ovaries normal in appearance. A subserosal bulge was present over the anterior and lateral fundal region above the attachment of the round ligament. Vasopressin was injected under the serosa as in all myoma/adenomyoma resection and after blanching of the mass incision was given over the bulge. On extending and deepening the incision to find the plane of resection, thick chocolate-colored fluid came out that was approximately 30 to 50 ml. After drainage of fluid, a cavity was seen in the myometrium. Chromo-perturbation was performed and the dye came freely from both the tubes but not from the cavity of this uterine mass. This suggested that the cavity of uterine mass had no direct communication with the main uterine cavity. A part of wall of the cavity was sent for a frozen section that suggested normal uterine muscle tissue of the uterus with hemosiderin deposits again suggesting the diagnosis of the rudimentary horn. The entire cavity with surrounding myometrial tissue was dissected, excised, and sent for histopathological evaluation. The final histopathology report showed myometrial tissue lined by a collection of hemosiderin-laden macrophages as well as endometrial cuboidal lining and occasional endometrial glands (Figs 1-4).

- Laparoscopy finding of vasopressin being injected at the bulge seen over the left side of the anterior uterine myometrium near the insertion of the round ligament.

- Incision given over the mass.
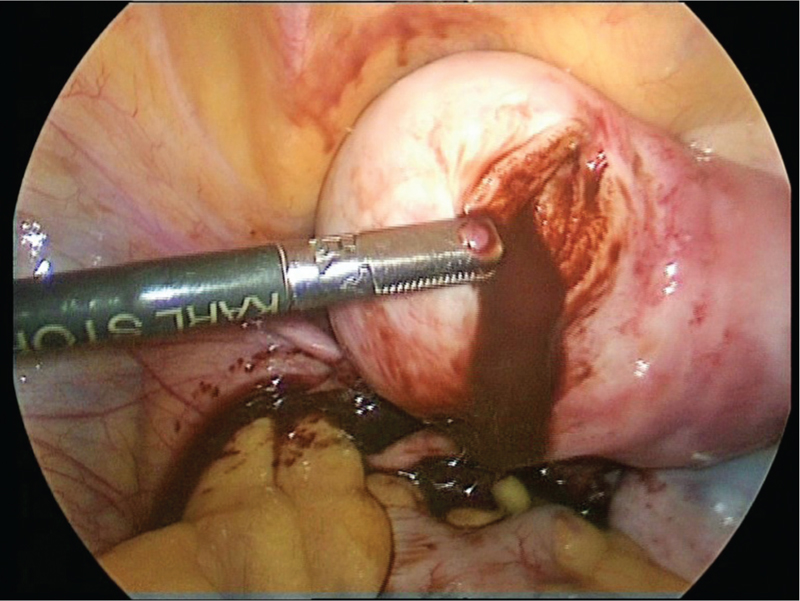
- Mass incised with chocolate-colored fluid.
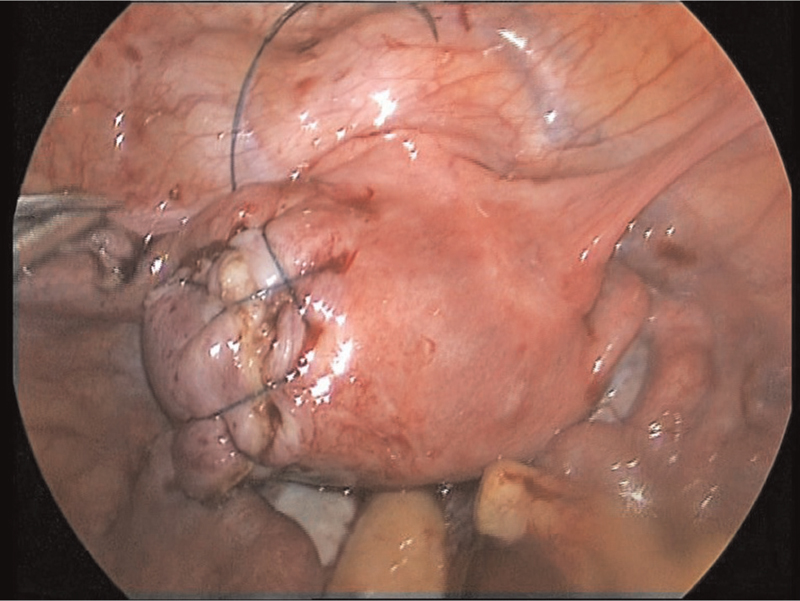
- Defect closed meticulously.
DISCUSSION
Development
It appears that even if ACUM is not directly a Mullerian duct anomaly, it is formed during the development of the uterus from the Mullerian ducts and evolution wise may have some similarity to the rare development of Gartner’s cyst that are mesonephric remnants but during embryonic development may continue to exist as cyst far away from the 86 course of the ducts.
Clinical suspicion
The pathognomonic clinical feature of ACUM is its early onset of severe dysmenorrhea, which usually starts soon after menarche. This symptom could be attributed to intracystic bleeding and stretching of the cystic cavity.
Diagnosis
Apart from a 3D ultrasound, MRI and conventional HSG are helpful but laparoscopy is the only confirmatory option for such a rare disorder.
Histologically, accessory uterine horns and ACUM’s both have a thick myometrial wall with a cavity lined by an endometrial epithelium.
Management
Early diagnosis and surgical intervention involving laparoscopic removal of the mass can shorten the usually prolonged suffering of these young women. For complete symptom relief, complete excision of the mass is required. Our patient had significant improvement in her pain.
Clinical implication
Except a few cases, most of the cases were misdiagnosed preoperatively as other Mullerian anomalies, cystic degeneration in adenomyoma and leiomyoma, and broad ligament fibroids. Awareness and adequate knowledge of the entity can help to make an accurate preoperative diagnosis of ACUM.
CONCLUSION
Cases of ACUM can be misdiagnosed as unicornuate or bicornuate Mullerian anomalies or cystic adenomyomas. Gynecologists’ as well as radiologists should be aware of and keep a high index of suspicion about this condition to make an accurate preoperative diagnosis. It appears that this condition is not as rare as previously believed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- New cases of accessory and cavitated uterine masses (ACUM): a significant cause of severe dysmenorrhea and recurrent pelvic pain in young women. Human Reprod. 2012;27:683-94.
- [Google Scholar]
- The cavitated accessory uterine mass: a Müllerian anomaly in women with an otherwise normal uterus. Obstet Gynecol. 2010;116:1101-9.
- [Google Scholar]
- Diagnosis, laparoscopic management, and histopathologic findings of juvenile cysticadenomyoma: a review of nine cases. Fertil Steril. 2010;94:862-8.
- [Google Scholar]
- Robot‑assisted laparoscopic management of a case with juvenile cystic adenomyoma. Fertil Steril. 2010;94:e55-e56.
- [Google Scholar]
- Juvenile cystic adenomyoma in a 19-year-old woman: a case report with a proposal for new diagnostic criteria. J Laparoendoscopic Adv Surg Techn. 2011;21:771-4.
- [Google Scholar]
- Laparoscopic management of juvenile cystic adenomyoma: four cases. J Minim Invasive Gynecol. 2011;18:343-8.
- [Google Scholar]
- Cystic Adenomyoma simulates uterine malformation: a diagnostic dilemma: case report of two unusual cases. J Hum Reprod Sci. 2012;5:285-8.
- [Google Scholar]
- Accessory and cavitated uterine Mass with functional endometrium in an adolescent: diagnosis and laparoscopic excision technique. J Pediatr Adolesc Gynecol. 2013;26:e89-e91.
- [Google Scholar]
- Accessory cavitated uterine mass: a rare cause of severe dysmenorrhea in young women. J Minimal Invasive Gynecol. 2015;22:1300-3.
- [Google Scholar]







