Translate this page into:
Impact of color Doppler assessment and interventions on the outcome of frozen-embryo transfer in infertile women
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Context:
A good blood supply is essential for endometrial receptivity which in turn impacts the outcome of frozen-embryo transfers (FETs) in infertile women. With the advent of Doppler ultrasound, studying endometrial blood flow has emerged as an important means of evaluating endometrial receptivity.
Aim:
This study was undertaken to assess the usefulness of color Doppler as a marker of predictor of outcome in FET cycles.
Settings and Design:
This was a retrospective study conducted at the Southend Fertility and IVF Centre on all women who underwent FET cycle as part of the infertility management at the center.
Materials and Methods:
A total of 400 women were recruited in the study with 200 in case group (Group A) and 200 in control group (Group B).
Statistical analysis:
Statistical analysis was carried out using data analysis software system, SPSS V27 and Microsoft excel.
Results:
In Group A, 70 (35%) women became pregnant and 130 (65%) did not conceive. On the other hand, in Group B, 55 (28%) women became pregnant, and 145 (72%) did not conceive.
Conclusion:
Endometrial and subendometrial vascularity as measured by color Doppler is a useful predictor for pregnancy in FET cycles. However, there is still no larger consensus as to whether measurement of endometrial and subendometrial blood flow using color Doppler is useful and whether it plays any role in predicting of the pregnancy cycle outcome. Further large randomized trials are required to reach to definite conclusion on this topic.
Keywords
Color Doppler
endometrial and subendometrial vascularity
endometrial receptivity
infertility management
pulsatility index
resistance index
INTRODUCTION
In vitro fertilization (IVF) has evolved rapidly since its inception 40 years ago. Advancements include controlled ovarian stimulation with gonadotropin, which multiplied the number of oocytes retrieved. Further, embryo cryopreservation made it possible to conserve surplus embryos for future use, and thus increased cumulative live-birth rates after an IVF cycle. Observational studies and small randomized controlled trials have shown higher pregnancy rates and better perinatal outcomes with frozen-embryo transfer (FET) than with fresh-embryo transfer.[1,2,3,4]
Since less than 20% of FET cycles result in pregnancy and live birth, it is important to carefully evaluate the various factors that may affect the treatment result.[5] The failure of implantation may be caused by the low quality of the embryo(s) transferred or by a nonreceptive uterine endometrium.
A good blood supply to endometrium is considered necessary for implantation. Various markers have been proposed to evaluate endometrial receptivity, such as molecular markers and sonographic markers. With the advent of Doppler ultrasound, studying endometrial blood flow has emerged as an important means of evaluating endometrial receptivity.
Doppler ultrasound examination of uterine vessels is a noninvasive assessment of the uterine blood flow, which may affect uterine receptivity and implantation. Usage of Doppler in an IVF cycle to measure the endometrial and subendometrial blood flow and its subsequent role in predicting the outcome has gained importance in the recent years. However, the various studies on this topic have given conflicting conclusions.
Hence, this study was undertaken to assess the usefulness of color Doppler as a marker of endometrial receptivity in FET cycles.
The objective of the study was to evaluate the role of uterine artery Doppler in a FET cycle to predict ART outcome:
Primary outcome − Pregnancy seen as an intrauterine gestation sac
Secondary outcome − Effect of therapy on blood flow parameters
MATERIALS AND METHODS
It was a retrospective study conducted at the Southend Fertility and IVF Centre from October 2020 to April 2021. The study was conducted on all women who underwent FET cycle as part of the infertility management at the center, irrespective of their previous embryo transfer outcomes, were included in the study.
A total of 400 women were recruited in the study with 200 in control and 200 in case group. A total of 200 women (cases) who underwent FET along with the Doppler ultrasound were compared with 200 women (controls) who underwent FET without the Doppler assessment during preparation.
Ethical clearance was obtained from the Independent Ethics Committee of Indian Fertility Society (IFS). The selection of the women for the study was based on the following inclusion and exclusion criteria:
Inclusion criteria considered for this study were:
All infertile women who underwent FET preparation
Normal serum prolactin levels <20 ng/ml
Euthyroid women (TSH < 3.5)
Day 2/3 LH, FSH < 10 MIU/ml
D2/3 E2 < 50 pg/ml
Exclusion criteria considered for this study were:
Uterine anomalies
Prolactin > 20 ng/ml
TSH > 3.5
Day 2/3 FSH > 10 MIU/ml
Day 2/3 E2 > 50 pg/ml
Baseline scan with endometrial thickness (ET) > 5 mm and any residual active cyst in the ovaries
Suboptimal response to endometrial preparation
Methods
Baseline ultrasound and hormonal profile were performed on Day 2/3. Baseline hormonal profile included serum LH, E2, and P4 levels.
Baseline TVS was carried out to confirm adequate endometrial shedding (ET < 5 mm) and rule out any residual follicle/cyst in ovaries.
Endometrial preparation was carried out using any of the following protocols:
Ovulation induction protocol − tablet. Letrozole 2.5 mg once daily for 5 days from D2 to D7 with/without injection human menopausal gonadotropins (HMG)
HRT protocol − Endometrial preparation with tablet Estradiol, filtrated as per ultrasound monitoring
Downregulated HRT protocol − Downregulation with tablet Ovral/Meprate in the previous cycle followed by an overlap and injection leuprolide for the last 3 to 4 days. An endometrial preparation and Estradiol was started from D3 of the next cycle.
Monitoring for endometrial assessment was carried out at periodic intervals. Ultrasonography (USG) Doppler was performed on D12 to D14 of the cycle, once endometrium had reached >7.5 mm thickness.
If Doppler parameters were normal, that is, vascularity up to zones 3 to 4, resistance index (RI) < 0.8, pulsatility index (PI) <3, switchover was carried out with progesterone using two routes.
If found abnormal, injection low molecular weight heparin (LMWH) 20/40 units was started and ET performed only if the flows improved.
Embryo transfer was carried out on D4 of progesterone for a D3 transfer and on sixth day of progesterone for a D5 transfer. Post-transfer, luteal support was given using progesterone through two routes and supplementation with injection human chorionic gonadotropin (HCG) was carried out on Days 3, 6, and 9 post-transfer.
S. beta HCG was carried out on D16 post-transfer to confirm pregnancy
For the purpose of data analysis, subgroups were created according to:
The underlying infertility factors
Use of heparin
Type of protocol used
Day of transfer
Type of luteal phase support
Statistical analysis
Statistical analysis was carried out using data analysis software system, SPSS V27 and Microsoft excel. Independent sample t test was used to calculate the independence of two samples and the statistically significant value, that is, P-value. Continuous data were expressed as mean ± standard deviation and P-value of 0.05 was considered as statistically significant. NS represents a nonsignificant difference between the two samples being considered.
RESULTS
In the study, a total of 400 women who underwent FET were investigated. These women were divided into two groups: Group A (women who underwent color Doppler ultrasound before FET, N = 200) and Group B (women who underwent FET without color Doppler, N = 200). Various baseline characteristics for both these groups were assessed in detail and a summary of the findings was assessed.
Table 1 includes the baseline characteristics for both the groups. In Group A, 70 (35%) women became pregnant and 130 (65%) did not conceive. On the contrary, in Group B, 55 (28%) women became pregnant and 145 (72%) did not conceive. The average age of women in Group A was 34.14 ± 4.95 years and in Group B, it was 33.47 ± 4.86 years. Thus, the average age was comparable in both the groups. It was observed that primary infertility was observed in 114 (57%) women and 140 (70%) women in Group A and Group B, respectively, whereas secondary infertility was observed in 86 (43%) and 60 (30%) women in Group A and Group B, respectively.

The various factors associated with infertility were assessed. It was observed that incidence of polycystic ovary syndrome (PCOS) was comparable in both the groups. It was 70 (35%) and 74 (37%) in Groups A and B, respectively. It was reported that 56 (28%) and 66 (33%) patients with infertility were associated poor or diminished ovarian reserve and 16 (8%) and 18 (9%) had premature ovarian failure in Groups A and B, respectively. Tubal factor-associated infertility was observed in 40 (20%) and 62 (31%) patients in Groups A and B, respectively. Incidence of endometriosis was comparable in both the groups. Endometriosis was observed in 36 (18%) and 34 (17%) patients in Groups A and B, respectively.
Past incidence of Tuberculosis was also comparable in both the groups. It was 22 (11%) and 18 (9%) in Groups A and B, respectively. Adenomyosis or Fibroid was reported in 44 (22%) and 42 (21%) patients in Groups A and B, which was again comparable. Male factor infertility was reported in 64 (32%) and 72 (36%) patients in Groups A and B, respectively.
History of previous IVF cycle was present in 110 (55%) and 112 (56%) patients in Groups A and B, and it was the first IVF cycle in 90 (45%) and 88 (44%) patients in Groups A and B, respectively. Thus, the number of cycles was comparable in both the groups.
As shown in Figures 1 and 2, majority of the cases and controls under study were given HRT and downregulated protocol. In Group A, 115 and 51 patients were given HRT and downregulated protocol, respectively, of which 34 and 21 patients conceived. In Group B, 92 and 94 patients were given HRT and downregulated protocol, of which 22 and 26 patients conceived.

- Variation of frozen-embryo transfer protocol and pregnancy outcome for cases.

- Variation of frozen-embryo transfer protocol and pregnancy outcome for controls.
Figures 3 and 4 show the correlation between various causative factors of infertility and their impact on the pregnancy outcome. Male factor infertility was reported in 64 and 72 patients in Groups A and B, respectively, of which 22 and 20 patients had positive pregnancy outcome.

- Bar diagram for infertility factor and number of total cases and positive outcome cases.
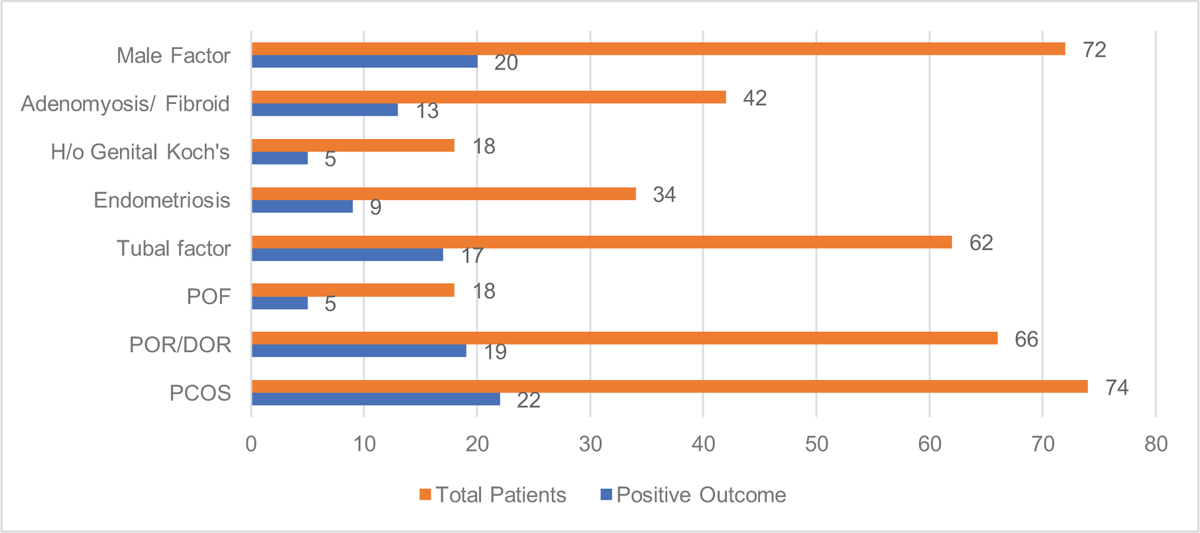
- Bar diagram for infertility factor and number of total controls and positive outcome controls.
Adenomyosis and fibroid were present in 44 and 42 patients in Groups A and B, of which 16 and 13 patients conceived. Previous history of tuberculosis was present in 22 and 18 patients in Groups A and B, out of which 5 patients became pregnant in both the groups. Almost similar number of patients had endometriosis in Groups A and B, that is, 36 and 34, of which, 10 and 9 patients conceived in both the groups, respectively.
Infertility associated with tubal factor was reported in 50 and 62 patients in Groups A and B, out of which 17 patients became pregnant in both the groups. In Group A, 16 and 56 women had premature ovarian failure and diminished ovarian reserve, of which 6 and 20 women became pregnant. Similarly, in Group B, 18 and 66 women had premature ovarian failure and diminished reserve, of which 5 and 19 women conceived, which is comparable to Group A. In Group A, 70 patients had PCOS, of which 25 conceived, which is similar to 74 patients of PCOS in Group B, of which 22 conceived.
Table 2 summarizes the various infertility factors and the positive outcome in patients with those factors in both the groups. In patients with PCOS, 25 (36%) conceived in Group A, whereas 22 (30%) conceived in Group B. Similarly, pregnancy rate was higher in patients with poor ovarian reserve and patients having premature ovarian failure in Group A when compared with Group B. In Group A, 36% patients with poor ovarian reserve conceived, whereas 29% conceived in Group B.

In patients having premature ovarian failure, 38% conceived in Group A and 28% conceived in Group B. Positivity rate was 34% in Group A and 27% in Group B, in patients with associated tubal factor. Positivity rate in patients with endometriosis was similar, 28% and 26% in Groups A and B, respectively. Patients who conceived were 23% in Group A and 28% in Group B in patients with the history of Tuberculosis. Positivity rate was 36% and 31% in Groups A and B in patients with adenomyosis or fibroid, respectively. In patients with male factor, 34% conceived in Group A, whereas in Group B 28% conceived.
Table 3 summarizes the trend of PI, RI, and vascularity zones with pregnancy outcome for cases. It was observed that mean PI was lower (2.21 ± 0.58) in patients who conceived, when compared with those who did not (2.80 ± 0.56) and this difference was statistically significant (P < 0.001). Similarly, the mean RI was lower in patients who conceived when compared with those, who did not, (0.67 ± 0.06) versus (0.77 ± 0.07), respectively, which was again statistically significant (P < 0.001). It was reported that the ratio of patients in cases in vascularity zone 3 was significantly higher in the pregnant group at 51% when compared with the nonpregnant group which stood at 45%.

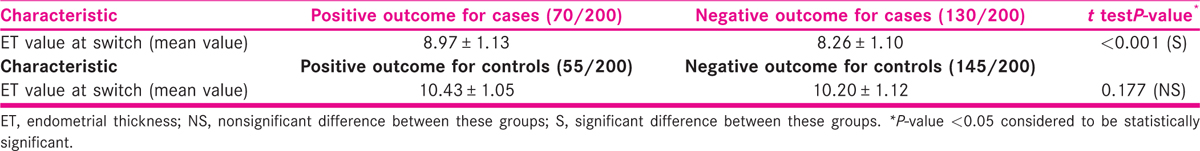
Table 4 depicts the trend of endometrial thickness in patients who conceived and in patients who did not, in both case and control groups. Mean endometrial thickness in cases was more (8.97 ± 1.13) in patients who conceived, when compared with those who did not conceive (8.26 ± 1.10) and this difference was statistically significant (P < 0.001). Similarly, in control group, mean endometrial thickness was more (10.43 ± 1.05) in patients who conceived, when compared with those who did not conceive (10.20 ± 1.12). However, this difference was not statistically significant (P = 0.177).
DISCUSSION
The role of receptive endometrium in implantation is well established. A good blood supply is essential for endometrial receptivity which in turn impacts the outcome of FETs in infertile women. Various studies have focused on measurement of endometrial and subendometrial blood flow using color Doppler and their role in predicting cycle outcome, but the results are conflicting.
Singh et al. had carried out a prospective study on 101 infertile women in 2009.[6] Women with tubal factor, male factor, and unexplained infertility were included in their study and they concluded that endometrial vascularity has a predictive value on the implantation rate in IVF cycles. The mean age of patients was 35 years in the above-mentioned study, which is comparable to the mean ages of patients in our study (34.14 ± 4.95 for cases and 33.47 ± 4.86 for controls).
As per our study, maximum conception was observed in cases having endometrial blood flow till zone 3 (51%), which is like the results of the study conducted by Singh et al. wherein 51.8% patients who became pregnant had blood flow till zone 3.
Mishra et al. had studied the role of endometrial and subendometrial blood flow measured by 3D power Doppler for prediction of pregnancy in FET cycles.[7] They assessed and compared the endometrial and subendometrial blood flows between the pregnant and the nonpregnant groups.
They concluded that study of endometrial and subendometrial vascularity by 3D power Doppler is useful in predicting pregnancy in FET cycles. In our study, patients who conceived had lower mean PI value at 2.21 ± 0.58, when compared with those, who did not conceive (2.80 ± 0.56). On similar lines, mean RI was lower in patients who conceived, 0.67 ± 0.06, when compared with those who did not 0.77 ± 0.07.
Sardana et al. concluded that pregnancy rate was found to be significantly higher at 35.43% in the presence of subendometrial–endometrial blood flow when compared with 15.78% when the blood flow was absent.[8] Clinical pregnancy rate and implantation rate were also significantly higher in Group A when compared with Group B (31.49% and 14.79% versus 13.15% and 6.52%). Thus, they concluded that presence of endometrial blood flow significantly improves cycle outcome in FET cycles.
As per results of the study carried out by Strohmer et al., on 323 stimulated cycles of women undergoing IVF treatment, the results showed that the PI of patients who conceived was significantly low when compared with those who did not become pregnant.[9] This is comparable to our study where cases who conceived had lower PI and RI values in comparison to cases who did not conceive.
Similarly, Steer et al. in their study on the correlation between uterine artery impedance with immunohistochemical, histologic, and ultrasonographic markers of uterine receptivity concluded that the PI on day 14 was significantly lower in those patients who conceived when compared with those who did not conceive.[10] Hence, uterine artery impedance has a significant correlation with biochemical markers of uterine receptivity and it accurately predicts the probability of pregnancy in FET cycles.
In their study, Kim et al. also concluded that 3D power Doppler ultrasound is a useful and effective method for assessing endometrial blood flow in IVF cycles.[11] Good endometrial blood flow on the day of embryo transfer is associated with high pregnancy success, as it is indicative of endometrial receptivity. This is on similar lines to our study, where higher pregnancy rate was observed in patients having vascularity in zone 3 and zone 4.
Ardaens et al. stated that in ART, the measure of the blood flow is important, as it correlates to the number and quality of harvested oocytes.[12] This neo-angiogenesis is also important in endometrium, especially for the embryo implantation. Doppler ultrasound allows estimation of the endometrial receptivity.
The study concluded that the chances of pregnancy are almost zero, if endometrial thickness is <8 mm and uterine PI is >3. As per our study also, all cases who underwent the ART cycle had mean endometrial thickness more than 8 mm. Additionally, the cases who conceived in our study were observed to have a mean PI value of 2.21 ± 0.58 which is a similar finding to the above-mentioned study. Thus, Doppler ultrasound is a thereby a useful complement to standard vaginal ultrasound in ART.
However, as per some other studies, not much difference was found between the endometrial–subendometrial vascularity and PI–RI values between pregnant and nonpregnant patients who underwent embryo transfer.
In their study, Zhang et al. found that pregnant patients had similar endometrial thickness, endometrial volume, endometrial pattern, uterine PI, RI, S/D, and endometrial and subendometrial vascularization index (VI), flow index (FI), and vascularization flow index (VFI) when compared with the nonpregnant patients.[13] As per this study, the Doppler parameters of endometrium measured were not good predictors of pregnancy and its outcome in IVF treatment. On similar lines, Check et al. also concluded that at least for FET, there does not appear to be any relationship of sonographic endometrial parameters (endometrial and subendometrial blood flow, PI, RI) with the pregnancy rates.[14]
Prasad et al. in their study concluded that uterine artery Doppler in women undergoing IVF cycles does not predict the pregnancy outcomes.[15] They found that mean PI during early follicular phase and on the day of HCG trigger between the pregnant and nonpregnant groups were comparable (2.09 ± 1.15 versus 1.9 ± 0.95; P = 0.385 and 1.86 ± 1.12 versus 2.03 ± 1.0; P = 0.192). They also did not find any significant changes in the uterine artery PSV, Systolic/Diastolic (S/D) values, and RI during the cycle.
Tekay et al., in their study, did not find any difference in uterine PI between pregnant and nonpregnant women.[16] Hence, they also concluded that the prognostic outcome of the IVF therapy could not be improved with Doppler. Ng et al. carried out a study to know the impact of endometrial and subendometrial blood flows on pregnancy outcome.[17] As per them, vascularity of endometrial and subendometrial layers measured by 3D power Doppler ultrasound was not a good predictor of pregnancy in FET cycles.
As can be observed from the results of the above-mentioned studies, there is still no larger consensus as to whether measurement of endometrial and subendometrial blood flow using color Doppler is useful and whether it plays any role in predicting of the pregnancy cycle outcome. Further large studies are required to reach to definite conclusion on this topic.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Obstetric and perinatal outcomes in singleton pregnancies resulting from the transfer of frozen thawed versus fresh embryos generated through in vitro fertilization treatment: a systematic review and meta-analysis. Fertil Steril. 2012;98:368-77.e1-9.
- [Google Scholar]
- Fresh versus frozen embryo transfer: backing clinical decisions with scientific and clinical evidence. Hum Reprod Update. 2014;20:808-21.
- [Google Scholar]
- Elective cryopreservation of all pronucleate embryos in women at risk of ovarian hyperstimulation syndrome: efficiency and safety. Hum Reprod. 1999;14:1457-60.
- [Google Scholar]
- Evidence of impaired endometrial receptivity after ovarian stimulation for in vitro fertilization: a prospective randomized trial comparing fresh and frozen-thawed embryo transfers in high responders. Fertil Steril. 2011;96:516-8.
- [Google Scholar]
- Assessment of endometrial and ovarian characteristics using three dimensional power Doppler ultrasound to predict response in frozen embryo transfer cycles. Reprod Biol Endocrinol. 2009;7:151.
- [Google Scholar]
- Predictive value of endometrial thickness, pattern and sub-endometrial blood flows on the day of hCG by 2D Doppler in in-vitro fertilization cycles: a prospective clinical study from a tertiary care unit. J Hum Reprod Sci. 2011;4:29-33.
- [Google Scholar]
- Endometrial and subendometrial vascularity by three-dimensional (3D) power Doppler and its correlation with pregnancy outcome in frozen embryo transfer (FET) cycles. J Obstet Gynaecol India. 2016;66(Suppl 1):521-7.
- [Google Scholar]
- Correlation of subendometrial-endometrial blood flow assessment by two-dimensional power Doppler with pregnancy outcome in frozen-thawed embryo transfer cycles. J Hum Reprod Sci. 2014;7:130-5.
- [Google Scholar]
- Prognostic appraisal of success and failure in an in vitro fertilization program by transvaginal Doppler ultrasound at the time of ovulation induction. Ultrasound Obstet Gynecol Off J Int Soc Ultrasound Obstet Gynecol. 1991;1:272-4.
- [Google Scholar]
- Vaginal color Doppler assessment of uterine artery impedance correlates with immunohistochemical markers of endometrial receptivity required for the implantation of an embryo. Fertil Steril. 1995;63:101-8.
- [Google Scholar]
- Detection of endometrial and subendometrial vasculature on the day of embryo transfer and prediction of pregnancy during fresh in vitro fertilization cycles. Taiwan J Obstet Gynecol. 2014;53(3):360-5.
- [Google Scholar]
- Contribution of ovarian and uterine color Doppler in medically assisted reproduction techniques (ART) Gynecol Obstet Fertil. 2002;30:663-72. [in French]
- [Google Scholar]
- The role of three-dimensional power Doppler ultrasound parameters measured on hCG day in the prediction of pregnancy during in vitro fertilization treatment. Eur J Obstet Gynecol Reprod Biol. 2016;203:66-71.
- [Google Scholar]
- The relationship of color and power Doppler ultrasound parameters of pulsatility and resistance indices and sub-endometrial blood flow with endometrial thickness on day prior to progesterone administration and their relationship to clinical pregnancy rate following frozen embryo transfer. Fertil Steril. 2003;80:123.
- [Google Scholar]
- The relationship between uterine artery two-dimensional color Doppler measurement and pregnancy outcome: a prospective observational study. J Reprod Infertil. 2017;18:251-6.
- [Google Scholar]
- Blood flow changes in uterine and ovarian vasculature, and predictive value of transvaginal pulsed colour Doppler ultrasonography in an in-vitro fertilization programme. Hum Reprod Oxf Engl. 1995;10:688-93.
- [Google Scholar]
- The role of endometrial and subendometrial vascularity measured by three-dimensional power Doppler ultrasound in the prediction of pregnancy during frozen-thawed embryo transfer cycles. Hum Reprod Oxf Engl. 2006;21:1612-7.
- [Google Scholar]







