Translate this page into:
Effect of age on semen parameters
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Aim:
This study was designed to evaluate the effect of age on various semen parameters.
Settings:
Womens Center and Hospitals Pvt. Limited, Coimbatore.
Design:
Observational cross-sectional study was conducted from October 2020 to March 2021.
Study subjects:
Male partners of 366 infertile couples attending the infertility clinic at Womens Center, Coimbatore.
Materials and methods:
Semen samples collected by masturbation were evaluated for parameters such as volume, sperm concentration, motility, and morphology as per the standard World Health Organization 2010 (5th edition) guidelines.
Outcome measures:
Comparison of volume, concentration, normal morphology, and motility in different age groups: <30, 30–35, 36–40, and >40 years.
Results:
No significant association of volume, concentration, and normal morphology with age was observed. However, there was a significant decline in motility with age.
Conclusion:
In the present study, motility was the only semen parameter that had a significant negative association, whereas all the other parameters did not exhibit any change with advancing age.
Keywords
motility
semen analysis
and semen parameters
INTRODUCTION
Male factors alone or in combination with female factors contribute to 50% of the total infertility cases. The female biological clock has been well established as having a negative effect on fertility. However, the risks of abnormal pregnancies and heritable effects associated with advancing paternal age are poorly understood.
It has been observed in recent years that there has been a shift in the average paternal age of the first child for a variety of reasons. As couples delay childbearing, it is becoming increasingly important to determine whether the advanced paternal age of infertile couples is associated with diminished semen quality.
Semen analysis is a primary step in the laboratory evaluation of the infertile male. It includes the assessment of the semen volume, sperm concentration, motility, and morphology using World Health Organization (WHO) criteria.
Some studies have shown that with increasing paternal age, semen volume, sperm motility, and the percentage of normal morphology tend to decrease.[1,2] However, other studies had conflicting conclusions and there is no consensus among various studies.
Thus, this study is planned to evaluate various semen parameters in different age groups of men attending an infertility clinic.
MATERIALS AND METHODS
This observational cross-sectional study was conducted from October 2020 to March 2021.
Sample size
Sample size of 468 was calculated based on the study of Kumar et al.[3] In their study carried out in central India, they evaluated the semen analysis of 1219 participants categorizing them into five subgroups (group 1: 21–28 years; group 2: 29–35 years; group 3: 36–42 years; group 4: 43–49 year, and group 5: 50–60 years). Pearson’s correlation was applied to find out significant changes between age and semen parameters.
Even though the calculated sample size was 468, due to the coronavirus disease 2019 pandemic situation, the patient load was not up to the expected level. Hence, only 366 male partners of infertile couples were recruited into the study.
Study subjects
Male partners of infertile couples attending the infertility clinic at womens center, Coimbatore. Written informed consent was taken from the participants before recruiting them in the study and collecting their clinical specimens. A detailed history including information on lifestyle habits and occupation besides medical and surgical history was documented as per the proforma. Results of female partner evaluation were also noted from the couple’s file.
All participants were assessed for their serology status for viral/bacterial infections including human immunodeficiency virus (HIV)-1 and HIV-2, hepatitis B surface antigen, hepatitis C virus, and venereal disease research laboratory test before semen analysis.
Inclusion criteria
All male partners of couples who presented for infertility evaluation were included in the study.
Exclusion criteria
Azoospermia
Men with ejaculatory and erectile dysfunction
Recent febrile illness (in the preceding 3 months)
Chemotherapy, radiation therapy, any reproductive surgery in the last 6 months
History of hormonal therapy and antioxidant therapy in the last 6 months
Semen collection
Subjects were instructed to report to the center for semen analysis after 2 to 5 days of abstinence. Semen was collected by them through masturbation into a clean sterile, wide-mouth sample collection container. In case of loss of part or complete sample because of spillage or other reasons, patients were instructed to report and come for a repeat sample. If any participant failed to provide a sample in the clinic, he was offered to bring the sample from home provided the sample could reach the laboratory within half an hour of collection time.
Semen analysis
The samples were kept at room temperature for about 20 to 30 minutes for liquefaction, after which semen analysis was performed according to the standard WHO 2010 (5th edition) guidelines.[4] After liquefaction, the viscosity of the sample was estimated by gently aspirating it into a Falcon pipette, allowing the semen to drop by gravity and observing the length of thread.
The general appearance of the sample was also noted. Semen volume was estimated by Falcon graduated pipette. The pH value was measured using pH paper and compared with a calibration strip.
To determine the concentration of sperm, 10 µl of thoroughly mixed semen was loaded on a Makler counting chamber (Sefi Medical Instruments, Haifa, Israel) under a light microscope at a magnification of 10×. The number of sperm cells in 100 squares was counted which gives the concentration of sperm in millions/ml. The motility parameter was graded according to the WHO classification (5th edition) into forward progressive motility, nonprogressive motility, and immotility. If round cells >1 million/ml noted, LeucoScreen test was performed using the LeucoScreen test kit.
Sperm morphology
Smears were prepared for sperm morphology and vitality assessment. Following fixation (air-dried) using an Eosin & Nigrosin staining kit (Krishco Medical Products, India), the slide was examined with bright field optics at 100× magnification with oil immersion, sperm morphology was assessed according to Kruger strict criteria.[5] At least 100 spermatozoa were counted from each sample. The results were expressed as the percentage of live sperms, dead sperms, normal spermatozoa, head defects, midpiece defects, and tail defects. The patients were divided into four groups based on their ages: <30, 30 to 35, 36 to 40, and >40 years.
Statistical analysis
The data were entered in Microsoft excel and were analyzed using SPSS software version 23. Categorical variables were presented as frequency and percentages, and continuous variables were presented as mean ± standard deviation. Independent sample T test was used to measure the association between the semen analysis parameters and different age groups. Bivariate analysis using Chi-squared/Fischer exact test was applied between categorical variables and outcome. P < 0.05 was considered as statistically significant.
RESULTS
Our study subjects were between the age of 26 and 48 years with a mean age of 32.69 ± 4.29. Majority (77%) were below the age of 35 years and only 6% were above 40 years of age [Table 1].

Distribution of study population according to semen parameters is represented in Figure 1. The semen volume in the samples ranged from 0.2 to 6 ml, and in nearly 30% samples, the volume was <1.5 ml. On the other hand, the sperm concentration in the samples ranged from 0.5 to 145 million/ml and 18% of subjects showed concentration of less than 15 million/ml. The percentage of samples showing normal morphology (>4%) was only18%. Sperm motility in the samples ranged from 0% to 95% with 7.7% of samples showing motility less than normal value of 40%.

- Distribution of normal and abnormal semen parameters in the study population.
As shown in Table 2, when comparing different age groups, the semen volume, concentration, and morphology were comparable and there was no statistically significant difference of these parameters with age. In contrast to the other parameters measured, sperm motility showed significant decline with age. The mean sperm motility in the study population was 60.99% with <30 years age group, showing the highest mean value of 62.8% and the 31 to 35 years age group not far behind with a mean value of 62.32%. The age group 36 to 40 years exhibited the lowest mean value of 54.49%.
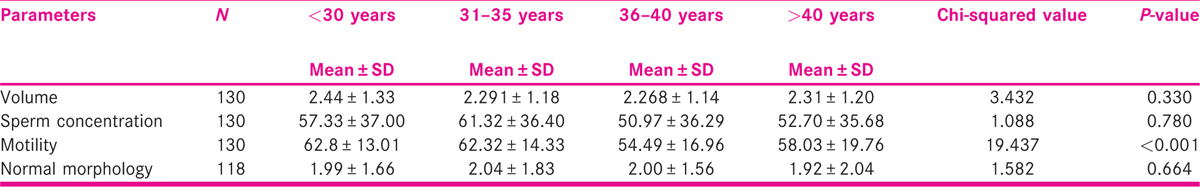
As shown in Figure 2, semen volume, sperm concentration, and normal morphology have no significant association with age. However, as age increases, sperm motility decreases and the difference is statistically significant.

- Percentage of study subjects with abnormal values of various semen parameters.
DISCUSSION
The outcome of our study reveals that age does not have a significant effect on semen volume, concentration, and normal morphology. However, age has a significant negative effect on motility.
Aging is a natural and irreversible process affecting all body parts including the reproductive system. Although the effect of maternal ageing on a couple’s fertility and reproduction is well documented, the role of paternal age on the same is not studied enough. There are many studies suggesting that women over the age of 35 years have a higher risk of infertility, pregnancy complications, spontaneous abortion, congenital anomalies, and perinatal complications.[6] However, literature on the impact of paternal age on a couple’s fertility remains unclear. Although spermatogenesis continues until late in life, and according to theory, it enables men to father a child even at a very advanced age, male fertility also seems to decline with age. Male reproductive organs undergo both minor and major changes as time passes, thereby leading to deterioration in semen parameters, hormone profile, and testicular cytological structure.[7]
Our results are in accordance with those of Winkle et al. who analyzed the semen parameters in 320 unselected patients and 84 normozoospermic controls, and their findings suggest that sperm motility decreased with increasing age, whereas concentration and normal morphology did not decline in aging men.[8]
A similar study which was a retrospective study by Gallo et al. found no correlation between male age and semen parameters such as semen volume, concentration, normal morphology, and motility in 439 couples.[9]
From our data, we did not find evidence that increasing age may affect concentration. This finding is supported by some other studies.[10,11,12] There are many studies that also reveal either a decrease or even an increase in sperm concentration with increasing age. For example, a study by Kumar et al. on 1219 male partners of infertile couples of rural tertiary care center of central India revealed a significant negative association of concentration with age.[3] Contrary to this, a study by Brahem et al. comprising semen samples of 140 infertile patients between 24 and 76 years of age and 50 fertile men between 25 and 65 years of age illustrated that with increased male age, sperm concentration increased.[13]
In addition to concentration, the present study reveals that the percentage of normal morphology is also to be unaffected with increasing age. Similar results were found by Winkle et al. in their study on 320 unselected patients and 84 normozoospermic controls in the year 2008.[8] This was further supported by studies conducted by Brahem et al.[13] There are some other studies that confirm that normal morphology declines with increasing age.[12,14,15]
Furthermore, our study showed no statistically significant change in semen volume with age which is supported by evidence provided by Sunanda et al. on 730 subjects in the year 2014.[15] This result contrasts with some data reported in other works of literature in which authors found that there is a pronounced decrease in semen volume with age.[16,17,18,19,20]
In contrast to other semen parameters, our study observed a statistically significant fall in sperm motility with aging. This is similar to many studies which indicate a fall in motility with advanced male age.[11,18,20] Moreover, a study by Sloter et al. revealed that sperm motility decreases by 0.8% per year and linear motion decreases by 0.2% per year.[21] On the other hand, there are many other studies that indicate no significant correlation between age and motility. For example, a study by Brahem et al.[13] and Li et al.[10] conclude that age does not have any impact on sperm motility.
Motility is a fundamental sperm property, it is necessary to enable the sperm cell to swim up the genital tract, penetrate the oocyte, and form the male pronucleus. Sperm motility appears to be very important not only for natural fertility but also in assisted reproduction, especially in the most advanced technique, Intracytoplasmic sperm injection, which allows fertilization with very few spermatozoa. In this case, it is of critical importance to have motile sperm cells, an unmistakable sign of their viability. Kasai et al.[22] demonstrated a higher fertilization and pregnancy rate in patients with higher sperm motility.
In recent years, there has been a shift in the average paternal age of the first child for a variety of reasons and therefore it is very important to understand the effect of age on sperm motility.
This study could serve to provide valuable knowledge not only in the determination of couple fertility prospects but also in the education of the general public about aging and fertility [Table 3].

Limitations
Study subjects in this study were male partners of infertile couples that might have caused some selection bias. So our study subjects were reproductively compromised individuals in comparison to other general population. In addition, our study took only age into consideration but there can be many other factors such as smoking, alcohol, occupation, pollution, obesity, drugs, other comorbid conditions (hypertension, diabetes), etc. that can have an influence on semen parameters and reproductive potential of a male. Hence, in the future, we can do a study taking these factors also into consideration.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Oxidative stress and antioxidants for idiopathic oligoasthenoteratospermia: Is it justified? Indian J Urol. 2011;27:74-85.
- [Google Scholar]
- Consistent age-dependent declines in human semen quality: a systematic review and meta-analysis. Ageing Res Rev. 2015;19:22-33.
- [Google Scholar]
- Impact of age on semen parameters in male partners of infertile couples in a rural tertiary care center of central India: a cross-sectional study. Int J Reprod Biomed. 2017;15:497-502.
- [Google Scholar]
- WHO Laboratory Manual for the Examination and Processing of Human Semen (5th). Geneva: World Health Organization; 2010.
- Predictive value of abnormal sperm morphology in vitro fertilization. Fertil Steril. 1988;49:112-7.
- [Google Scholar]
- Paternal age and outcome of intracytoplasmic sperm injection. Reprod Biomed Online. 2007;14:588-92.
- [Google Scholar]
- The correlation between male age, sperm quality and sperm DNA fragmentation in 320 men attending a fertility center. J Assist Reprod Genet. 2009;26:41-6.
- [Google Scholar]
- Impact of paternal age on seminal parameters and reproductive outcome of intracytoplasmic sperm injection in infertile Italian women. Front Endocrinol (Lausanne). 2019;10:35.
- [Google Scholar]
- Semen quality pattern and age threshold: a retrospective cross-sectional study of 71,623 infertile men in China, between 2011 and 2017. Reprod Biol Endocrinol. 2019;17:107.
- [Google Scholar]
- Effects of male age on semen quality and fertility: a review of the literature. Fertil Steril. 2001;75:237-48.
- [Google Scholar]
- The effects of age on sperm quality: an evaluation of 1, 500 semen samples. JBRA Assist Reprod. 2014;18:34-41.
- [Google Scholar]
- The effects of male aging on semen quality, sperm DNA fragmentation and chromosomal abnormalities in an infertile population. J Assist Reprod Genet. 2011;28:425-32.
- [Google Scholar]
- The effects of age on DNA fragmentation, chromatin packaging and conventional semen parameters in spermatozoa of oligoasthenoteratozoospermic patients. J Assist Reprod Genet. 2007;24:437-43.
- [Google Scholar]
- Effect of age and abstinence on semen quality: a retrospective study in a teaching hospital. Asian Pac J Reprod. 2014;3:134-41.
- [Google Scholar]
- Semen quality and age-specific changes: a study between two decades on 3, 729 male partners of couples with normal sperm count and attending an andrology laboratory for infertility-related problems in an Indian city. Fertil Steril. 2010;93:2247-54.
- [Google Scholar]
- Comparison of semen quality in older and younger men attending an andrology clinic. Andrologia. 2002;34:116-22.
- [Google Scholar]
- The association of age and semen quality in healthy men. Hum Reprod. 2003;18:447-54.
- [Google Scholar]
- Age thresholds for changes in semen parameters in men. Fertil Steril. 2013;100:952-8.
- [Google Scholar]
- The effects of aging on semen parameters and sperm DNA fragmentation. JBRA Assist Reprod. 2020;24:82-6.
- [Google Scholar]
- Relationship between sperm mitochondrial membrane potential, sperm motility, and fertility potential. Asian J Androl. 2002;4:97-103.
- [Google Scholar]
- The effects of semen parameters and age on sperm motility of Iranian men. Glob J Fertil Res. 2017;2:24-9.
- [Google Scholar]







