Translate this page into:
Impact of peak serum estradiol levels on the outcomes of hormone replacement therapy (HRT) frozen embryo transfer (FET) cycles
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
With the improvised ovulation induction methods coming up, FET (Frozen Embryo Transfer) has gained preference over fresh transfers. Several strategies have been devised for preparing the endometrium for FET, out of which the hormone replacement regimen (HRT) with exogenous estrogen and progesterone supplementation still remains the most popular one. There are different clinical protocols for the transfer of frozen-thawed embryos. However, there has always been a debate about the impact of hyperestrogenism on endometrial development and implantation, particularly when controlled ovarian hyperstimulation is used in conjunction with fresh embryo transfers. We conducted this study with an objective to investigate the impact of variable serum estradiol (E2) levels achieved in the late follicular phase on implantation and pregnancy outcomes of cryopreserved/thawed embryos transferred in programmed cycles with exogenous hormonal replacement.
Keywords
FET (Frozen Embryo Transfer)
estradiol (E2)
estrogen
progesterone
INTRODUCTION
The percentage of frozen embryo transfer (FET) cycles is rapidly increasing across the world, due to a trend to transfer fewer embryos, improved cryopreservation techniques and elective oocyte cryopreservation.[1] Several strategies have been devised for preparing the endometrium during FET, including using ovulation during the natural process of follicle development and a hormone replacement regiments with exogenous estrogen and progesterone supplementation. There are different clinical protocols for the transfer of frozen–thawed embryos.[2] These include artificial cycles using hormone replacement therapy (HRT) in different administration routes, or ovulatory-based treatments that aim to achieve optimal endometrial preparation for embryo transfer or just a natural cycle FET.[3] In women with regular cycles, the natural cycle looks appealing as there is no extraneous hormonal intervention, but it requires thorough monitoring and there are occasional cancellations due to lack of ovulation. On the other side, in programmed cycles with hormonal replacement, efficient scheduling is a possible alternative and hence practically efficient for both ovulatory and anovulatory women, with only sporadic cancelations due to unwanted ovulation. However, there has always been a debate about the impact of hyperestrogenism on endometrial development and implantation, particularly when controlled ovarian hyperstimulation is used in conjunction with fresh embryo transfers.[4]
We conducted this study with an objective to investigate the impact of variable serum estradiol (E2) levels achieved in the late follicular phase on implantation and pregnancy outcomes of cryopreserved/thawed embryos transferred in programmed cycles with exogenous hormonal replacement.
AIMS AND OBJECTIVES
To evaluate the impact of serum E2 levels on cycle outcomes in hormone replacement FET cycles. Clinical pregnancy rates (CPRs) and ongoing pregnancy rates are primary outcomes.
Miscarriage rates (MRs) and live birth rates (LBRs) will be calculated as secondary outcomes in patients undergoing HRT FET cycles with monitoring of serum E2 levels.
MATERIALS AND METHODS
We conducted a center-based prospective study to include all patients undergoing HRT FET cycles at our center between October 2021 and February 2022. This number was 39. Following criteria were applied to include patients.
Inclusion criteria
All patients in reproductive age 18 to 40 years undergoing HRT FET cycle were included.
Exclusion criteria
Patients <18 years were excluded. Those with more than three in vitro fertilization/intracytoplasmic sperm injection failures were excluded too. Natural and stimulated FET cycles, donor FET cycles, and initiated artificial cycles without a subsequent embryo transfer were excluded.
The same artificial standard protocol was applied to all cycles.
Standard protocol
Exogenous estrogens are administered orally under the form of estradiol valerate (Progynova; Bayer Schering Pharma AG, Berlin, Germany). Supplementation is started on cycle day 2 after confirmation of basal serum hormonal values (for E2, Progesterone (P), and Luteinising Hormone (LH)). Routinely, a dose of 2 mg is prescribed thrice daily during the first 8 days. Cycle monitoring, with a first control visit planned on day 8 of endometrial preparation, with serum determinations of E2/P/LH and transvaginal ultrasound scans to assess the endometrial thickness. Second visit between day 10 and 14. If the endometrial lining is not found appropriate after 8 to 10 days of oral estrogen, transdermal E2 is added as 2 mg twice daily (Estogel Gel 80 gm [Estradiol-0.06%w/w, Intas Pharmaceuticals Ltd]). Serum E2 is measured on the day when targeted lining is achieved (thickness >7 mm). Serum progesterone assessments were used to detect escape ovulation and the cycle is cancelled when progesterone was 1.5 ng/mL or higher.
If the endometrial thickness was below 6.5 mm on day 14 of supplementation, patients were asked to follow a step-up protocol consisting of (1) prolonging the duration of the estrogen administration but adhering to the same dose via the oral route, (2) increasing the dose but adhering the oral administration route, or (3) adding transdermal estrogen administration (also estradiol valerate at a dose of 2 mg three times daily). If following the step-up protocol endometrial thickness did not reach 6.5 mm, the cycle was cancelled. Aqueous progesterone (AqSusten; Sun Pharmaceutical Industries Ltd, India; 25 mg subcutaneous, once daily) was used to induce the luteal phase. Once P supplementation was started, the estradiol valerate dose was decreased to 2 mg twice daily to mimic the natural cycle. Luteal phase support was continued until the time of the human chorionic gonadotropin (hCG) pregnancy test and prolonged until 12 weeks of gestation whenever positive.
All embryos are vitrified on day 3 or day 5 or 6 of embryo culture using the same vitrification protocol.
Cleavage stage day 3 embryos are warmed the day before FET and transferred as a day 4 embryo on the fourth day of P supplementation. Blastocysts were warmed and transferred on sixth day of P supplementation.
Biochemical pregnancy is defined as positive βhCG level without evidence of a gestational sac on ultrasound. Clinical pregnancy was defined as evidence of a gestational sac on ultrasound. Ongoing pregnancy was defined as intrauterine pregnancy with a heartbeat at 20 weeks or later. Peak serum E2 levels were considered the highest serum E2 level (pg/mL) obtained from initiation of the artificial FET cycle to the level immediately prior to progesterone supplementation, whereas average serum E2 levels (pg/mL) were the average of all serum E2 levels recorded from the initiation of the artificial FET cycle to the last level prior to progesterone supplementation.
Ethical Consideration
Ethical approval was sought and obtained from the institutional and Indian fertility society ethical committee. And the ref no was IEC/IFS/2021No.10.
RESULTS
Within the study period between October 2021 and February 2022, a total of 39 HRT FET cycles were done. Out of these, 24 patients showed a positive implantation and 15 had no implantation or a failed embryo transfer. Table 1 shows baseline characteristics of both these groups. The groups did not differ significantly regarding the majority of baseline characteristics, hence showing to be comparative. We divided the study patients in two groups with Group A having peak E2 levels <200 pg/dL and Group B with peak E2 levels >200 pg/dL. It was observed that in a normal menstrual cycle in the late follicular phase, the E2 levels reach around 200 mg/dL for ovulation to occur.

Hence, we divided the study population on this basis considering that these levels are more close to physiology.
Table 2 shows the comparison of implantation rates between groups A and B. Only one patient in group A achieved implantation. While 96% of the patients of the positive pregnancy group had peak E2 levels >200 mg/dL (group B) There was no statistical significance obtained (P value = 0.062).
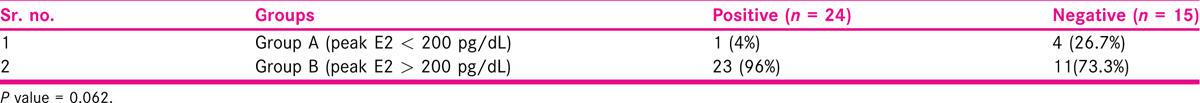
Table 3 shows the comparison of CPRs between groups A and B. Where, 22 (95.6%) out of 23 patients with a positive clinical pregnancy were in group B as compared to only one in group A. However, there was no statistical significance (P value = 0.173). Only one patient had a miscarriage from group B.

DISCUSSION
This was a prospective study conducted at Ridge IVF, Gouri Hospital, Delhi, India. This can be considered as a pilot study as we could bring up results of only 40 patients undergoing HRT FET cycle due to time limits.
Our findings were similar to those of Garimella etal., who in their retrospective study found that the outcomes of FET cycles were similar over a wide range of E2 values (100–500 pg/mL). However, when E2 levels were <100 pg/mL or >500 pg/mL there was significant increase in the MRs, but the numbers in these groups were less.[5]
Similarly, Özdemir etal. in their retrospective study found that it is not necessary to monitor E2 levels in HRT cycles. They used oral E2 to prepare endometrium and measured outcomes in terms of clinical and ongoing pregnancy rates.[6]
However, there were studies that had different findings. Fritz etal.[7] in their retrospective study found that elevated E2 levels in HRT FET cycles could negatively impact ongoing pregnancy and LBRs, probably due to adverse effect on the endometrium from excess unopposed E2 exposure. We divided the patients on basis of peak E2 of 200 mg/dL.
There was only one miscarriage which was from a biochemical pregnancy.
The main limitation of our study was small sample size as the study period was just 5 months and it was a prospective study. There was a significant dip in FET cycles as there was the third wave of COVID-19 in this time period.
CONCLUSION
Our study showed no impact of peak E2 levels on the outcomes of HRT FET cycles in terms of implantation and CPRs. A larger sample size may show different results and hence advised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- What is the optimal means of preparing the endometrium in frozen-thawed embryo transfer cycles? A systematic review and meta-analysis. Hum Reprod Update. 2013;19:458-70.
- [Google Scholar]
- Cycle regimens for frozen-thawed embryo transfer. Cochrane Database Syst Rev. 2017;7:CD003414.
- [Google Scholar]
- Clinical evidence for a detrimental effect on uterine receptivity of high serum estradiol levels in high and normal responder patients. Hum Reprod. 1995;10:2432-4.
- [Google Scholar]
- Does serum estrogen level have an impact on outcomes in hormonal replacement frozen-warmed embryo transfer cycles? Gynecol Endocrinol. 2021;37:891-4.
- [Google Scholar]
- Does high estrogen level negatively affect pregnancy success in frozen embryo transfer? Arch Med Sci. 2022;18:647-51.
- [Google Scholar]
- Elevated serum estradiol levels in artificial autologous frozen embryo transfer cycles negatively impact ongoing pregnancy and live birth rates. J Assist Reprod Genet. 2017;34:1633-8.
- [Google Scholar]







