Translate this page into:
Retrospective analysis on the effect of duration of ejaculatory abstinence on fertilization, embryo development, and pregnancy rates in patients undergoing conventional in vitro fertilization
Address for correspondence: Dr Sweta Gupta, Medicover Healthcare Private Limited, E-20, Panchsheel Park, New Delhi 110017, India. E-mail: Swetagupta06@yahoo.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Aim:
This study aims to find out how different sexual abstinence period influences semen parameters, fertilization, embryo development, and pregnancy rates in patients undergoing conventional in vitro fertilization.
Setting and designs:
A retrospective analysis was conducted at a tertiary level infertility care clinic.
Materials and methods:
The clinical study included 532 patients between January 2017 and July 2021 who had been treated with conventional in vitro fertilization. The effect of sexual abstinence on primary outcomes such as semen volume, total sperm concentration, total motile sperm concentration, sperm morphology, and secondary outcomes such as fertilization rate, cleavage rate, top quality day 3 and day 5 embryo development rate, implantation and clinical pregnancy rate between fresh versus frozen embryo transfer on day 3 and day 5 of conventional in vitro fertilization under three groups, that is, sexual abstinence of less than or equal to 1, 2 to 5, and 6 to 7 days was evaluated.
Statistical analysis used:
Chi-square test was used to evaluate the qualitative variables whereas one-way analysis of variance was used to evaluate the quantitative variables.
Results:
Group II with 2 to 5 days of abstinence, observed a positive correlation between abstinence period and semen volume, total sperm concentration, total motile sperm concentration, and morphology. Fertilization rate was higher in groups II and III than group I (P = 0.21) with no significant difference in cleavage rate (P = 0.4) and embryo development on day 3 (P = 0.1057). The formation of AA grade blastocyst between group I and group II was 27.54 % and 23.47 %, respectively, with a P-value of 0.007154. Both fresh and frozen embryo transfers of groups II and III of abstinence period had implantation and clinical pregnancy rates of 23.39% and 43.83%, respectively.
Conclusion:
Our study did not find any significant difference in primary and secondary outcomes of conventional in vitro fertilization between the three groups. We recommend further prospective large randomized control studies to prove any association between duration of abstinence and pregnancy outcomes.
Keywords
Conventional in vitro fertilization
ejaculatory abstinence
infertility
semen parameters
INTRODUCTION
Infertility is quite common at present and is a major cause of concern for 70 million people around the world. World Health Organization (WHO) estimates that 15% of couples in the total population are facing infertility problems, of which 40% of the cases are due to male factors.[1,2,3,4,5] Hence, to confirm the presence of the male factor and to regularize the semen analysis worldwide, we have accepted many recommendations from WHO Laboratory Manuals for the examining of human semen over the past two decades. These recommendations have helped in setting up a reference value in the assessment of basic semen parameters globally.
Many factors including abstinence, routine ejaculation, scrotal conditions, surgery, genital or urinary tract infections, general health status, lifestyle, and medications have a negative impact on semen parameters.[6] Even long physiologic duration of spermatogenesis or any intervention in spermatogenesis can also impair semen parameters.[7,8] All these factors result in variation in semen parameters during the assessment. Therefore, one should not expect to get a full analysis view of semen quality just by assessing only one semen sample, whereas other groups suggested analysis of two or more semen samples to reduce the variations in some of the known parameters. At present, the formal recommendation from WHO regarding the abstinence period for semen analysis is 2 to 7 days.[4] However, this duration is not supported by the European Society of Human Reproduction and Embryology and Nordic Association for Andrology guidelines which are in favor of a narrower abstinence period, that is, from 3 to 4 days.[9]
Several studies have been carried out to evaluate the duration of the abstinence period on clinical outcomes. A few studies have depicted higher pregnancy rates in intrauterine insemination (IUI) with no detrimental effects on semen parameters when semen sample from a shorter period of abstinence was used[10] but a negative impact was observed when abstinence was less than 24 hours.[11] Some studies have shown that an increased period of abstinence may result in higher sperm concentration with poor motility.[12] An earlier study has shown that a shorter abstinence period may lead to sperm chromatin immaturity and negatively affect DNA integrity.[13] Prolonged storage of sperm inside the epididymis negatively affects its motility, but the exact duration of storage for good morphologically and motile sperm is still not clear.[14] Seminal volume may decrease with more frequent ejaculations with no significant effects on sperm concentration, motility, morphology, or vitality.[15] A recent study performed in 2018[16] showed that ejaculatory abstinence of less than 4 days had significantly higher fertilization, good quality embryos on day 3, blastocyst development, and pregnancy rates when compared with an abstinence period of more than 4 days after intracytoplasmic sperm injection (ICSI) but similar results may not be expected from conventional in vitro fertilization (IVF). Our previous study found a significant correlation between an improved clinical pregnancy rate and a decreased abortion rate with lower abstinence duration.[17]
Therefore, on the basis of our previous study on ICSI cycles, we wanted to observe how abstinence duration influences semen parameters, fertilization, embryo development, and pregnancy rates in IVF cycle.
MATERIALS AND METHODS
Methodology of the study
A clinical study of 532 patients treated with conventional IVF has been retrospectively evaluated at a tertiary infertility clinic between January 2017 and July 2021. The study was agreed upon by the Institutional Ethical Committee (MCRM/01/2021). Consents were duly signed by the couples, and ethical ideals were obeyed as specified by the Helsinki Declaration (2013). During the evaluation, a total of 31 cycles with fertilization failure (n = 10) and no embryo cleavage (n = 21) were excluded from the study. Finally, the whole evaluation of 501 patients who had undergone conventional IVF was performed.
Inclusion criteria
Subfertile couples with a history of primary or secondary infertility were included in this study. Male partners with an age between 25 and 45 years with normal body mass index (BMI), who were able to provide a semen sample on the day of ovum pickup through masturbation with normal semen parameters and female partners with an age of 25 to 38 years with normal ovarian reserve (Anti-Müllerian hormone), were the part of this study. Initial infertility workup for both the partners was carried out.
Exclusion criteria
Male partners having a history of lifestyle disease (diabetes mellitus, hypertension, thyroid, and mumps) or any other medical disease [tuberculosis, varicocele, sexually transmitted disease (STD), undescended testis, congenital absence of vas deferens, or genetic and/or chromosomal abnormalities], and abnormal semen parameters (oligozoospermia, asthenozoospermia, teratozoospermia, oligoasthenoteratozoospermia, azoospermia, or aspermia) were excluded from the study. Females with poor ovarian reserve, no oocytes retrieved on the day of ovum pickup, activation of oocytes, or diagnosed with the polycystic ovarian syndrome, endometriosis, unexplained infertility were excluded from the study.
Ovarian stimulation protocol
All females had undergone controlled ovarian stimulation through gonadotropin-releasing hormone-antagonist regimen. The dose of gonadotropins was started from 150 IU to 375 IU and later adjusted according to the response of the ovarian follicular development, which was monitored via vaginal ultrasonography. When the follicles had reached 18 mm in diameter, all drugs were discontinued and trigger with ovitrelle 0.25 mg sc was administered. Oocyte retrieval was performed via vaginal ultrasound-guided 17 G follicle aspiration needle, 36 hours after trigger administration.
Semen collection and preparation
The semen sample was collected in a sterile wide-mouthed plastic container through masturbation. Before sample collection, all-male partners were advised to sign consent forms and to provide details of their age, BMI, ejaculatory abstinence, lifestyle habits, and disorders. Semen analysis was performed according to the WHO 2010 criteria. Semen preparation was carried out using the discontinuous density gradient method (Pure Sperm density gradient; SAR Healthline Pvt. Ltd., Chennai, Tamil Nadu, India) followed by the swim-up method. To find out the effect of ejaculatory abstinence on primary outcomes including semen parameters such as semen volume, sperm concentration, total motile sperm concentration, sperm morphology, and secondary outcomes including fertilization rate, cleavage rate, day 3 and day 5 top quality embryo development rate, implantation, and clinical pregnancy rate between fresh versus frozen embryo transfer (FET) on day 3 and day 5 of conventional IVF, patients were divided into three groups, that is, group I – 0 to 1 day, group II – 2 to 5 days, and group III – 6 to 7 days of abstinence period.
Method for fertilization and embryo development
All cumulus–oocyte complexes retrieved through ovum pickup were subjected to conventional in vitro insemination with a husband’s processed semen sample after 2 hours of incubation in 1 mL of continuous single culture medium (CSC-NX complete medium from FUJIFILM Irvine Scientific, Santa Ana, CA, USA). Fertilization was assessed after 17 + 1 hours postinsemination based on the presence of two pronuclei and two polar bodies. All fertilized oocytes were then cultured in droplet culture using the same culture medium. Embryo developed on days 2, 3, and 5 were assessed based on the Istanbul consensus workshop for embryo assessment (2011).[18]
Grade A
Day 2: 2 to 4 even size blastomeres with ≤10% fragmentation
Day 3: 6 to 8 even size blastomeres with ≤10% fragmentation
Day 5: ICM – Prominent, easily discernible, with many cells that are compacted and tightly adhered together
Trophectoderm – Many cells form a cohesive epithelium
Grade B
Day 2: 2 to 4 even or uneven size blastomeres with 10% to 20% fragmentation
Day 3: 6 to 8 even or uneven size blastomeres with 10% to 20% fragmentation
Day 5: ICM – Easily discernible, with many cells that are loosely grouped together
Trophectoderm – Few cells forming a loose epithelium
Grade C
Day 2 and 3: Uneven and few blastomeres with >20% fragmentation
Day 5: ICM – Difficult to discern, with few cells
Trophectoderm – Very few cells
Embryo vitrification and thawing
In most of the cycles, either day 3 or day 5 embryos were cryopreserved, whereas in a few cycles, both day 3 and day 5 embryos were cryopreserved. Thawing of embryos was performed a minimum of 2 hours before FET. Both vitrification and thawing of embryos were carried out using the Kitazato vitrification and thawing kit (Kitazato Co., Fuji city, Shizuoka, Japan).
Frozen embryo transfer
For FET, baseline scan and hormonal assessment on days 2/3 of periods were performed to check the thickness of the endometrium, and when the endometrium reached 8 mm in thickness with a triple line, progesterone was supplemented. Under ultrasound guidance, vitrified-warmed day 3 cleavage stage embryos or day 5 blastocyst embryos were transferred transvaginally using a 17.3-cm soft embryo transfer (ET) catheter (COOK K-JETS-7029-SIVF). Depending on the female’s age and the number of previous cycle failures, maximum of 2-3 × day 3 or 2 × day 5 embryos were transferred in 1 mL of conventional culture medium in each group.
Fresh ET on day 3 was carried out in cases with less number (≤4) of embryos available on day 3.
Statistical analysis
To perform the statistical analysis of the whole study data, the Chi-square test was used to evaluate the qualitative variables, whereas one-way analysis of variance was used to evaluate the quantitative variables. A P-value of <0.001 was regarded as statistically significant. The SPSS Statistical software (Released 2012, IBM SPSS Statistics for Windows, Version 21.0; IBM Corp, Armonk, NY, USA) was used to do the whole statistical analysis.
RESULTS
The study included a total of 532 IVF cycles, seeking infertility treatment at a tertiary infertility clinic. The method of fertilization for the foregoing cohort was conventional insemination. A total of 6085 oocyte cumulus complexes (OCCs) were retrieved through ovum pickup after controlled ovarian hyperstimulation. Out of these total retrieved OCCs, 4907 were directed for conventional IVF, whereas the remaining were inseminated through ICSI, which were excluded from the study. An overview of the study is summarized in Table 1.

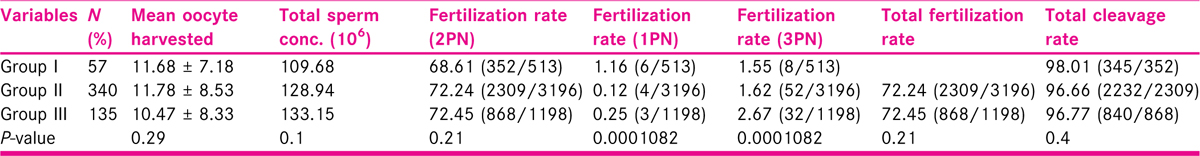
To compare the effects of ejaculatory abstinence on primary and secondary outcomes, the whole cohort was divided into three groups based on the duration of abstinence. Patients in group I had a ≤1-day abstinence period (n = 57), patients in group II had a 2- to 5-day abstinence period (n = 340), and patients in group III had a 6- to 7-day abstinence period (n = 135). To begin, the primary outcomes were measured among the three groups, focusing on macro- and microscopic semen characteristics such as semen volume, total sperm concentration, and total motile sperm concentration [Table 2]. A significantly higher semen volume along with total sperm concentration and total motile sperm concentration per ejaculate was observed in group III than in groups I and II. Average semen volume and average sperm concentration were recorded as 2.5 mL and 56.84 × 106/mL, respectively. Morphologically good sperms were retrieved in group I with a minimum abstinence period.

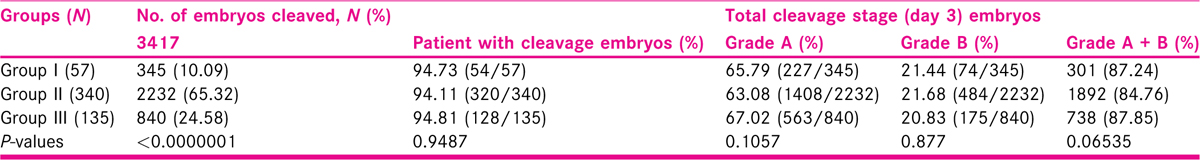
The secondary outcomes, such as fertilization rate, cleavage rate, and top quality day 3 and day 5 embryo development rate, were measured and are summarized in Tables 3 to 5. A total fertilization rate of 71.91% and a total cleavage rate of 96.82% were noticed across the study. Based on the abstinence period among the three groups, there was no significant difference between the fertilization and cleavage rate. However, groups II and III showed a slightly higher fertilization rate than group I, but that was also not significant enough to be recorded. The development of top quality day 3 embryos was not eminent in any of the three groups, whereas the sum of day 3 grade A and grade B embryos was only marginally distinguished in groups I and III. Development of top quality grade AA blastocyst on day 5 was significantly higher in group I than the other two groups, with no difference in the development of grades AB, BA, and BB blastocyst among the three groups. Also, the overall blastocyst development rate was higher in group I.
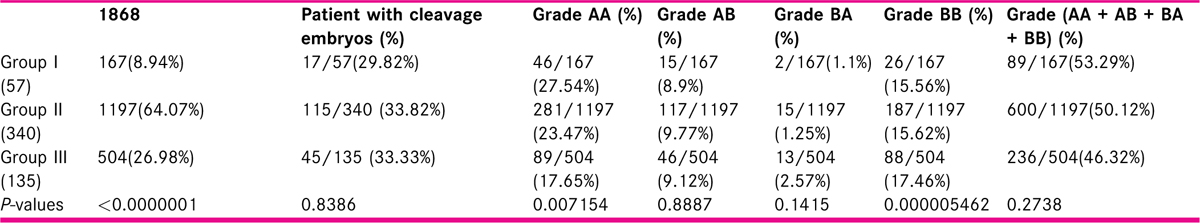
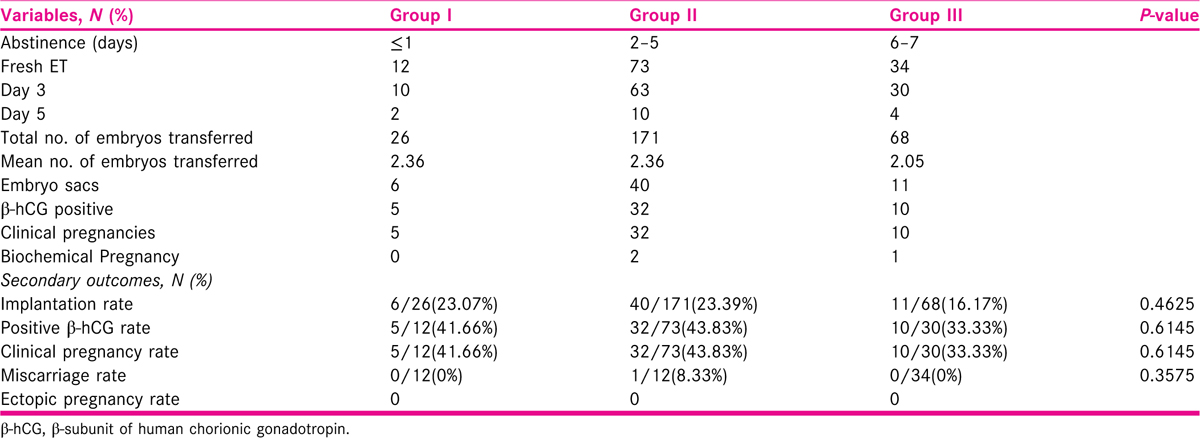
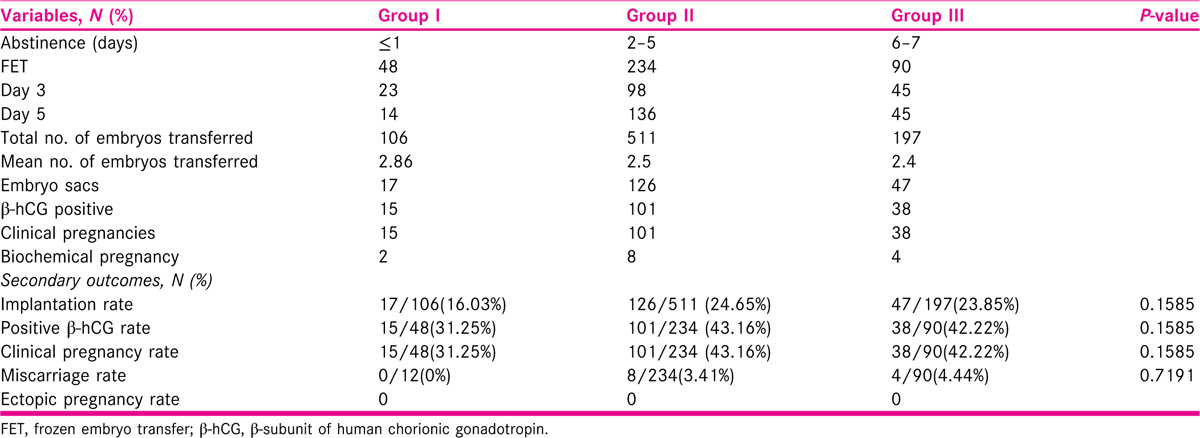
Further, secondary outcomes were analyzed by evaluatingcycles with 120 fresh ETs and 373 FET on days 3 and 5. Out of 120 fresh ETs, 104 were carried out on day 3 and 16 were carried out on day 5, whereas in 373 FETs, 161 were carried out on day 3, and 163 were carried out on day 5. A total of 269 days 3 and 5 embryos were transferred in Fresh ET cycles, and 814 embryos were transferred in FET cycles. Among all the groups, the maximum number of 73 (60.83%) fresh ET was performed with 171 top-quality embryos, and 234 (62.73%) FET with 511 top-quality embryos was performed in group II. In fresh ET cycles, a slightly higher implantation rate of 23.39%, β-subunit of human chorionic gonadotropin (β-hCG) positivity rate of 43.83%, and a clinical pregnancy rate of 43.83% were observed in group II than in groups I and III. For group I, these values were 23.07%, 41.66%, and 41.66%, respectively, and for group III, these values were 16.17%, 33.33%, and 33.33%, respectively. However, group II noticed a maximum miscarriage rate of 8.33%. In FET cycles, group II had a higher implantation rate, β-hCG positivity rate, and clinical pregnancy rate than groups I and III, at 24.65%, 43.16%, and 43.16%, respectively. There was no significant difference in miscarriage rates between groups II and III (3.41% vs. 4.44%). Moreover, there was no evidence of ectopic pregnancy in either fresh ET or FET cycles.
In FET cycles, implantation rate, β-hCG positivity rate, and clinical pregnancy rate were again higher in group II than in groups I and III, i.e., 24.65%, 43.16%, and 43.16%, respectively. There was no significant difference in miscarriages rates between groups II and III (3.415% vs. 4.44%). Moreover, there was no evidence of ectopic pregnancy in either fresh ET or FET cycles [Tables 6 and 7].
DISCUSSION
With reference to the following study, it was observed that having a longer abstinence period increases semen volume and sperm concentration. A significantly higher seminal volume and total sperm concentration were noted in group III when compared with the other two groups, which is consistent with previous studies.[19,20,21] Frequent ejaculations result in low sperm concentration along with lower levels of sperm chromatin maturity. Some studies have associated increased sperm DNA damage with a longer abstinence period.[22] Thus, the effect of abstinence period on semen quality needs more recommendations or evidence to reach a comprehensive analysis.
In IUI cycles, previous studies have found a higher pregnancy rate when the abstinence period was ≤3 days.[23,24] A similar higher pregnancy rate was achieved in ICSI cycles, when the abstinence period was not more than 3 days. Conversely, the highest total motile sperm count was observed after 7 days of abstinence but similar results were not observed when pregnancy was considered.[24] Total motile sperm count was formerly thought to be the most important predictor of conception in IUI cycles but several studies have shown that even with lower motile sperm counts, higher pregnancy rates can be achieved.[25] However, a retrospective and observational study found that pregnancy rates are higher in groups with 4 to 7 days of abstinence than in groups with 1 to 4 days of abstinence.[26] As a result, comparing pregnancy rates in IUI cycles based on different abstinence periods is quite inconsistent, and further research is needed before a conclusion can be reached.
Secondary outcomes in conventional IVF or ICSI cycles were also inconsistent across abstinence study groups.[27] Some studies have shown that short-term abstinence had a positive effect on fertilization and pregnancy rates.[28] Despite these diverse conclusions, it could never be stated that couples with shorter abstinence periods have lower pregnancy rates than high abstinence period couples or vice-versa. With conventional IVF, no specific difference was reported in fertilization and cleavage rates. Our present study, too, shows no statistical difference between fertilization, cleavage, development of good quality days 3 and 5 embryos, implantation, and clinical pregnancy rates. Almost similar fertilization and cleavage rates were obtained in all three study groups. Development of top quality day 3 embryos and day 5 blastocyst was higher in group I, whereas the implantation rate and clinical pregnancy rate were higher in group II. Neither a positive nor a negative effect of a shorter or longer abstinence period was observed in couples undergoing conventional IVF. Moreover, in conventional IVF, oocyte naturally selects competent spermatozoa for fertilization and synchronized embryo development, and this could be one of the reasons that we might not see any significant difference in fertilization and cleavage rates when compared with ICSI.
There are not many similar studies in literature, and therefore, this study becomes relevant. We did not notice any significant difference which could be due to small number of patients in all groups. Another limitation was that this study was retrospective. We therefore suggest larger prospective studies in future to know the exact effect of ejaculatory abstinence on the fertilization rate, embryo development rate, and pregnancy outcomes of patients undergoing IVF.
CONCLUSION
In conclusion, an abstinence period of 2 to 5 days is appropriate as it is neither too short nor too long and provides a sample with improved sperm concentration, motility, morphology, and increased sperm maturity with potential clinical benefits for conventional IVF outcomes. Our present study did not find any significant difference in primary and secondary outcomes after conventional IVF between the groups of different abstinence. Further larger studies are required to define the optimum abstinence interval within the sexual abstinence period.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Laboratory Manual for the Examination of Human Semen andSemen-Cervical Mucus Interaction. Singapore: Press Concern; 1980.
- WHO Laboratory Manual for the Examination of Human Semen and Sperm-Cervical Mucus Interaction (3rd). Cambridge, UK; New York, NY, USA: Published on behalf of the World Health Organization by Cambridge University Press; 1992.
- WHO Laboratory Manual for the Examination of Human Semen and Sperm-Cervical Mucus Interaction (4th). Cambridge, UK; New York, NY, USA: Published on behalf of the World Health Organization by Cambridge University Press; 1999.
- WHO Laboratory Manual for the Examination and Processing of Human Semen (5th). Geneva, Switzerland: World Health Organization; 2010.
- Laboratory Manual for the Examination of Human Semen and Semen-Cervical Mucus Interactions (2nd). Cambridge, UK: Cambridge University Press; 1987.
- Influence of analytical and biological variation on the clinical interpretation of seminal parameters. Hum Reprod. 2006;21:847-51.
- [Google Scholar]
- Causes of Male Infertility. Berlin, Germany: Springer Science and Business Media LLC; 2020. p. :3-14.
- Effects of ejaculatory frequency and season on variations in semen quality. Fertil Steril. 2004;82:358-366.
- [Google Scholar]
- Nordic Association for Andrology; European Society of Human Reproduction and Embryology. Special Interest Group on Andrology. Manual on Basic Semen Analysis. In: ESHRE Monographs. Oxford, MA, USA: ESHRE by Oxford University Press; 2002.
- [Google Scholar]
- Effect of sexual abstinence on pregnancy rates after an intrauterine insemination. Ginecologia Y Obstetricia De Mexico. 2015;83:104-9.
- [Google Scholar]
- Influence of the abstinence period on human sperm quality. Fertil Steril. 2004;82:57-65.
- [Google Scholar]
- The impact of ejaculatory abstinence on semen analysis parameters: a systematic review. J Assist Reprod Genet. 2018;35:213-20.
- [Google Scholar]
- Sperm chromatin immaturity observed in short abstinence ejaculates affects DNA integrity and longevity in vitro. PLoS One. 2016;11:e0152942.
- [Google Scholar]
- Influence of ejaculation frequency on seminal parameters. Reprod Biol Endocrinol. 2015;13:47.
- [Google Scholar]
- Revisiting the impact of ejaculatory abstinence on semen quality and intracytoplasmic sperm injection outcomes. Andrology. 2018;7:213-9.
- [Google Scholar]
- Short ejaculatory abstinence in normozoospermic men is associated with higher clinical pregnancy rates in sub-fertile couples undergoing intra-cytoplasmic sperm injection in assisted reproductive technology: a retrospective analysis of 1691 cycles. J Hum Reprod Sci. 2021;14:273-80.
- [Google Scholar]
- The Istanbul consensus workshop on embryo assessment: proceedings of an expert meeting. Alpha Scientists in Reproductive Medicine and ESHRE Special Interest Group of Embryology. Hum Reprod. 2011;26:1270-83.
- [Google Scholar]
- Revisiting the impact of ejaculatory abstinence on semen quality and intracytoplasmic sperm injection outcomes. Andrology. 2019;7:213-9.
- [Google Scholar]
- Analysis of semen parameters during 2 weeks of daily ejaculation: a first in humans study. Transl Androl Urol. 2016;5:749-55.
- [Google Scholar]
- Effects of ejaculatory frequency and season on variations in semen quality. Fertil Steril. 2004;82:358-66.
- [Google Scholar]
- Influence of the abstinence period on human sperm quality: analysis of 2,458 semen samples. JBRA Assist Reprod. 2017;21:306-12.
- [Google Scholar]
- Effect of ejaculatory abstinence period on the pregnancy rate after intrauterine insemination. Fert Steril. 2005;84:678-81.
- [Google Scholar]
- A short period of ejaculatory abstinence before intrauterine insemination is associated with higher pregnancy rates. Fert Steril. 2010;93:286-8.
- [Google Scholar]
- The effect of male sexual abstinence periods on the clinical outcomes of fresh embryo transfer cycles following assisted reproductive technology: a meta-analysis. Am J Mens Health. 2020;14:1557988320933758.
- [Google Scholar]
- Effect of sexual abstinence on pregnancy rates after an intrauterine insemination. Ginecologia y obstetricia de Mexico. 2015;83:104-9.
- [Google Scholar]
- Influence of abstinence period on clinical outcomes in fresh embryo transfer after intracytoplasmic sperm injection. Fert Steril. 2015;104:e292.
- [Google Scholar]
- Influence of sexual abstinence length on sperm parameters and on IVF outcomes in ICSI assisted treatment cycles. Fert Steril. 2007;88:S252.
- [Google Scholar]







