Translate this page into:
The Impact of Magnetic Activated Cell Sorting (MACS) on Assisted Reproduction Outcomes

*Corresponding author: Dr Raiheen K P, MS, DNB (OBG), Department of Reproductive Medicine, ARMC Aegis Hospital, Perinthalmanna, India. raihykp@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: KP R, KU K, Seethi F, Subhash VV, The Impact of Magnetic Activated Cell Sorting (MACS) on Assisted Reproduction Outcomes. Fertil Sci Res. 2024;11:10. doi: 10.25259/FSR_10_2024
Abstract
Objectives
The study’s objectives were to evaluate the benefits of adding the magnetically activated cell sorting (MACS) technique to the traditional density gradient sperm wash method for advanced sperm selection in intracytoplasmic sperm injection (ICSI) cycles by comparing fertilisation rates, embryo quality, blastocyst formation, and pregnancy rates.
Material and Methods
A retrospective observational study was conducted at ARMC Aegis Hospital Perinthalmanna, Kerala. The study group was 116 patients taken during ICSI cycles done from October 2021 to September 2023, with 58 patients in the study (MACS after density gradient centrifugation) and 58 in control (density gradient centrifugation alone). Cases and controls were determined by the willingness of the patient to do MACS in sperm selection after discussion with their clinician. Patients with a severe male factor with sperm morphology <4% were included in the study, with the female partner having regular cycles, normal AFC, and AMH > 1 ng/ml. Patients with seminal infection, known genetic errors, female partners with endometriosis, PCOS, infections, malformations and previous poor responders were excluded. Spermatozoa are incubated with microbeads for 15 min at room temperature (100 μl/10 million) in MACS, after which they are placed into a separation column that contains magnetised iron spheres in it that is magnetised. While the unlabelled cells flow through the MACS column, the micro-bead labelled cells are trapped there subsequently, ICSI was performed using the processed sperm sample. The 2PN (Pro-nuclei) embryos, blastocysts, embryo quality, clinical pregnancies, and live births were noted and statistically analysed.
Results
The study and control groups were demographically similar; both cases (MACS group) and control group Density Gradient Centrifugation (DGC) group were under a 95% confidence interval. Results of the MACS group were compared with the DGC group. 2 PN status, number of embryos, Grade I embryos, day 5 blastocyst formation, live birth rates, and the number of positive pregnancies were examined in both groups. Analysis showed an increase in the 2 PN status, number of embryos, Grade I embryos, and day 5 blastocyst formation in the MACS group compared to the conventional DGC method. However, embryo grades (Grade I embryos) in the MACS group were high compared to the DGC group (P-value < 0.01).
Conclusion
For couples with severe male factors and defective sperm morphology, the study finds that MACS may be recommended as an additional option to standard sperm processing.
Keywords
Magnetic Activated Cell Sorting (MACS)
Density Gradient Centrifugation (DGC)
INTRODUCTION
The efficacy of assisted reproduction technology (ART) hinges on the quality of gametes employed in fertility treatment cycles. Nevertheless, in most of instances, seminal quality is still assessed only using conventional semen analysis. Because of its unpredictability and lack of specificity, this method is not very efficient in detecting functional changes or determining the cause of sperm abnormalities.[1]
An examination of sperm DNA fragmentation is a highly promising method for diagnosing male infertility.[2] Multiple meta-analyses have shown that the preservation of DNA integrity is essential for the proper development of embryos[3,4] as well as for successful implantation and the continuation of pregnancy.[5-7] The primary factors responsible for single- or double-stranded DNA fragmentation in spermatocytes are changes in apoptotic processes, abnormalities in DNA remodelling during spermatogenesis, and oxidative damage in the epididymis.[8,9]
Apoptosis is a natural mechanism that removes defective sperm cells to maintain a balanced population of germ cells and ensure sufficient nutrients in the testicles.[10] Apoptosis is strongly associated with unsuccessful implantation and spontaneous abortions.[11] Sertoli cells can differentiate and remove sperm cells that have apoptotic signals, such as phosphatidylserine (PS) residues, on their outer plasma membrane. Dysfunction of Sertoli cells or excessive activity of testicular apoptotic processes, also known as abortive apoptosis, can hinder the removal of apoptotic cells during sperm production and hence lead to an increase in the number of dead sperm cells in the ejaculate.[12]
Under normal physiological conditions, phagocytes in the female genital tract can identify and effectively eliminate apoptotic sperm cells with externalised PS residues on the plasma membrane,[13] preventing a spermatozoon with altered DNA integrity from fertilising the oocyte.[14] When ART sperm-selection techniques like density gradient centrifugation or sperm swim-up are used, this crucial sperm-selection process is inconveniently circumvented. In intracytoplasmic sperm injection (ICSI) cycles, the embryologist’s subjective preference for the best sperm morphology determines which viable spermatozoon would be injected into an oocyte.
Recently, many methods for selecting sperm have been discovered that can initiate the processes involved in sperm-cell capacitation. One such is the magnetically activated cell sorting (MACS) technique, which uses Annexin V-conjugated superparamagnetic microbeads to recognise externalised PS residues on apoptotic sperm cells.[15-17] This technique is utilised to positively eliminate apoptotic cells from ejaculation.[18] By adopting this method, the percentage of sperm with fragmented DNA in the ejaculate is also decreased before ART operations.[19]
Numerous articles have supported the MACS selection strategy as a helpful way to lower the quantity of apoptotic sperm, enhancing overall embryo quality and increasing the likelihood of conception.[20,21] Many authors have failed to demonstrate a significant improvement in using MACS versus conventional sperm-selection techniques.[22,23] Additionally, male factors have not been taken into account in patient selection criteria or demographic studies.
Various studies have shown that the sperm DNA fragmentation index, as measured by different methods, might not predict assisted reproductive outcomes.[24]
Recent studies have shown that aneuploidy in spermatozoa of infertile men with poor semen quality is increased. The results suggest that poor sperm morphology is associated with numerical chromosome abnormalities of spermatozoa.[25] There were no significant differences in IVF and ICSI fertilisation rate, good embryo rate, and pregnancy rate (PR) between high, moderate, and low DFI groups.[26] Embryonic development and clinical outcomes after Frozen Embryo Transfer (FET) were equivalent for low and high DNA Fragmentation Index (DFI) groups using ICSI or IVF. However, sperm DFI did not provide sufficient information regarding embryo development or clinical outcomes for infertile couples using FET.[27]
This study examines if using the MACS sperm selection approach, as opposed to the traditional density gradient centrifugation sperm wash method, could enhance the reproductive result in individuals with severe teratozoospermia.
MATERIAL AND METHODS
Objective
To evaluate the benefits of adding the MACS technique to the traditional density gradient sperm wash method for advanced sperm selection in ICSI cycles by comparing fertilisation rates, embryo quality, blastocyst formation, and pregnancy outcomes.
This study, which was carried out in Kerala’s ARMC Aegis Hospital Perinthalmanna, is a retrospective observational study. All Patients undergoing ICSI cycles from October 2021 to September 2023 were included in the study. The sample size was calculated as a total of 116, with 58 each in 2 groups using a similar study population in another study.
The sample size was calculated using the formula
p = (p1+rp2)/(1+r)
r = ratio of grp 1/ grp 2 = 1
where Zα/2 is the critical value of the normal distribution at α/2 (e.g., for a 95% confidence level, α is 5% and the critical value is 1.96), Zβ is the critical value of the normal distribution at β . For a power of 80%, β is 20% and the critical value is 0.84.
According to the previous study ‘Utility of MACS in assisted reproduction’ done by Adel Abou et al.[28], the blastocyst formation rate in MACS group and the control group was 38.3% and 63.9% respectively. The estimated sample size was found to be 116, with 58 in case group and 58 in control group.
Inclusion Criteria
Male partners with normal sperm morphology <4% in semen analysis before processing.
Semen analysis total sperm concentration 1–15 million/ml, 5–20% actively motile sperm.
Male partners are between 25 and 45 years, and female partners are between 21 and 35 years.
Female partners with regular cycles, AFC5-12, AMH 1-6.8 ng/ml.
Exclusion Criteria
Any partner with known genetic errors.
H/o current seminal infection on culture and senstivity [Figure 1].
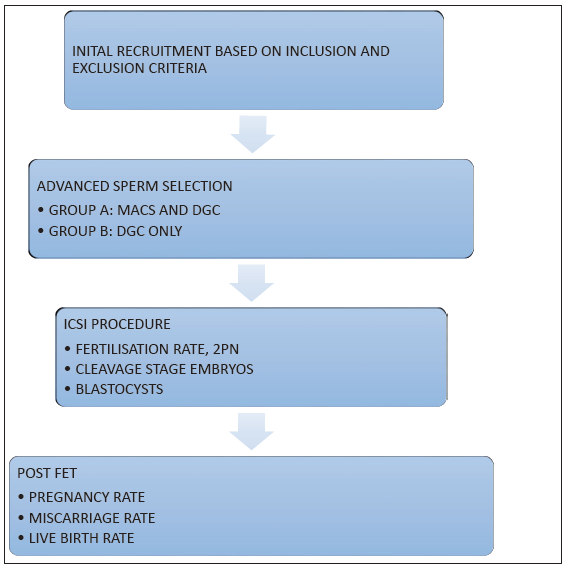
- Study Workflow. AMH: Anti-Mullerian Hormone; SA: Semen Analysis, PN: pronuclei; MACS: Magnetic Activated Cell Sorting; DGC: Density Gradient Centrifugation; ICSI: Intracytoplasmic Sperm Injection.
Female partner with severe endometriosis, PCOS, PID, uterine malformations, and poor ovarian reserve.
The male partners were considered for advanced sperm selection if they had mild oligasthenozoospermia with teratozoospermia in semen analysis. The option of using MACS was provided to the couple after counselling regarding its potential benefits and weighing the affordability with the benefits. The ICSI cycles used self-oocyte only.
The study group consisted of patients for whom sperm selection was done using MACS in addition to the conventional density gradient sperm wash method. The control group consisted of patients for whom sperm processing was done by conventional density gradient method only. Semen analysis was done as per WHO 6th edition (2021) standards.
DGC (Density Gradient Centrifugation)
The count and motility of the semen sample were examined beforehand. In a centrifuge tube, 1 ml of lower-phase media (80%) was added, and 1 ml of upper-phase media (40%) was carefully put on top. The tube was maintained at 37°C for 15–30 min. In parallel, 2.5 ml of sperm wash medium was added to the bottom tube and heated for 15–30 min to 37°C. In parallel, 2.5 ml of sperm wash medium was added to the bottom tube and incubated at 37°C for 15-30 minutes. The liquefied semen sample was carefully placed on top of the warmed tube and centrifuged for 20 min at 1800 rpm. The supernatant was then disposed of. The leftover pellet was combined with 2 ml of sperm wash medium, well mixed, and centrifuged for 10 min at 1600 rpm. Once again, the supernatant was discarded, and the pellet was combined well with 0.5 ml of heated sperm wash medium well. This post-wash sample was incubated at 37°C for 15 min. Post-wash count and motility were checked.
Magnetic Activated Cell Sorting (MACS)
Kit contents were taken to room temperature before use. Assessed the sperm concentration and motility. Use a minimum of 105 to max 108 total spermatozoa for MACS separation. Perform density gradient separation (DGC). After DGC, wash the cells with 100 µl of MACS ART binding buffer. Remove all supernatant and add 100 µl of ART annexin reagent. Add 1× MACS ART binding buffer to a final volume of 500 µl. Mix well and incubate for 15 min at room temperature, 5 min before the 15-minute incubation and attach the MACS ART separation unit to the MACS multi-stand. Place the MACS ART MS column in the MACS ART separation unit. Place a tube below the MACS ART MS column to collect the rinsing buffer. Rinse the column with 1000 µl of 1× MACS ART binding buffer. Discard effluent and place a new collection tube for the target cell fraction under the MACS column. Apply cell suspension to the column and collect the flow-through fraction (Annexin V negative fraction). Wash the column with 500 µl of 1× MACS ART binding buffer. Collect the flow-through fraction in the same tube. The combined fraction represents enriched viable sperm. Mix the cell suspension in an equal volume of sperm wash media and centrifuge at 300× rpm for 5 min, aspirating the supernatant completely. Resuspend cells in sperm washing media or culture media for further application. Both MACS and DGC sperm preparation were done using standard hospital protocol.
Under general anaesthesia, oocytes were extracted using transvaginal ultrasonography to obtain human cumulus cells 35 h after human chorionic gonadotropin (hCG) was administered. After the denudation process, ICSI was performed for both groups. Injected oocytes were checked after 17 h for Two Pro-nuclei (2PN) status. Day 3 embryo has been checked after 72 h for grading. Similarly, blastocyst formation on day 5 was checked. Culture media used is vitrolife single step in benchtop incubators.
All embryos were frozen using Cryotech Medium by vitrification. Culture media used is vitrolife. Embryo transfer (ET) is done after preparing the endometrium using oestradiol valerate. Endometrial thickness of 9–13 mm and triple-line morphology with more than zone II vascularity have been taken as the criteria for ET.
Twelve days after ET, a serum hCG assay was carried out, and clinical pregnancy was verified when an ultrasound examination revealed a gestational sac with a foetal heartbeat.
Primary outcomes measured: 2PN status, total number of embryos, Day-2/Day-3 Grade-1 embryos, day 5 blastocyst formation. Two Pro-nuclei (2PN) status was measured on Day-1. Clevage stage embryos were graded based on blastomere size, symmetry and fragmentation on Day-2/Day-3. Blastocysts were graded according to Gardner’s scoring on Day-5.
Secondary outcomes: The clinical positive pregnancy outcome was measured as a gestational sac in USG with cardiac activity.
Anembryonic with beta-hCG positive followed by no gestational sac in USG.
Live-birth rate (LBR) was measured as at least 1 live baby delivering after 20 weeks gestation.
Ethical consideration: Study done after getting written informed consent. Confidentiality of the patients was maintained including name, address, and hospital ID. This study was approved by the Hospital Review Board. No; ARMC/PMNA/2/2023.
RESULTS
Written informed consent was obtained from each participant, and the data were handled and analysed in an anonymous, private manner. The data entry was done using Microsoft Excel. The data were analysed using SPSS version 26, a statistical analysis software program. This matched case-control study was conducted at the ARMC Aegis Hospital in Perinthalmanna, Kerala, from October 2021 to September 2023. The study group comprised the cycles (n = 58) in which MACS selection was carried out following the density gradient centrifugation process, while the control group (n = 58) simply underwent density gradient centrifugation for sperm selection. Pairwise matching was done for cases and controls to remove the confounding factors. Confounding factors taken were the age of the patients, BMI, underlying medical conditions, duration of the marriage, previous pregnancy history, lifestyle factors, duration of infertility, and use of other medications.
The baseline characteristics of the study population are given in Table 1. For continuous variables like age, duration of the marriage, levels of AMH, SA morphology, number of embryos, and distinct 2PN, an unpaired T-test was used to calculate the difference in mean. The chi-square test and Fisher Exact test were performed to find differences between categorical variables like previous pregnancy, embryo grade, and clinical pregnancy. Here, p-value ≤0.05 was considered to be statistically significant. The effect of MACS (cases) versus the control group was calculated using the odds ratio. A multivariate logistic regression model was used for calculating the adjusted odds ratio with a 95% confidence interval for minimising the effect of possible confounders like age, duration of marriage, previous pregnancy, embryo grades, etc. [Table 2].
| Characteristics | Cases | Controls | p-value |
|---|---|---|---|
| Number, N> | 58 | 58 | |
| Age* | |||
| Females | 30.4 ± 4.5 | 30 ±4.4 | 0.57 |
| Males | 35.2±4.6 | 36.1 ± 4.7 | 0.31 |
| Duration of marriage in years* | 6.6 ± 3.6 | 6.41±3 | 0.99 |
| Infertility status** | |||
| Primary infertility | 34 (58.6) | 36 (62.1) | 0.85 |
| Secondary infertility | 24 (41.4) | 22 (37.9) | |
| Levels of AMH in ng/ml* | 3.76 ± 2.24 | 3.83± 2.1 | 0.82 |
| SA morphology * | |||
| 1% | 23 | 27 | |
| 2% | 23 | 23 | 0.80 |
| 3% | 11 | 7 | |
| 4% | 1 | 1 | |
| 2PN* | 4.74 ± 2.9 | 3.84 ± 2.4 | 0.07 |
| Cleavage embryo grades** | |||
| Grade 1 | 46(79.3) | 24(41.4) | 0.0001 |
| Grade 2 | 8(13.8) | 21(36.2) | |
| Grade 3 | 4(6.9) | 13(22.4) | |
| No of embryos* | 2.90 ± 1.47 | 2.40 ± 1.88 | 0.11 |
| Day 5 blastocyst | |||
| Present | 20 | 15 | 0.58 |
| Absent | 38 | 43 | |
| Clinical pregnancies** | |||
| Positive | 22 (37.9) | 14 (24.1) | 0.1 |
| Negative | 36 (62.1) | 44 (75.9) | |
| Pregnancy outcome** | |||
| Live birth | 20 (90.1) | 12 (85.8) | 0.06 |
| Miscarriage | 2 (9.9) | 2 (14.2) |
| Variables | Cases | Control | Unadjusted odds ratio | Confidence interval | Adjusted odds ratio | Confidence interval | ||
|---|---|---|---|---|---|---|---|---|
| Lower limit | Upper limit | Lower limit | Upper limit | |||||
| Presence of 2 Pronucleate Embryo | ||||||||
| Yes | 57 | 55 | 3.10 | 0.03 | 3.18 | 0.13 | 0.01 | 1.69 |
| No | 1 | 3 | 1 | 1 | ||||
| Favourable embryo grades | ||||||||
| Yes | 46 | 24 | 5.43 | 2.38 | 13.36 | 8.14 | 2.97 | 22.32 |
| No | 12 | 34 | 1 | 1 | ||||
| Blastocyst formation on day 5 | ||||||||
| Present | 20 | 15 | 1.50 | 0.67 | 3.35 | 1.17 | 0.46 | 2.97 |
| Absent | 38 | 43 | 1 | 1 | ||||
| Clinical pregnancy | ||||||||
| Clinically confirmed | 22 | 14 | 1.92 | 0.86 | 4.28 | 2.14 | 0.69 | 6.67 |
| Failed conception | 36 | 44 | 1 | 1 | ||||
| Pregnancy outcome | ||||||||
| Miscarriage | 2 | 2 | 0.6 | 0.07 | 4.8 | 0.50 | 0.06 | 4.11 |
| Live births | 20 | 12 | 1 | |||||
MACS = Magnetic Activated Cell Sorting
Table 1 shows baseline characteristics of the study population, including age of male and female partners, duration of marriage, type of infertility, level of AMH, and semen analysis morphology. Also, the outcome of MACS (study group) versus DGC (control group) 2 PN (2PN status) stage, number of embryos, embryo grade, day 5 blastocyst formation, clinical pregnancies, and pregnancy outcome were studied.
The mean age of male partners in the case and control groups was 35.2 ± 4.6 years (case) & 36.1 ± 4.7 years (control), similarly female ages in both groups were 30.4 ± 4.5 years (case) and 30 ± 4.4 years (control). The duration of marriage in the case group was 6.6 ± 3.6 years, and in the control group was 6.41 ± 3 years. Likewise, primary infertility in the case group was 34 (58.6%), and in the control group was 36 (62.1%), secondary infertility was 24 (41.4%) in cases and 22 (37.9%) in the control group.
AMH in the case group was 3.76 ± 2.24, and in the control group, 3.83 ± 2.1. Semen analysis morphology in the case group with 1% good morphology was 23, 2% good morphology was 23, similarly 3% in 11, and 4% in 1. In the control group, 27 with 1% good morphology, 23 with 2% morphology, 7 with 3%, and 1 with 4 % good morphology.
All these baseline characteristics were analysed, p-value is insignificant in all these groups. It showed analysis was done in similar groups.
Outcome variables analysis showed a 2 PN mean in the MACS group (study group) as 4.74 ± 2.9 and in the DGC group (control group) as 3.84 ± 2.4. And obtained a very low p-value which is 0.07, even though it is statistically insignificant.
The fertilisation rate of MACS showed 48.75% from 564 mature oocytes. In the DGC group, a fertilisation rate of 40.32% was demonstrated out of 553 mature oocytes. Though higher, the MACS value was not statistically significant (p = 0.23).
In the cleavage embryo grades analysis, grade I embryos in the MACS groups were 46 (79.3%), grade II embryos were 8 (13.8%), and grade III embryos were 4 (6.9%). Similarly, in DGC groups, grade I embryos were 24 (41.4%), grade II embryos were 21 (36.2%), and grade III embryos were 13 (22.4%). Statistical analysis showed a p-value of 0.0001, which is statistically significant.
The mean number of embryos obtained in the MACS group was 2.90 ± 1.47, and in the DGC, group was 2.40 ± 1.88; here p-value showed 0.11, which is statistically insignificant.
Day 5 blastocyst formation in the MACS group was 20, and in the DGC group, it was 15. Even though more number of embryos were obtained in MACS, it was statistically insignificant. The p-value is 0.58.
Positive pregnancy obtained on MACS were 22 (37.9%), DGC 14 (24.1%). Here, the p-value was 0.1, which was insignificant.
Pregnancy outcome measured in MACS group as live birth 20 (90.1%), compared to DGC group 12 (85.8%). Miscarriage in MACS were 2 (9.9%), and in DGC were 2 (14.2%). P-value came very low 0.06, but not statistically significant.
Table 2 shows the outcome of MACS versus DGC by comparing the presence of 2PN status, favourable embryo grades, day 5 blastocyst formation, clinical pregnancy, and pregnancy outcome in both groups. The odds ratio and confidence intervals of both groups were analysed. The adjusted odds ratio was also analysed, considering the confounding factors.
2PN status in the MACS group was 57, and in the DGC group, it was 55. The adjusted odds ratio was 0.13 with a confidence interval of 0.01–1.69, which was statistically not significant.
Favourable embryo grades showed a value of 46 in MACS and 24 in the DGC group, with an unadjusted odds ratio of 5.43 with a confidence interval of 2.38–13.36, which was statistically significant. The adjusted odds ratio was 8.14 with a confidence interval of 2.97–22.32, which was again statistically significant.
Day 5 blastocyst formation in the MACS group was 20, whereas in the DGC group was 15, with an adjusted odds ratio of 1.17 (confidence interval 0.46–2.97), statistically not significant.
Positive PRs observed and clinically confirmed in MACS was 22, and in DGC was 14, with an adjusted odds ratio was 2.14 (confidence interval 0.69–6.67), statistically not significant.
The pregnancy outcome showing live birth in the MACS group was 20, and in DGC was 12. Unadjusted odds ratio 0.6 with a confidence interval of 0.07–4.8. Adjusted odds ratio 0.50 and confidence interval 0.06–4.11. Both were statistically insignificant.
DISCUSSION
In our study, baseline characteristics were compared and were noted to be statistically similar (at p = 0.05) when comparing the age of both partners, AMH, duration of marriage, infertility status, and semen analysis before processing.
Grade I embryos in the MACS groups were 46 (79.3%), grade II embryos were 8 (13.8%), and grade III embryos were 4 (6.9%). Similarly, in DGC groups, grade I embryos were 24 (41.4%), grade II embryos were 21 (36.2%), and grade III embryos were 13 (22.4%). Here, the p-value came as 0.0001, which is statistically significant. However, fertilisation rates, average embryos obtained, and blastocyst formation did not show a significant difference between the groups despite the higher numerical value in the MACS group.
Nadalini et al.[29] in their research noted that integrating MACS as a part of the sperm preparation technique does not improve sperm fertilising potential to the same extent as the traditional swim-up separation procedure.
The impact of MACS on rates of clinical pregnancy, miscarriage, embryo growth, and fertilisation in couples undergoing ICSI was assessed by Horta et al.[23] They found that there was no difference in the effect of MACS on patients with male factor infertility compared to those who were normozoospermic.
According to a study by Pacheco et al.[30], the study group experienced higher rates of pregnancy and good-quality blastocyst development and fragmentation after ICSI cycles on patients with normal sperm DNA fragmentation and those carried out using non-apoptotic MACS-selected spermatozoa. Another study by Dirican et al.[31] found a significant increase in chemical pregnancy when the study group used non-apoptotic MACS-selected spermatozoa to evaluate the impact of male infertility during ICSI treatments.
In contrast, our study showed no significant difference in PRs, miscarriage rates, ongoing pregnancies, or live births between the MACS group and the DGC group.
In Nilofer Zimati et al.’s study,[21] fertilisation, embryo quality, pregnancy, and implantation rates were evaluated between two groups using MACS and DGC against DGC alone. While there was no discernible variation in the rates of fertilisation between the two groups, the MACS DGC group exhibited considerably greater rates of pregnancy, implantation, and high-quality embryo percentage when compared to DGC alone. As a result, MACS might aid in the selection of the most viable sperm and enhance the clinical results of ICSI acquired for both groups.
In a different study, Romany et al.[22] assessed the effect of removing suspected dead sperm cells from specimens from unselected males using MACS on live-birth delivery rates after ICSI in couples undergoing ovum donation and demonstrated no improvement in pregnancy outcomes by using MACS over DGC.
Our study showed that the MACS group had better odds at attaining good quality cleavage stage embryos and blastocysts, better PRs, and lower odds of miscarriages when compared to the couples DGC group. Though the statistical significance was not satisfactory, we cannot overlook any advantage that an add-on procedure can contribute to total ART reproductive outcomes.
LIMITATIONS
The major drawback of the study was that it was analysed retrospectively. A prospective study would have made it possible to create tighter inclusion and exclusion criteria.
Randomisation of initial subjects was not possible, as the procedure was done at the discretion of the participating couples.
CONCLUSION
Recently, many methods for selecting sperm have been discovered that can initiate the processes involved in sperm-cell capacitation. One such is the MACS technique. This study showed an increase in the fertilisation rates, number of embryos, grade I embryos, and day 5 blastocyst formation in the MACS group compared to the conventional DGC method. However, embryo grades (grade I embryos) in the MACS group were high compared to the DGC group (p-value <0.01).
Hence, the application of MACS as part of advanced sperm selection in male partners with teratozoospermia led to improved cleavage rates and a marginal increase in fertilisation rates.
For couples with severe male factors and aberrant sperm morphology, MACS, in addition to traditional sperm processing, may be provided as an option.
Ethical approval
This study was approved by the Hospital Review Board. Approval number: ARMC/PMNA/2/2023.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
REFERENCES
- Role of semen analysis in subfertile couples. Fertil Steril. 2011;95:1013-9.
- [CrossRef] [PubMed] [Google Scholar]
- Sperm DNA fragmentation index as a promising predictive tool for male infertility diagnosis and treatment management - meta-analyses. Reprod Biomed Online. 2018;37:315-26.
- [CrossRef] [PubMed] [Google Scholar]
- Sperm DNA fragmentation: Paternal effect on early post-implantation embryo development in ART. Hum Reprod. 2006;21:2876-81.
- [CrossRef] [PubMed] [Google Scholar]
- Late, but not early, paternal effect on human embryo development is related to sperm DNA fragmentation. Hum Reprod. 2004;19:611-15.
- [CrossRef] [PubMed] [Google Scholar]
- Paternal influence of sperm DNA integrity on early embryonic development. Hum Reprod. 2014;29:2402-12.
- [CrossRef] [PubMed] [Google Scholar]
- Developmental sperm contributions: Fertilization and beyond. Fertil Steril. 2009;92:835-48.
- [CrossRef] [PubMed] [Google Scholar]
- Measuring sperm DNA fragmentation and clinical outcomes of medically assisted reproduction: A systematic review and meta-analysis. PLoS One. 2016;11:e0165125.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The source and significance of DNA damage in human spermatozoa; a commentary on diagnostic strategies and straw man fallacies. Mol Hum Reprod. 2013;19:475-85.
- [CrossRef] [PubMed] [Google Scholar]
- Double-stranded DNA breaks hidden in the neutral comet assay suggest a role of the sperm nuclear matrix in DNA integrity maintenance. Mol Hum Reprod. 2014;20:330-40.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Apoptosis, spermatogenesis and male infertility. Front Biosci (Elite Ed). 2012;4:746-54.
- [CrossRef] [PubMed] [Google Scholar]
- The impact of single- and double-strand DNA breaks in human spermatozoa on assisted reproduction. Int J Mol Sci. 2020;21:3882.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Abnormal spermatozoa in the ejaculate: Abortive apoptosis and faulty nuclear remodelling during spermatogenesis. Reprod Biomed Online. 2003;7:428-32.
- [CrossRef] [PubMed] [Google Scholar]
- Mononuclear phagocytes rapidly clear apoptotic epithelial cells in the proximal epididymis. Andrology. 2014;2:755-62.
- [PubMed] [Google Scholar]
- Sperm selection in natural conception: What can we learn from mother nature to improve assisted reproduction outcomes? Hum Reprod. 2015;21:711-26.
- [CrossRef] [Google Scholar]
- Does combining magnetic-activated cell sorting with density gradient or swim-up improve sperm selection? J Assist Reprod Genet. 2016;33:1059-65.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Sperm selection for ICSI using annexin V. Methods Mol Biol. 2013;927:927.
- [CrossRef] [Google Scholar]
- New era in sperm selection for ICSI. Int J Androl. 2012;35:475-84.
- [CrossRef] [PubMed] [Google Scholar]
- Magnetic-activated cell sorting for sperm preparation reduces spermatozoa with apoptotic markers and improves the acrosome reaction in couples with unexplained infertility. Hum Reprod. 2010;25:839-46.
- [CrossRef] [PubMed] [Google Scholar]
- Efficient isolation of sperm with high DNA integrity and stable chromatin packaging by a combination of density-gradient centrifugation and magnetic-activated cell sorting. Clin Exp Reprod Med. 2016;43:199-206.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Clinical outcome using non-apoptotic sperm selection for ICSI procedures: Report of 1 year experience. Fertil Steril. 2010;94:S232.
- [Google Scholar]
- Clinical outcomes of magnetic activated sperm sorting in infertile men candidate for ICSI. Hum Fertil (Camb). 2019;22:118-25.
- [CrossRef] [PubMed] [Google Scholar]
- Removal of annexin V–positive sperm cells for intracytoplasmic sperm injection in ovum donation cycles does not improve reproductive outcome: A controlled and randomized trial in unselected males. Fertil Steril. 2014;102:1567-75.
- [CrossRef] [PubMed] [Google Scholar]
- Male factor infertility outcomes using magnetic activated cell sorting in intra cytoplasmic sperm injection cycles. Andrology. 2016;5:155-9.
- [Google Scholar]
- Sperm DNA fragmentation index, as measured by sperm chromatin dispersion, might not predict assisted reproductive outcome. Taiwan J Obstet Gynecol. 2018;57:493-98.
- [CrossRef] [PubMed] [Google Scholar]
- Aneuploidy in spermatozoa of infertile men with teratozoospermia. Int J Androl. 2001;24:197-205.
- [CrossRef] [PubMed] [Google Scholar]
- Sperm chromatin structure assay parameters are not related to fertilization rates, embryo quality, and pregnancy rates in in vitro fertilization and intracytoplasmic sperm injection, but might be related to spontaneous abortion rates. Fertil Steril. 2008;90:352-9.
- [CrossRef] [PubMed] [Google Scholar]
- Random sperm DNA fragmentation index is not associated with clinical outcomes in day-3 frozen embryo transfer. Asian J Androl. 2022;24:109-115.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Utility of magnetic activated cell sorting (MACS) in assisted reproduction. AIMJ. 2022;3:22-9.
- [CrossRef] [Google Scholar]
- Annexin V magnetic-activated cell sorting versus swim-up for the selection of human sperm in ART: Is the new approach better than the traditional one? J Assist Reprod Genet. 2014;31:1045-51.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Magnetic-activated cell sorting (MACS): A useful sperm-selection technique in cases of high levels of sperm DNA fragmentation. J Clin Med. 2020;9:3976.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Clinical outcome of magnetic activated cell sorting of non-apoptotic spermatozoa before density gradient centrifugation for assisted reproduction. J Assist Reprod Genet. 2008;25:375-81.
- [CrossRef] [PubMed] [Google Scholar]







