Translate this page into:
Abstract Fertivision 2016
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
1. Oxidative stress and low-grade inflammation in patients of polycystic ovary syndrome
Objective:
The aim of this study was to evaluate the role of oxidative stress and low-grade inflammation in polycystic ovary syndrome (PCOS) patients with normal and obese condition and correlate these factors with insulin resistance and hyperandrogen, which are aetiopathological factors of pathogenesis of PCOS.
Methods:
Thirty clinically diagnosed PCOS patients according to Rotterdam criteria and thirty apparently healthier subjects who were registered in outpatient's clinic of Sir Sundar Lal hospital, BHU have been included in this study. Assessment of markers of oxidative stress, low-grade inflammation, hyperandrogenism and insulin resistance were performed in both PCOS patients and control groups.
Results:
There were significant increase in markers of low-grade inflammation and oxidative stress in PCOS patients as compared to their control groups. Insulin resistance and testosterone were significantly high in PCOS patients. The difference between control groups and PCOS patients group is significant to (P < 0.001).
Conclusion:
This study suggests that low-grade inflammation and oxidative stress are independent of obesity, which along with insulin resistance and androgens is incriminating causative factors of PCOS. Testosterone is primarily responsible for induction of low-grade inflammation and oxidative stress and higher BMI is additive in this process.
2. In menstruating women endometrial preparation by hormone replacement and Natural/Stimulated cycle have comparable success rates for frozen embryo transfer
Objectives:
To compare the Frozen Embryo Transfer (FET) outcome in natural/stimulated (Nat/Stim) and hormone replacement cycles (HRT).
Methods:
Duration: Jan 2014 – June 2016. Inclusion: Out of 503 FET cycles, 216 menstruating women, 23-40 years of age were included.
Exclusion: Postmenopausal women, blastocyst transfer, dual transfer, ovum donation cycles, thin endometrium (<7 mm) and poor quality embryos. Group 1 (n = 119) – Nat/stim cycles - Ovulation was documented in nat/stim cycles by serial ultrasonography. Injection hCG 5000 IU I/M was given when lead follicle was >18 mm size. Group 2 (n = 97) – HRT cycles - Estradiol valerate (E2Val) 6 mg/day, given orally in divided doses and transdermal estrogel 7.5 mg/d administered from day 1 or 2 of periods. Endometrial thickness was assessed sonographically and injectable progesterone (P) 100 mg I/M was started when endometrium >7 mm was achieved. Thawing of embryos was done on day 4 post HCG injection and day 2 of Pstart in group 1 and 2 respectively and transfer was done after 24 hours of culture after ensuring growth and quality of embryos. In Luteal phase, P 100 mg I/M in both groups and in group 2, E2Val and E2 gel were also continued until β-hCG test (day 14 post embryo transfer) and through first trimester of pregnancy.
Results:
The β-hCG positive rate, Clinical pregnancy rate and Implantation rate were (37.82%, 29.90%), (28.57%, 28.87%) and (12.04%, 10.82%) in Nat/Stim and HRT cycles respectively but the difference was not statistically significant.
Conclusion:
There was no significant difference in FET outcome between Nat/stim cycles as compared to HRT.
Theme: Clinical.
3. Correlation of ovarian reserve parameters with the outcome of in vitro fertilization/intracytoplasmic sperm injection cycles in gonadotrophin releasing hormone antagonist protocol
Objective:
To correlate serum AMH and AFC with the number and quality of oocytes, embryos and clinical pregnancy.
Methods:
In this cross sectional study, total 49 women aged between 21 to 42 years who were stimulated with GnRh antagonist protocol for IVF/ICSI during May to September 2016 were included. Serum AMH and AFC were obtained on day 2 of the cycle. Number of oocytes and embryos retrieved were noted and grading of quality of oocytes and embryos was done using Thomas Ebnar and James Catt et al. criteria. Positive cardiac activity on TVS was taken as clinical pregnancy. Statistical analysis was done using SPSS version 22.0.
Results:
Out of the total 49 patients 25 were positive for pregnancy (51%) and cardiac activity was seen in 21 patients (42.9%). Serum AMH and AFC was significantly correlated with the number of oocytes obtained (p = 0.00, P= 0.00). A positive correlation of serum AMH and AFC was seen with quality of oocytes and quality of embryos, but it was not found to be significant. Correlation of AMH, AFC with the clinical pregnancy was found to be not significant. However significant correlation was seen between clinical pregnancy and grade 1 quality of embryos (p = 0.19) with an overall accuracy of 63%. Blastocyst formation was seen in 100% of the Grade 1 embryos.
Conclusion:
The present study concludes that serum AMH and AFC are biomarkers of number of oocytes obtained after stimulation. The quality of embryo is an independent and most important determinant for clinical pregnancy in patients undergoing IVF/ICSI in antagonist cycles.
Theme: Clinical.
4. Role of inflammatory cytokine, interleukin 6 in endometriosis and its correlation with the stage of disease
Objective:
To find out the co-relation of inflammatory marker cytokine IL-6 and stage of ndometriosis.
Methods:
A prospective study, from July 2013 - July 2015 at Institute of Medical Science, Department of obstetrics and gynecology, Department of Immunopathology, Banaras Hindu University. 50 cases with chronic pelvic pain and infertility, per operatively diagnosed endometriosis and 50 controls who were fertile of comparable age, eumenorrhic, planned for tubal ligation were taken. They were investigated for routine, infertility work up followed by lapro-hysteroscopy or laparotomy. Peripheral blood sample was taken for estimation of serum IL-6 by Immunoenzymetric assay (ELISA).
Result:
Mean IL-6 levels were very much elevated in all types as compared to controls. Level increases with severity of endometriosis and even adenomyosis. Severe type endometriosis had highest mean IL-6 level, it was 535.99 (140.70-1704.0) as compared to controls which was 4.43 (2.83-6.11).
Conclusion:
IL-6, an inflammatory cytokine was increased in ascending order with stage of the disease. Endometriosis progresses with increase in inflammation. So it can be prevented by reducing the inflammation. An early diagnosis of Endometriosis and initiation of its treatment can improve the gynecological future of patient and can also prevent progression, symptom worsening and development of related infertility.
Theme: Miscellaneous
5. Correlation of applebaum scoring in predicting pregnancy outcome in infertility patients
Objective:
We aimed to evaluate the correlation of Applebaum Scoring in predicting pregnancy outcome in spontaneous cycle in patients with unexplained infertility.
Method:
A prospective observational study was conducted in the Department of Obstetrics and Gynecology, UP Rural Institute of Medical Sciences and Research, Saifai on 55 women with unexplained primary infertility after standard diagnostic work up. Ultrasound (TVS) measurement of all patients was performed in their midcycle of spontaneous cycle.
Outcome Measures:
The Uterine Biophysical Profile (UBP) were noted during the normal midcycle of these patients which included 7 parameters: Endometrial thickness in greatest AP dimension (full-thickness measurement), a layered (“5 line”) appearance to the endometrium, myometrial contractions, myometrial echogenecity, uterine artery blood flow as measured by PI, blood flow within the zone 3 using colour Doppler, myometrial blood flow seen on gray-scale examination. Applebaum Scoring i.e. the “Uterine Scoring System for Reproduction” (USSR) was used to evaluate the total score.
Results:
Among 55 unexplained primary infertility cases, 24 (43.63%) conceived during serial ultrasonographic monitoring of spontaneous menstrual cycle and timed intercourse. According to Applebaum scoring, with a ‘perfect score’ of 20, there was 80% conception rate. While 9/15 patients (60%) conceived with a score 17-19. With a score of 14 16, 10/23 (43.37%) patients conceived. Only 8.33% conception rate was seen with a low score of 13 or less. Highest pregnancy rate (60%) was seen with an endometrial thickness of 7-9 mm while zone IV (as per applebaum criteria) endometrial blood flow gave maximum conception rate of 66.66%.
Conclusion:
Applebaum scoring using UBP can prove to be simple, rapid and non invasive tool to predict uterine environment and hence pregnancy outcome.
Theme: Clinical
6. Impact of midluteal serum progesterone levels on pregnancy outcome in fresh and frozen embryo transfer cycles
Objective:
To assess whether mid-luteal serum progesterone impacts pregnancy outcome in fresh and frozen embryo transfer cycles.
Methodology:
Patients undergoing embryo transfer at our ART center were enrolled after obtaining written and informed consent. Patients with age more than 40 years, Hyperresponders, Recurrent Implantation Failures, poor embryo quality and patients where standard LPS not followed were excluded. Dose in antagonist cycle was based on Age, BMI, ovarian reserve and previous response. Antagonist started according to flexible protocol. Human chorionic gonadotropin was given as trigger. LPS in fresh cycles given using vaginal micronized progesterone 400 mg twice a day and Inj micronized progesterone 50 mg twice a week. In frozen cycles LPS was vaginal micronized progesterone 400 mg twice a day and Inj micronized progesterone 50 mg alternate day. Progesterone levels analysed on day 3 after a blastocyst transfer and day 5 after a day 3 transfer.
Results:
In fresh cycles out of 66 women recruited in the study 11 patients had Progesterone <15 ng/ml. Of these only 1 (9%) became pregnant. Of the 55 patients having progesterone >15 g/ml 22 patients (40%) became pregnant. Pval (0.049). In frozen cycles out of 79 women recruited 21 had progesterone less than 15 of which 10 (47%) became pregnant. Of 58 patients with progesterone >15 ng/ml 30 (51.7%) cases became pregnant (P = 0.34).
Conclusion:
As per the above study in fresh cycle midluteal progesterone level less than 15 ng/ml has significant negative clinical and statistical impact on the pregnancy. Evaluation of midluteal progesterone in fresh IVF cycles may help to identify patients who need additional LPS to improve pregnancy outcome. No correlation was observed in patients undergoing FET.
7. Association of insulin resistance with serum Vitamin D status in Indian subjects with polycystic ovarian syndrome
Objective:
Polycystic Ovarian Syndrome (PCOS) is the most common endocrine disorder affecting 5-10% of in women during the reproductive age group. Its prevalence among infertile women is 15%–20%. It has an X-linked mode of inheritance but the precise etiology is unclear. PCOS has a long prodrome with detectable abnormalities presenting as Metabolic Syndrome X. The clinical manifestations of PCOS vary from a mild menstrual disorder to severe disturbance of the reproductive and metabolic functions. Emerging evidence suggests a possible influence of vitamin D on reproductive function in females. Present study aims to evaluate the association of Insulin Resistance with Serum Vit D status in subjects with Polycystic Ovarian Syndrome.
Methods:
This cross-sectional study was conducted from May 2016 till date in the Gynae OPD at AIIMS, Rishikesh. It included 96 women with PCOS diagnosed by Rotterdam's criteria. Waist-to-hip ratio (WHR), Ferriman-Gallwey score, Vit D levels, OGTT with 75 gms glucose, homeostasis model assessment of insulin resistance (HOMA-IR), Lipid profile, LH/FSH, total testosterone, and DHEAS were measured.
Results:
Results were expressed as mean ± SD and were statistically analysed using SPSS software version 16, unpaired student's t-test and Pearson's correlation coefficient. We found lower levels of Vitamin D, which was statistically significant. Hyperinsulinemia, rise in insulin resistance and low HDL levels was observed in the present study. The correlation of Vitamin D with insulin resistance and Homeostatic Model of Assessment- Insulin Resistance Index (HOMA-IR) was weak and did not show any statistical significance.
Conclusions:
Hypovitaminosis D results from the presence of obesity and insulin resistance in women with PCOS. This is perhaps related to metabolic and hormonal disorders in PCOS. However, randomized control trials are required to explore the above hypothesis.
Theme: Clinical
8. In vitro fertilization outcome in menopausal age group and in cases of premature ovarian failure: An observational study
Objective:
To study the outcome of IVF in menopausal age group and cases of premature ovarian failure.
Methods:
The study was conducted at Creator's IVF Nepal Pvt. Ltd. in 181 ladies who belonged to the categories of menopausal age group and premature ovarian failure cases. This is a retrospective observational study carried out using the records in the centre.
Results:
The infertility centre has already provided IVF service to a total of 686 infertile patients among which 153 (22.3%) were of menopausal age group (≥40 years). Among the 153 patients, 63 (41.17%) had positive pregnancy. Likewise, there were 28 cases (4.01%) of premature ovarian failure among which 11 (39.28%) had positive pregnancy.
Conclusion:
The scenario observed at our centre gives a positive outlook to the treatment option for menopausal women and those suffering from premature ovarian failure.
Theme: Clinical.
9. Increasing body mass index does not have an impact on in vitro fertilization embryo transfer outcome in normal responders: A retrospective analysis
Objective:
To study the impact of increasing BMI on IVF outcome in normal responders.
Materials and Methods:
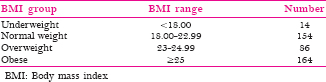
The study was conducted from January 2012 to September 2015. Subjects included women aged <35 years, undergoing first IVF cycle where number of oocytes retrieved ranged between 6-14 and embryo transfer was done. Out of 1564 patients, 418 fulfilled the inclusion criteria. BMI cut offs as per Asian Indian standards:
Outcome parameters studied were gonadotropin dose, metaphase 2 (M2) number, M2 rate, fertilization rate, cleavage rate, embryo quality and number of embryos frozen. End points for IVF outcome studied were clinical pregnancy rate, implantation rate and live birth rate. Statistical analysis was done using SPSS version 18 with one way ANOVA for multiple comparisons and Pearson's co relation for establishing correlation of various variables with BMI.
Results:
There was statistically significant positive correlation between BMI and gonadotropin requirement (P < 0.031). In sub group analysis of obese group, number of M2 oocytes retrieved was significantly lower (P < 0.018) in subjects with BMI >=30. However, this did not have any impact on M2 rate, fertilization rate, cleavage rate, embryo quality and number of embryos frozen in different BMI categories. The IVF outcome in terms of clinical pregnancy rate, implantation rate or live birth rate was similar in all BMI groups (P > 0.8).
Conclusion:
Increasing BMI has no impact on IVF outcome in normal responders. However gonadotropin requirement increased with increasing BMI.
Theme: Clinical.
10. Can number of retrieved oocytes predict reproductive outcome in fresh assisted reproductive technology cycles?
Objective:
This prospective observational study aimed to evaluate relationship between number of oocyte retrieved and reproductive outcome in women aged 23-40 years undergoing fresh ART cycle.
Method:
A trial of 109 patients in age group 23-40 years who received ovarian stimulation by GnRH antagonist protocol in Akanksha IVF centre from March 2016 to September 2016 were categorized in 5 groups. Categorisation was based on number of retrieved oocytes namely 5-7, 8-10, 11-13, 14-16, 17-19 and designated as group I, II, III, IV, V respectively. Only cycles with single fresh blastocyst transfer were included in the study. Primary outcomes-implantation rate, clinical pregnancy rate and ongoing pregnancy rate per embryo transfer were computed and compared among groups. Secondary outcomes were fertilisation rate, cleavage rate and pregnancy rate. Qualitative variables were summarized as frequencies/percentages and analysed using Chi-square test and quantitative variables as mean ± sd and compared using ANOVA.
Results:
Fertilisation rate (77%), Implantation Rate (59.3%), pregnancy rate (59.3%), clinical pregnancy rate (55.6%), ongoing pregnancy rate (44.4%) were found to be highest in group III where oocyte retrieved were 11-13 oocytes but it did not reach statistical significance comparing other groups.
Conclusions:
This study shows that number of oocytes harvested is a prognostic marker of reproductive outcomes in fresh ART cycles being maximal when eleven to thirteen oocytes were retrieved, declining on either side. However studies with larger sample size are required in this regard.
11a. Can response to clomiphene be predicted by the patient's clinical/metabolic/bio-chemical profile: A comparitive study between clomiphene citrate sensitive and resistant patients
Objective:
To compare the clinical/metabolic/bio-chemical parameters in the patients on clomiphene with polycystic ovarian syndrome (PCOS) related infertility and to further co-relate this with their response to clomiphene.
Methods:
A prospective observational study was conducted at PGIMER, Chandigarh on PCOS females of age group 20-35 years in the year 2016. Basal levels of various potential predictors (clincal/metabolic/hormonal) of ovulation were recorded before initiation of ovulation induction with clomiphene citrate. Response to clomiphene citrate was correlated with these potential predictors of ovulation.
Results:
Total of 50 patients recruited. Following treatment with increasing dose of clomiphene citrate, 24 of these patients ovulated (48%). Significant differances between CC resistant and CC sensitive groups were noted in severity of oligomenorrhea, weight, BMI, blood pressure, fasting insulin levels, lipid profile and LH levels. OGTT was more deranged in CC resistant group but the difference was statistically significant only in the 1 hour post meals value. Waist circumferance, Ferriman gallway score, LH/FSH, 17 OHP, androstendione levels and HOMA-IR values was higher in CC resistant group but the difference was not statistically significant.
Conclusion:
Severity of oligomenorrhea, weight, BMI, blood pressure, fasting insulin levels, lipid profile and LH levels can be used to predict response to clomiphene citrate in femlaes with PCOS.
Theme: Clinical.
11b. A case of pan-hypopituitarism with successful pregnancy through in vitro fertilisation-embryo transfer
Objective:
This case is being presented for its rarity, prompt diagnosis and successful management with an aim to discuss the stimulation protocols, adjuvant therapies and hormone deficiencies with their adequate, well-timed substitution before embarking onto IVF-ET in hypopituitarism patient.
Methods:
A 36 year old female, NRI, married since 2 years known case of hypopituitarism presented with primary infertility. At the age of 26 years, patient presented with oligo menorrhea and subsequently developed amenorrhoea. Thereafter, multiple HRT cycles were given. Patient was on long term thyroid and steroid supplementation. Basal scan showed normal AFC. Hormonal profile was done and COH was given along with substitution of other deficient hormones. rFSH, rLH, HMG with GnRH antagonist protocol was used. Daily TVS folliculometry and hormonal estimation as and when required was done. OPU was done after 15 days of prolonged stimulation and 2 blastocyst transfer was done subsequently. Complete luteal support was given and hormones were monitored.
Results:
Patient conceived with triplet pregnancy. Embryo reduction was done for one fetus and is at present uncomplicated 18 weeks twin gestation. Her TIFFA and triple test is normal.
Conclusions:
Conception and uncomplicated pregnancies in panhypopitutarism patients is rare but not impossible. Hormone deficiencies should be managed carefully and restored to normal levels. Stimulation with HMG – HCG and addition of growth hormone improves follicular maturation.
Theme: Clinical.
12. Efficacy of oxytocin receptor antagonist in embryo transfer recipients
Objective:
(i) Primary: To evaluate the efficacy of Atosiban in improving the implantation rate (IR) and clinical pregnancy rate (CPR) after ET.
(ii) Secondary: To evaluate the safety of Atosiban in enrolled patients.
Methods:
With reference to previous studies, sample size of 100 patients in each group was determined. Statistical testing was conducted with the SPSS 17.0 software and Pvalue less than 0.05 indicated a significant difference. As per predefined inclusion and exclusion criteria, participants from August 2016 onwards were randomly allocated into test and control groups. The study medication ‘Atosiban’ used as 37.5 mg in 5 ml was given in bolus followed by infusion dose over approximately 3.5-4 hours at ET.
Results:
An interim analysis of 73 patients from each of the intervention and control groups showed higher pregnancy rate of 46.8% in the former group. The IR in the test and control groups are 57.5% and 46.6% respectively which was statistically significant (P < 0.46). Demographic parameters were comparable and no major adverse effects of drug observed so far. The miscarriage rates were also lower in treated group.
Conclusions:
Treatment with atosiban before ET increased the IR, CPR and decreased the miscarriage rate, which may be the result of increased endometrial perfusion and decreased uterine contractility thus enabling retention of embryos.
Theme: Embryology.
13. Evaluation of relationship of anti Mullerian hormone with ultrasound markers of ovarian reserve and body mass index in infertile women with polycystic ovarian syndrome and other infertile women
Objective:
To determine any difference in relationship of AMH with – antral follicle count (AFC), ovarian volume and BMI between infertile women with PCOS and infertile women with other etiology.
Material and Methods:
This descriptive cross sectional study included 382 infertile women attending the fertility clinic from April 2016 to October 2016. Study participants were divided into two groups – PCOS and control. Serum AMH, AFC, ovarian volume, and BMI were determined for all participants. The AMH/AFC ratio and AMH/ovarian volume ratio were calculated for each of them.
Results:
Of the 382 women studied, 92 were in PCOS group while 290 were in control group. Mean AMH/AFC ratio in PCOS group and control group was 1.82 and 1.01 respectively. It was significantly higher in PCOS group. There was no significant difference in the mean AMH/ovarian volume ratio of both groups. While no correlation between AMH and BMI was seen in control group (r = 0.04, P> 0.05), AMH was inversely correlated with BMI in PCOS group (r = 0.36, P< 0.005)
Conclusions:
Results suggest that infertile women with PCOS produce more AMH per antral follicle when compared to other infertile women. Also, AMH levels are inversely and strongly correlated with BMI in PCOS group, while no such correlation was seen in control group.
Theme: Clinical.
14. Correlation between endometrial thickness and pregnancy rate following intra cytoplasmic sperm injection
Objectives:
Study was performed to investigate the relationship between the endometrial thickness, embryo quality and pregnancy rate following ICSI.
Methods:
This retrospective study included 10412 patients, who underwent ICSI cycle from July 2015 to August 2016 in Indira IVF Hospital Pvt ltd. Endometrial thickness was measured on day of HCG in OPU and on day of inj. Gestone in frozen embryo transfer and ovum donation cases. Patients were divided into four groups according to endometrial thickness such as group 1 (<6 mm), group 2 (6 to 9.9 mm) group 3 (10 to 14 mm) and group 4 (>14 mm). In addition, patient's age, BMI and embryo quality were also calculated and correlated with pregnancy outcome.
Results:
The mean age of the patients ranges between 31.15 ± 0.5 years to34.36 ± 1.1 years in all groups. The BMI ranged from 23.1 ± 0.5 to 24.87 ± 0.14. The highest pregnancy rate was observed in group 4, which was around 65%. In contrast, Group 1 showed lowest pregnancy (54%). In addition, we have observed a direct correlation between the endometrial thickness and pregnancy outcome.
Conclusions:
Endometrial thickness is a statistically significant factor in pregnancy rates that may be clinically useful in decisions regarding number of embryos transferred to ensure a better pregnancy rate.
Theme: Clinical.
15. To study the influence of sperm DNA fragmentation on intrauterine insemination and intracytoplasmic sperm injection outcome
Objective:
To study the influence of sperm DNA fragmentation on Intrauterineinsemination (IUI) and Intracytoplasmic sperm injection (ICSI) outcome. (1) To evaluate the extent of sperm DNA fragmentation in patients undergoing (IUI) and Intracytoplasmic sperm injection (ICSI) cycle. (2) To study the effect of DNA fragmentation on IUI and ICSI outcome.
Method:
A prospective study is being conducted at Dr. Kuldeep Jain's IVF and Laparoscopy Centre. A minimum of 100 subjects will be included in the study. Inclusion criteria: All patients going for IUI or ICSI with ejaculated sperm irrespective of their factor.
Exclusion criteria: ART procedure involving cryopreserved sperm samples or testicular extracted sperm. Written informed consent is obtained from all patients undergoing IUI and ICSI cycles, who are enrolled in the study. Standard protocol as per requirement of individual case was used for optimal stimulation. Semen sample is collected by masturbation, after an abstinence of 3 days. DNA fragmentation test is done on the day of procedure (IUI/ICSI), using sperm chromatin detection (SCD) test using CANfrag kit (Manufacturer - B S SCIENTIFIC), before processing the sample for procedure. A DFI >30% is taken as significant. Rest of the procedure is carried out as per standard protocol. Primary outcome: (1) Post wash recovery, (2) fertilization, cleavage and embryo morphology in ICSI. Secondary outcome: (1) Pregnancy rate in IUI and ICSI, (2) appropriate statistical analysis will be done using standard tests.
Theme: Clinical ART.
16. Endometrial preparation for frozen thawed embryo transfer with exogenous gonadotropins in oligoovulatory women showing poor response to exogenous estrogen
Objectives:
Primary: To evaluate the role of exogenous gonadotropins in improving the endometrial thickness in oligoovulatory women with thin endometrium (<7 mm) on exogenous estrogen. Secondary: To compare the positive BHCG and clinical pregnancy rate in the above mentioned group and in women where FET was done on endometrial thickness (ET < 7 mm) after exogenous estrogen treatment (historical controls).
Design:
Retrospective observational study. Duration: January 2015 to July 2016. Inclusion: Females with oligovulatory cycle and ET <7 mm after estrogen exposure for up to 20 days in the form of tablets, transdermal gels and/or injectable and FET cancelled.
Exclusion: (1) Uterine abnormality on either hysteroscopy or 3D transvaginal ultrasound. (2) Poor quality embryos (less than grade 4). (3) Age of self/donor at the time of oocyte retrieval >/=38 years
Methodology:
Low dose Recombinant FSH or Human Menopausal Gonadotropin was started from D2/3 of cycle after doing baseline hormonal and ultrasound. Regular follow up with TVS ultrasound for follicular growth, endometrial thickness and pattern was done. HCG trigger was given once the dominant follicle reached >/=18 mm size with adequate endometrial thickness.
Results:
29 females were exposed to low dose gonadotropins for endometrial preparation. Endometrial thickness >/=7 was seen in 21 cases (72.41%). Average ET was 7.6 mm. Positive BHCG rate was 68.96% (20/29). Clinical pregnancy rate was 55.17% (16/29).
BHCG and clinical pregnancy rate was significantly higher (P value 0.007 and 0.044 respectively) in gonadotropin treated females compared to females on exogenous estrogen with endometrial thickness <7 mm (38% and 34.54%). BHCG and clinical pregnancy rate was higher in gonadotropin treated females compared to females on exogenous estrogen with endometrial thickness >/=7 mm (48% and 40%), the difference was not significant.
Conclusion:
Low dose gonadotropins can be used as an alternative for endometrial preparation in oligovulatory females not responding to exogenous estrogens.
Theme: Clinical.
17. Management of a rare case of post in vitro fertilization triplet ectopic pregnancy post bilateral tubal occlusion
Incidence of ectopic pregnancy after in vitro fertilization and embryo transfer in patients with prior bilateral tubal occlusion is negligible, yet it can occur at the isthmic stump, cornua/interstitial or angle of uterus. Because of the possibility of early uterine rupture with life threatening haemorrhage, treatment of such pregnancies often requires removal of uterus as a life saving measure. The difficulties in management of such ectopic pregnancies especially if one need to save the uterus is immense, more so in high order ectopic pregnancies. We hereby report a case of triplet live ectopic pregnancy with beta hCG more than 2 lac units (2 in right cornua/interstitial) and 1 in left isthmus of 6 weeks and 5 days) following embryo transfer of 3 day 5 blastocysts. This patient had undergone laparoscopic bilateral proximal tubal occlusion 5 years ago for bilateral hydrosalpingx with frozen pelvis. She also had history of 6 failed IVF cycles at different centers for tubal factor infertility before she presented to us with this ectopic pregnancy.
Management
Patient was taken up for surgery after all necessary pre-operative details were taken care off. It was difficult to ascertain by all diagnostic modalities used pre-operatively whether the 2 right sided ectopic pregnancies were in the angle of the uterus or within the cornua hence as the first step, trans abdominal ultrasound guided suction evacuation of these sacs was attempted unsuccessfully. Hysteroscopy followed, which confirmed normal endometrial cavity with no gestational sac within it hence the diagnosis of interstitial/cornual pregnancy was confirmed. Laparoscopy was attempted but converted to laparotomy due to frozen pelvis. Post adhesiolysis and bowel dissection, bulky uterus with left sided cornual bulge was seen suggestive of left isthimic pregnancy. Pitressin was injected, incision made, products evacuated and hemostatic sutures applied. On the right side post bowel dissection hydrosalpingx drained, pitressin injected at uterine angle and while de-roofing hydrosalpingx products of conception seen extruding from uterine musculature close to angular area. Products evacuated and hemostatic sutures applied and intra operative ultrasound used to confirm complete clearance of both sacs before closing the abdomen. Post-operative period was uneventful.
This case highlights the importance of using gambit of diagnostic and operative procedures in absolute synchrony to enable treatment of such cases successfully. This case report also highlights the misery and complications which could follow multiple embryos transfer especially if these are blastocysts which have a much higher probability of implantation.
18. Effect of chemical oocyte activation with calcium ionophore on intra-cytoplasmic sperm injection out-comes in women with previous fertilisation failure
Objective:
To study the effect of chemical oocyte activation with calcium ionophore on fertilisation and pregnancy outcomes in women undergoing ICSI with previous fertilisation failure.
Design:
Prospective case-control study from Jan 2014 to July 2016 at Akanksha IVF Centre, New Delhi.
Material and Methods:
Forty patients with history of previous fertilisation failure undergoing ICSI treatment were randomly divided into two groups: In group A (N = 15) oocytes were routinely injected with ICSI while in group B (N = 25) oocytes were cultured in medium supplemented with 5 mM calcium ionophore (A23187) for 10 minutes and then washed at least five times with MOPS solution immediately after ICSI. In both groups, the fertilisation was evaluated after 16-18 hours.
Results:
The number of fertilised oocytes and embryos obtained were significantly different between two groups (P < 0.001). Fertilisation rate was significantly higher in group B - where calcium ionophore was applied compared to group A-control group. Cleavage rate also was significantly higher in group B compared to group A (P = 0.020). Implantation rate and pregnancy rate per transfer was significantly were higher in group B than in group A (24% vs. 15% and 30% vs. 21%).
Conclusion:
Chemical oocyte activation with calcium ionophore resulted in a significant improvement in fertilisation, cleavage, implantation and pregnancy rates after ICSI in infertile patients with previous fertilisation failure.
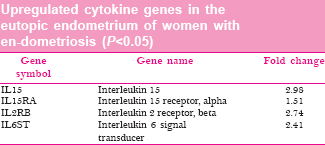
19. Upregulation of genes involved in cytokine production likely contributes to infertility in women with endometriosis
Objective:
Endometriosis is a pro-inflammatory disease leading to infertility in women with endometriosis. Imbalance of cytokine concentrations contributes to increased inflammation in endometriosis. Chronic inflammation of the reproductive system may lead to infertility. The expression levels of genes involved in cytokine production may be altered in the eutopic endometrium of women with endometriosis.
Design:
A prospective case-control study was conducted to assess expression levels of genes involved in cytokine production in the eutopic endometrium of women with endometriosis compared to that of women without endometriosis.
Materials and Methods:
Eutopic endometrial biopsies from 29 women (N = 16 with en dometriosis; N = 13 without endometriosis) was obtained by Pipelle curette between 1 January 2015 and 31 December 2015 in Akanksha IVF centre. Paralleled gene expression profiling using high density oligonucleotide microarrays was applied to investigate dysregulation of cytokine genes in the eutopic endometrium of women with endometriosis compared to women without the disease. Data analysis was conducted by GeneSpring version 4.0.4. T-test using Pvalue >0.05 and a fold-change expression >1.5 was applied to assess statistical significance.
Dysregulated genes were randomly chosen and validated by RT PCR.
Results:
In the eutopic endometrium from women with endometriosis, cytokine genes involved in inflammation were significantly upregulated when compared to women without en dometriosis.
Conclusions:
Upregulation of genes involved in cytokine production likely contributes to increased inflammation thereby leading to decreased pregnancy rates in women with en dometriosis. Increased cytokine production in the eutopic endometrium may contribute to a pro-inflammatory microenvironment and altered immune processes thereby impairing embryo implantation. An improved understanding of the role of cytokines in endometriosis and related infertility may provide new insights into infertility management.
20. Comparison of fresh versus frozen embryo transfer in women with polycystic ovary syndrome
Objective:
The objective of study was to examine the difference in the clinical pregnancy and live birth rates in fresh embryo transfer in vitro fertilisation (IVF) cycles compared to frozen embryo transfer cycles in women with polycystic ovary syndrome (PCOS).
Design:
Retrospective study.
Materials and Methods:
Clinical records were examined of all women with PCOS defined according to Rotterdam criteria, <35 years of age who underwent IVF with An-tagonist cycle in Akanksha IVF centre from 1st Jan 2015 to 31st Jan 2016. Women with terminal Estradiol levels below 2500 pg/ml were triggered with Inj Ovitrelle 250 mcg s/c and based on the number of retrieved oocytes were divided into two groups Group A - less than 15 oocytes retrieved and fresh embryo transfer was done on day 3 and Group B more than 15 oocytes were retrieved and all embryos were frozen on day 3 and transferred in subsequent cycle. Cycles complicated by ovarian hyperstimulation syndrome (OHSS) were excluded. Primary outcomes were clinical pregnancy rates and live birth rates. Secondary outcome were fertilisation rate, implantation rate and miscarriage rate. Statistical analysis was performed using chi square test analysis.
Results:
A total of 106 cycles were included in the study: Group A had 63 fresh transfer and Group B had 43 frozen embryo transfer. Both groups were comparable regarding age, body mass index (BMI), basal follicular stimulating hormone (FSH), Antimullerian hormone (AMH), and antral follicle count (AFC). Clinical pregnancy rates (Group A - 38.6% versus Group B - 42.2%, P= 0.45), Live Birth Rate (Group A: 25.4% versus Group B: 28.6% P= 0.72) were slightly higher in Group B though not statistically significant.
Conclusions:
In women with polycystic ovary syndrome undergoing in vitro fertilisation with serum E2 levels ≤2500 pg/ml, Clinical pregnancy rates and Live birth rates are higher in frozen cycles compared to fresh cycles though studies with larger sample size are required to validate and extrapolate the results.
21. Transvaginal versus transabdominal ultrasound guided embryo transfer: Which one is better?
Objective:
To compare implantation and Fgnancy rates with transvaginal (TV) versus transabdominal (TA) ultrasound guided embryo transfer (ET).
Design:
Randomised parallel arm study.
Setting:
Akanksha IVF Centre, Delhi.
Patients:
Forty eight women undergoing randomised recipients of donor IVF cycles using Antagonist protocol.
Interventions:
Group A: (N = 24) Embryo transfer using TV (with empty bladder, using the Cook ET catheter) versus Group B: (N = 24) TA ultrasound guidance (with full bladder, using the same catheter). Embryo transfer of 2 or 3 good quality embryos was done on day 3.
Main Outcome Measures:
Implantation and clinical pregnancy rates. Duration and difficulty of ET, patient as well as clinician's experience was evaluated by questionnaire. Statistical analysis done using SPSS software with chi square used for qualitative data and students t test for quantitative data.
Results:
Implantation rates and Clinical Pregnancy rates were comparable between the two groups (41.6% vs 45.8% P= 0.8, 33.2% vs 28.6%: P= 0.5, respectively). Mean duration of embryo transfer (104.2 seconds versus 84.8 seconds) was slightly more in transvaginal group however difficulty level was similar. Light to moderate-severe discomfort related to bladder distension was reported by 58.3% of the patients in the TA ultrasound group.
Conclusions:
Transvaginal ultrasound-guided ET yielded similar success rates compared with the TA ultrasound-guided procedure and is associated with increased patient comfort due to the absence of bladder distension and better visualisation specially in obese women.
22. Stress related hypothyroidism leads to infertility in women
Background:
Stress is both cause and effect of Infertility and its treatment. It disturbs gonadotropin secretion, affects uterine and fallopian tube function by catecholamines mediated action and disturbs implantation by immunological process. Hypothyroidism is more common in infertile women (prevalance >6%) and subclinical hypothyroidism (prevalence - 40 50%). Hypothyroidism can effect fertility due to anovulatory cycles, luteal phase defects, hyperprolactinemia, and sex hormone imbalance. Both of them independently affect fertility also stress could lead to hormonal imbalance and thyroid autoimmunity.
Aims and Objectives:
To study the prevalence of hypothyroidism due to stress in infertile women.
Materials and Methods:
Women aged <35 years, trying for conception <2 years, having primary infertility who came for their first consultation regarding infertility were included. Of a total of 600 patients who attended the OPD of Akanksha IVF Centre from 1st January 2015 to 30th September 2015 who met the inclusion criteria (N = 120) were screened using Ryff's Psychological Well-Being Scales (PWB) and underwent routine investigation including thyroid profile. Fifty six women were confirmed to have high stress levels. Based on the presence of stress and thyroid profile women were divided into 4 groups. Group A screened positive for stress and were hypothyroid (N = 38), Group B stress screen positive but normal thyroid profile (N = 18), Group C screened negative for stress but hypothyroid (N = 35) Group D with no stress and normal thyroid profile (N = 29). All 56 women were provided psychological clinical counselling to reduce their stress levels. These women with hypothyroidism were treated for hypothyroidism by administering thyroxine 25–150 mg. Centre's protocol for Infertility treatment followed. Primary Outcomes were Clinical pregnancy Rates in each group by end of 1 year.
Results:
The pregnancy rates were comparable in group A and Group D (26.3% vs 31.03%, P= 0.56) which were higher than in Group B or Group C (22.2% and 20% respectively). The prevalence of hypothyroidism is more in stressed women compared to non stressed women (67.8% versus 54.4% P= 0.08) indicating a stress mediated etiology of hypothyroidism.
Conclusion:
Infertile women were able to conceive with medical treatment of hypothyroidism and stress reducing psychological sessions with in six months. The pregnancy rates being comparable to women without stress or hypothyroidism. Measurement of TSH and psychological well being should be done at early stage of infertility treatment and clinical psychological counselling should be a routine.
Reference
Ryff CD. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. J Pers Soc Psychol 1985;57:1069 108.
Krassas GE. Thyroid disease and female reproduction. Fertil Steril 2000;74:1063 70.
Poppe K, Velkeniers B, Glinoer D. The role of thyroid autoimmunity in fertility and pregnancy. Nat Clin Pract Endocrinol Metab 2008;4:394 405.
Carter JN, Tyson JE, Tolis G, Van Vliet S, Faiman C, Friesen HG. Prolactin-screening tumors and hypogonadism in 22 men. N Engl J Med 1978;299:847 52.
23. Transvaginal sonography: A better diagnostic tool for infertility
Introduction:
Incidence of infertility is increasing worldwide. Infertility in women can be due to systemic (stress and obesity), endocrine related (hypothalmo-pitutitary-ovarian axis), and adnexal (fallopian tubes, uterus, etc) causes. Nearly 30% of infertile women present with anovulation related causes and 70% of them can be easily diagnosed and treated effectively. Thus an accurate diagnosis of anovulatory state is required. The use of transvaginal sonography (TVS) in the management of infertility is gaining increasing popularity. The improved resolution and better tissue textural differentiation offered by TVS makes this technique useful in monitoring ovarian follicular growth, ovulation, and corpus luteum formation, and in evaluating the normal anatomy of the uterus and the cervix and their cyclic response to ovarian steroids. Adnexal and cul-de-sac abnormalities related to infertility can also be identified.
Objective:
To predict the usefulness of transvaginal sonography in infertile women.
Methods:
It is a prospective observational study on 100 infertile women (primary or secondary) attending the MLB Medical College. After taking informed consent, detailed history and clinical examination was performed. Then TVS follicular study was performed on every alternate day after 11 day of menstrual cycle till the evidence of ovulation was detected.
Results:
In 73 cases ovulatory dominant follicle was seen with TVS. In 11 cases non dominant follicle was detected. In 10 cases failure of rupture of follicle was seen. PCOS was detected in 6 cases.
Conclusion:
TVS can be a better and accurate diagnostic tool for infertility. In addition, this method can also provide details of any uterine, endometrial, cervical or adnexal pathology and free fluid collection in pouch of Douglas.
Theme: Clinical
24. Study of histidine-rich glycoprotein polymorphism in unexplained infertility
Objectives:
(1) To study if there is any correlation between the HRG C633T Polymorphism and Ovarian response and Oocyte quality in unexplained infertility group of patients. (2) Does HRG C633T Polymorphism affect the preimplantation aspects (fertilization rate and good quality transferable embryos) of IVF in these patients.
Methods:
Study Design: Prospective, case-control study. Period of study: Six months, June – Nov 2016. Sample Size: Minimum 30 patients in each group of cases and controls. Setting: Ridge IVF Centre, Malka Ganj, Delhi. Inclusion: 20–35 years old women with unexplained infertility, who underwent IVF at our centre. Exclusion: 20 – 35 years old women with other causes of infertility.
Results:
The patients with HRG C633T SNP, C/C genotype have best quality oocytes, fertilization, implantation and clinical pregnancy rates as compared to T/T genotypes.
Conclusion:
The results suggest that HRG C633T single nucleotide polymorphism influences ovarian response.
Theme: Clinical.
25. Assisted reproductive technology outcomes following hatched and hatching embryo transfers compared with expanded blastocyst transfer
Background:
Blastocyst stage embryo transfer (ET) has become routine practice in recent years. Due to limitations of assisted hatching techniques, expanded blastocyst transfer (EBT) is widely done. Not much consideration has been given to spontaneously hatching/hatched blastocyst transfer.
Objectives:
To compare the pregnancy rates of spontaneously hatching/hatched blastocyst against expanded blastocyst transfer after total 5 days of embryo culture. To assess the rates of spontaneous hatching by day 5.
Methods:
Retrospective analysis of embryo transfers following a total 5 days (~120 hours) of embryo culture. Period of study - 18 months (2014 - 2016). Study centre ART centre in a tertiary care hospital.
Results:
There were 252 blastocyst transfers over two years, of which 201 were expanded blastocyst transfer, 32 had hatching blastocyst transfer and 19 had hatched blastocyst transfer. The average embryo culture duration in fresh transfers was 110-117 hours. In frozen embryo transfer (FET) cycles, the embryos that had been vitrified at 72 hours of culture were further warmed and cultured for another 48 hours prior to transfer. In FET cycles, (n-136) 21 patients had hatching embryos and six patients had hatched embryos. In the Fresh ET cycles (n-116) 11 and 14 patients had hatched and hatching embryos.
The pregnancy rates were 36.6% in expanded blastocyst transfers while 50% and 61% in the hatching and hatched blastocyst transfers respectively.
Conclusion:
Spontaneous hatching/hatched blastocysts after a total 5 days of culture have higher chances of pregnancies when compared to the embryos that reached full expansion only after 5 days of culture.
26. Secondary hypogonadotropism and microadenoma-successful pregnancy outcome with dopamine agonists and in vitro fertilization using antagonist protocol: Case series
Low gonadotropin concentrations can be due to congential or acquired factors, and can present as isolated deficiency or combined with other pituitary hormone deficiencies.1 Hypogonadotropism occurring after puberty, is revealed by secondary amenorrhea in women, decreased libido in men. The hormonal diagnosis is easy in the complete forms with usually undetectable plasma LH, FSH and sex steroid levels. In the partial forms, plasma gonadotropin levels may be in the low normal range with slightly decreased plasma sex steroid levels. Treatment requires only substitution when fertility is not sought. Treatment of infertility has to be individualized. GnRH agonists (pulsatile) and gonadotropins are successful in restoring fertility. We report two cases of hypogonadotropism (markedly decreased gonadotropin levels without clinical evidence of hypogonadism) who presented to our clinic with primary infertility. Other pituitary hormones were within normal range for both the patients except in second patient prolactin was marginally high. In our first patient, there was non functional pituitary microadenoma which could explain hypogonadotropism, while in second patient no obvious cause could be found. Our first patient was put on cabergoline in view of pituitary adenoma although there was no hyperprolactinemia. In both patients, successful pregnancy was achieved with In vitro fertilization using antagonist protocol. Role of cabergoline in non functional pituitary adenoma is discussed. Role of in vitro fertilization when indicated for achieving pregnancy in such cases is discussed.
Theme: Clinical
References
Carter JN, Tyson JE, Tolis G, Van Vliet S, Faiman C, Friesen HG. Prolactin.screening tumors and hypogonadism in 22 men. N Engl J Med 1978;299:847.52.
27. A survey on the prevalence of depression and violence among infertile women attending SSH, Varanasi
Objective:
To assess the prevalence of depression and physical/mental violence among patients with female infertility.
Method:
A prospective study was designed to study the prevalence of depression; verbal and physical violence among women with infertilty attending infertility clinic at Sir Sunderlal Hospital, BHU. The sample entailed of 278 infertile female who satisfied the following inclusion criteria: (1) At fertility age 20-45. (2) Had infertility of minimum 1 year duration.
Results:
The prevalence of depression among women with primary infertility was 75.5% and that in secondary infertility was 73.1%. Suicidal tendencies were present in 37.7% and 7.3% in primary and secondary female infertility respectively. Depression in rural population was 76.8% and urban was 74.3%. Sixty six percent of women with infertility had suffered abuse, either physical or verbal, out of which 16.3% suffered both physical and verbal abuse by husband or in-laws. Depression was present in 88% and suicidal tendencies in 41% of women who suffered domestic abuse, either physical or verbal. But suicidal tendencies increased to 67% in women who suffered both physical and verbal abuse.
Conclusion:
This study showed that depression and suicidal tendencies were higher in women suffering from primary than secondary infertility; and higher in the rural than the urban population. The prevalence of depression and suicidal tendencies were much higher in women facing physical or verbal abuse, than those who had supportive husband and in-laws. Thus addressing the psychological needs of an infertile woman is important as psychotherapy in the form of Cognitive Behavioral Therapy may prevent the surge in depression and could presumably lead to increased pregnancy rates.
Theme: Clinical.
28. Correlation of serum anti-mullerian hormone with various parameter's in polycystic ovary syndrome patients
Introduction:
PCOS is one of the most common endocrine disorders of women of reproductive age group with a prevalence of approximately 6-10%. Studies have shown that serum AMH levels are 2-3 folds higher in PCOS women and it's level are in correlation with serum LH, FSH, and LH/FSH ratio in PCO patient.
Objective:
To study the correlation of AMH with various parameter's in PCOS (LH, FSH, LH/FSH).
Material and Methods:
Serum AMH along with other markers like LH, FSH, LH/FSH ratio was analysed in 60 PCOS patients diagnosed as per Rotterdam criteria and 60 healthy controls. Correlation between serum AMH and parameters like serum LH, FSH LH: FSH ratio was analysed.
Results:
Serum AMH was significantly raised in PCOS patient's compared to control group (11.95 ng/ml vs 3.68 ng/ml, P< 0.001) and it showed a significant positive correlation with LH: FSH ratio, and significant negative correlation with serum FSH, and a positive but insignificant relationship with serum LH.
Conclusion:
Serum AMH is positively correlated with serum LH/FSH ratio and has a significant negative correlation with FSH levels.
Lacunae: Limited sample size as there were only 60 cases and controls in this study.
29. Study of embryogenesis in vitro fertilisation in different phenotypes of poly systic ovary syndrome
Objective:
To compare the fertilization rate, Total no. of oocytes, MII oocytes and good quality embryos in all phenotypes.
Methods:
It is prospective single centrestudy. All the patients were comparable and stimulate according standard Ivf protocol.
Duration:
March 2016-Nov 2016. Following are four groups: (i) GROUP 1: PCO morphology + Oligoanovulation. (2) GROUP 2: PCO morphology + Hyperandrogenemia. (3) GROUP 3: Oligoanovulation + Hyperandrogenemia. (4) GROUP 4: All the above.
Results:
We found good quality embryos in PCO patients with morphology and hyperandrogenemia. It is statically significant.
Conclusion:
Hyperandrogenemia patients with PCO morphology provide better results in terms of good quality embryos.
Theme: Embryology
30. Study of in vitro fertilization outcome in different polycystic ovarian syndrome phenotypes
Objective:
This prospective single centre study is designed to analyse the result of IVF treatment in different phenotypes of 100 PCOS patients.
Duration:
March 2016–November 2016.
Material and Methods:
Study participants were divided into: Group 1 – PCO morphology + Oligoanovulation, Group 2 – PCO morphology + hyperandrogenism, Group 3 – Oligoanovulation + hyperandrogenism, Group 4 – All the three. They were compared regarding the number of oocytes, fertilization rate, embryo quality and pregnancy rates. They were further subdivided into: Group A – High AMH and LH, Group B – High LH, Group C – High AMH. And pregnancy rates compared between them.
Results:
Of the 382 women studied, 92 were in PCOS group while 290 were in control group. Mean AMH/AFC ratio in PCOS group and control group was 1.82 and 1.01 respectively. It was significantly higher in PCOS group. There was no significant difference in the mean AMH/ovarian volume ratio of both groups. While no correlation between AMH and BMI was seen in control group (r = 0.04, P> 0.05), AMH was inversely correlated with BMI in PCOS group (r = 0.36, P< 0.005).
Conclusion:
Women PCO morphology and hyperandrogenism had a significantly higher embryo quality.
The high AMH group had a significantly increased pregnancy rate after correction of the level with metformin pre-treatment.
Theme: Clinical.
31. Adult granulosa cell tumor-A differential diagnosis to be considered in clomiphene failure infertility
Granulosa cell tumors are rare sex cord stromal tumors of the ovary. They may present with features of hyperestrogenism. We present a case of 29 year old nulliparous lady, with infertility and oligomenorrhoea, initially managed with a provisional diagnosis of polycystic ovarian syndrome. She did not respond to multiple cycles of ovulation induction with clomiphene citrate. Later an ovarian cystic mass was detected and she was planned for laparoscopic cystectomy. She was lost to follow up for 3 months. MRI pelvis revealed a solid looking mass in the ovary, with increased vascularity. FNAC from the mass suggested granulosa cell tumor. She underwent staging laparotomy with fertility preserving surgery. Thereafter she conceived on first cycle of clomiphene citrate. Ongoing pregnancy is currently in its third trimester. Concluding, a high index of suspicion for underlying malignancy in cases of clomiphene resistant infertility with ovarian cysts, is advisable.
32. Retrospective comparative study between cyproterone acetate and ethinyl estradiol in patients with polycystic ovarian syndrome
Introduction:
Polycystic Ovarian Syndrome (PCOS) is one of the most common causes of oligomenorrhoea and anovulatory cycles. In 1935, Stein and Leventhal described a syndrome in women which consisted of amenorrhoea, infertility, hirsutism, and was associated with bilateral, enlarged, cystic ovaries. Other features like abortion and acanthosis nigricans are also found.
Aim:
To evaluate the outcome of combined therapy of cyproterone acetate and ethinyl estradiol in patients with PCOS.
Materials and Methods:
This study was conducted in the Department of Obstetrics and Gynaecology of M.G.M Medical College, M.Y. Group of Hospitals, Indore (M.P.) and was carried out over 12 months from SEP 2015 to AUG 2016. The patients were selected from GOPD, Department of OBG MYH Indore. In the study, 100 patients were randomly included at the time of enrollment.
Results:
The results of this study show that the combination of low dose estrogen and Cyproterone acetate successfully reduce the hormonal disturbances which characterize PCOS. Apart from the normalization of the hormonal profile the decrease in ovarian size, beneficial effects observed on acne, hirsutism and regulation of menstrual cycles are remarkable also CPA + EE treatment shows beneficial effects on improving infertility status.
Conclusion:
Diagnosis is made by typical clinical features along with hormonal assays and ovulation studies. TVS is a new eye in the diagnosis of minute pelvic pathology. Various modalities of treatment have been tried to manage the constellation of symptoms of PCOS. CPA + EE is a recent advance in the field of management of PCOS. It has shown anti-androgen effects on PCOS patients clinically, biochemically and on ovarian morphology.
33. Demographic predictors of IVF outcomes-A retrospective analysis
Background:
The study involves analysis of age, AMH and BMI, as a predictor of oocyte quality and usable embryos.
Objective:
To determine the impact of age, AMH and maternal metabolic state on oocyte development and quality of embryos in women undergoing in vitro fertilization/intracytoplasmic sperm injection (IVF/ICSI) cycles. A retrospective analysis of cohort of women undergoing IVF/ICSI from August 2015-September 2016 in a tertiary care fertility center ere analyzed.
Method:
Total of 180 IVF/ICSI self cycles were stratified into cohorts based on BMI (<18, 18-24.9, 25-29.9, 30-39.9, >40); age (20-30 years, 31-35 years, >36 years) and AMH levels (<1 ng/dl, 1 3 ng/dl, >3 ng/dl).
Results:
Comparison was done based on the parameters of number of oocytes retrieved, quality of oocytes, fertilization rate and total usable embryos. Age group (20-30) years and AMH levels of 1-3 ng/dl had a statistically significant better oocyte quality, fertilization rate, and total usable embryos. BMI per se has no effect on all of the above.
Conclusion:
Age group of 20-30 years and AMH in the range of 1-3 ng/dl shows a significant improved oocyte quality and fertilization rates, Obesity measured in terms of parameters of BMI on its own does not conclusively effect the results of IVF as per the outcomes found in our study in terms of success rate. Hence BMI per se does not necessarily effect the folliculogenesis and oocyte quality though other variables i.e PCO could effect outcome in such cases.
Theme: Clinical
34. Infertility management and ethical dilemmas
Objective:
To audit cases of infertility with ethical dilemmas.
Design:
Retrospective case based reviews from January 2015 - December 2015.
Materials and Methods:
Cases where patients were advised ART treatment for achieving conception but the clinical or demographic status were deemed ethically challenging, and where ICMR guidelines were consulted for further information and justification of performing assisted reproductive technique. If ICMR guidelines were inadequate in providing information, advise of ART lawyer was taken prior to going ahead with the treatment.
Results:
10 cases of varied clinical situations with varied ethical dilemmas were reviewed. The type of cases included – (i) Clinical situations with regards to egg donor cases - 2 cases. (ii) Clinical situations with regards to preserving fertility - 2 cases. (iii) Clinical situations with regards to surrogacy cases - 4 cases. (iv) Clinical situations with regards to male factor infertility - 2 cases.
Conclusion:
We recommend that ICMR guideline to be comprehensive and legally binding.
Theme: Clinical.
35. A prospective cohort study of causes of recurrent pregnancy loss in North Indian population
Objective:
To identify causes of recurrent pregnancy loss in a cohort of North Indian population.
Methods:
A prospective cohort study was carried out in department of Obstetrics and Gynecology, PGIMER, Chandigarh. The study enrolled 89 patients aged 22 to 40 years of age during preconceptional period with a history of two or more pregnancy losses at less than 24 weeks of gestation. A detailed history, thorough clinical examination and investigations with a certain group of pre-decided laboratory tests were done to ascertain the causes of recurrent pregnancy loss.
Conclusion:
Endocrinological abnormality like deranged blood sugars were found in 11.2%; hypothyroidism in 3.4%; uterine anomalies and other ultrasonological abnormalities in 6.7%;abnormal karyotype in one of the partners in 6.7%; APLA positivity in 11.2% patients among the recruited cohort. Thus recurrent pregnancy loss could be explained in 39.2% patients. For rest 60.8% patients cause for recurrent pregnancy loss remained unexplained.
Theme: Miscellaneous.