Translate this page into:
Acute abdomen in ART pregnancy
Address for correspondence: Dr Papa Dasari, Senior Professor, Department of Obstetrics and Gynaecology, Women and Children Hospital, JIPMER, Gorimedu, Puducherry, India. Pin Code: 605006. E-mail: dasaripapa@gmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Acute abdomen during late pregnancy is a rare event. A 35-year-old second gravida with a history of previous early pregnancy loss, and two in vitro fertilization failures was hospitalized following the development of hypertension at 25 weeks and 6 days of pregnancy. She conceived under donar oocyte program because of low ovarian reserve due to stage IV endometriosis. She was type II diabetes mellitus and her blood sugars were controlled with Metformin and Insulin. At 32 weeks and 4 days of gestation, she had sudden onset pain abdomen and developed eclampsia. Preterm labor and placental abruption were suspected but there were no findings suggestive of abruption on ultrasonography. She had persistent diffuse pain abdomen and developed tachycardia and worsening pallor over 4 hours for which laparotomy was performed. At laparotomy, there was 1.5 L of hemoperitoneum due to ruptured endometriotic cyst which was adherent at fundus of uterus. Alive male baby 1.9 kg was delivered and partial cystectomy was undertaken. Both mother and baby were discharged after 14 days. Endometriosis though believed to regress during pregnancy, it can rupture during pregnancy and result in life-threatening situation.
Keywords
Acute abdomen
assisted reproductive techniques
endometriosis
hemoperitoneum
pregnancy
INTRODUCTION
Abdominal pain in pregnancy is a common symptom but sudden onset pain which is severe warrants an urgent and detailed evaluation. The incidence of acute abdomen in pregnancy varies from 1 in 500 to 6350.[1] Causes of acute abdominal pain in early pregnancy include rupture ectopic pregnancy, torsion ovarian cyst, urinary tract infection, etc. In pregnancies following assisted reproductive techniques (ART), ovarian hypertstimulation and torsion of enlarged ovary are usually thought of.[2] The common causes for abdominal pain in late pregnancy include obstetric causes such as preterm labor, placental abruption, acute polyhydramnios, degeneration of pre-existing fibroid uterus, rupture uterus, and nonobstetric causes such as acute appendicitis, intestinal obstruction, and cholelithiasis. Diagnostic difficulties are experienced in arriving at diagnosis when ultrasonography (USG) of fetus and placenta is normal. Hemoperitoneum due to endometriotic cyst rupture during late pregnancy is a rare event and hence this case is reported.
Case report
A 35-year-old second gravida with history of previous early pregnancy loss was admitted at 25 weeks and 6 days of pregnancy in view of hypertension through emergency services. This pregnancy is following donor oocyte program performed for low ovarian reserve due to stage IV endometriosis. She was on progesterone support and underwent cerclage at 16 weeks of pregnancy.
She attained menarche at 12 years of age and periods were regular. She had second degree consanguineous marriage at the age of 32 years and was diagnosed to have right-sided endometriotic cyst (3.7 × 4.7 cm) during evaluation for infertility. She was diagnosed to be type II diabetes mellitus since 2016 and was on Metformin therapy. She was initially treated with oral contraceptive pills for 6 months and one cycle of ovulation induction with Letrozole. Later she underwent hysterolaparoscopy elsewhere in 2018. The findings documented were the uterus was normal and bilateral tubes were patent. Pouch of Douglas (POD) was obliterated due to dense adhesions and there were bilateral endometriomas. The size of the endometriomas was not mentioned in the operative notes. Bilateral ovarian cystectomy was performed. This was followed by medical treatment with injection Leuprolide acetate 3.75 mg (three doses given at monthly intervals). Later she received one cycle of Leterozole (2.5 mg) and one cycle of Leterozole and hMG for ovulation induction and advised timed intercourse. In December 2018, she consulted us for ART. Her anti-Müllerian hormone was 0.9 ng/dL and transvaginal ultrasound showed posterior wall adenomyoma 2.8 × 2 cm, right ovary showed 2.2 × 2.7 cm endometriotic cyst, and there were no follicles. Left ovary was visualized posterior to uterus and showed four antral follicle count. She was recruited for ART in March 2019. Her follicle-stimulating hormone was 11.7 IU/L, LH 3.6 IU/L, and E2 32 pg/mL. Ovarian stimulation was carried out with rFSH with antagonist protocol. Her estradiol was 3289 pg/mL, P4 was 0.82 ng/mL, and human chorionic gonadotropin trigger was given. Seven oocytes were retrieved which resulted in six grade I embryos of eight-cell stage. Fresh transfer of three embryos was carried out and pregnancy did not occur. She underwent frozen embryo transfer of three remaining grade I embryos in July 2019 and pregnancy was confirmed which later resulted in early pregnancy loss.
The USG in July 2020 showed uterus 7 × 3.3 × 4.8 cm; right ovary 4 × 4.2 cm with chocolate cyst of 2.5× 1.8 cm; and left ovary showed chocolate cyst of 5.3× 2.2 cm with low level internal echoes and appeared to be adherent posterosuperior aspect of uterus. She underwent embryo transfer under donor oocyte program elsewhere in hormone replacement therapy (HRT) cycle with downregulation using injection Leuprolide acetate in August 2020 which resulted in the current pregnancy. Pregnancy was confirmed on September 18, 2020 with transvaginal ultrasound which showed intrauterine gestational sac and there was no comment regarding endometriotic cyst either during this scan or subsequent scans.
Since hospitalization at 25 weeks and 6 days of gestation, her blood sugars were controlled with Metformin and Insulin. Her pregnancy was supported with progesterone and she received antenatal corticosteroids for fetal lung maturity at 29 weeks under buffered dextrose cover to keep blood sugars under control. Her hemogram and other investigations such as liver function test and renal function test were normal. Her serial ultrasound showed fetal growth to be optimal and umbilical artery PI = 0.9. Placenta was implanted posteriorly and low lying. There were no findings regarding visualization of any ovarian cyst. At 32 weeks and 4 days of gestation, she complained of sudden pain abdomen following abdominal examination by undergraduate students. On examination, she was conscious and pulse rate was 100/minute, BP 130/80 mmHg, and SPO2 was 98% on room air. Her respiratory and cardiovascular examinations were normal. Her uterus was 34 weeks, irritable, and tender, fetal heart sound (FHS) 140/minute regular. Per vaginal examination cervix was 2 cm long and there was no bleeding per vaginum. On USG, cardiac activity was good and there was no retroplacental hemorrhage, amniotic fluid index (AFI) was 18 cm, uterine artery was PI = 0.9, and estimated fetal weight was 1.8 kg.
After 10 minutes of examination, she developed an episode of generalized tonic clonic convulsions followed by loss of consciousness for 2 minutes. She was treated as a case of eclampsia and started on magnesium sulfate and received zero hour of MgSO4 regimen (Dakha Protocol). Patient was monitored continuously in eclampsia room and was assessed for abruption and preterm labor. Initially tocogram showed irregular uterine contractions of 40 mmHg and hence injection Terbutaline 0.25 mg was given subcutaneously. Pain abdomen persisted and cervical cerclage was removed and there was no evidence of bleeding through os. As the gestational age was 32 weeks and baby weight was 1.9 kg decision for immediate termination by LSCS was deferred and she was monitored for 4 hours for improvement of symptoms of pain abdomen and to explore the cause of acute abdomen. USG was repeated by radiologist after 4 hours and there were no signs of abruption but minimal free fluid was noted in flanks. Her general condition showed gradual increase in tachycardia from 92 to 120 bpm without hypotension and she developed mild pallor. Her bleeding time was 2 minutes and clotting time was 6 minutes 50 seconds. Prothrombin time was 13.3, INR 1.12, and Hb 7.3 g%.
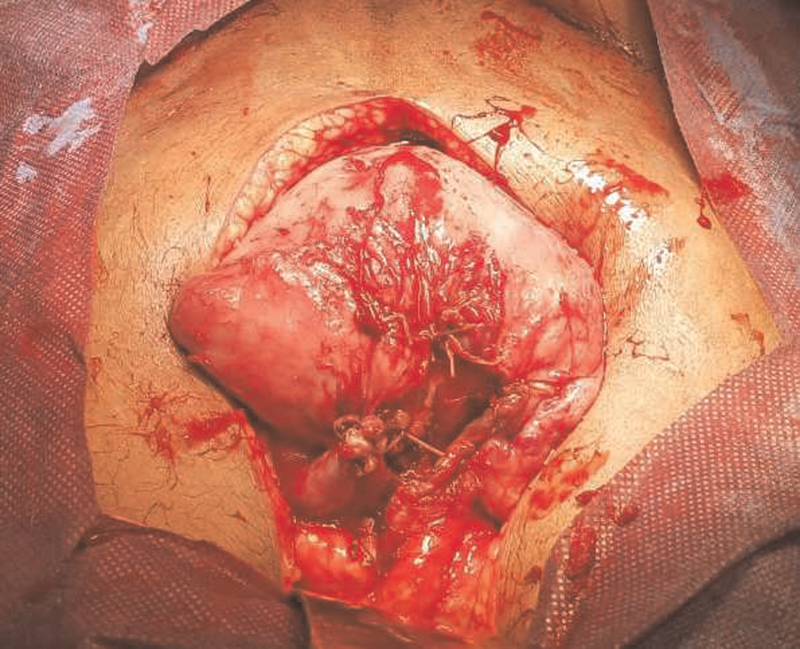
She was taken up for laparotomy with suspicion of concealed abruption after taking high-risk consent. At laparotomy, hemoperitoneum was present. LSCS was performed, and an alive female baby of weight 1.99 kg delivered with an Apgar scores of 3/10 and 7/10 at 5 and 10 minutes, respectively. There were no retroplacental clots and uterine atony was managed medically. Hemoperitoneum was approximately 1.5 L and the source of bleeding was found to be from posterosuperior aspect of the uterus, where endometriotic cyst was adherent and ruptured with multiple dilated vessels [Figure 1 a, b]. Part of the cyst wall was excised and hemostatic sutures were applied [Figure 2]. Right ovary was adherent to sigmoid colon and POD was obliterated. Abdomen was closed after inserting an intraperitoneal drain. She received 2 units of packed red blood cells and four fresh frozen plasma intraoperatively.

- (a) Superior aspect of uterus after delivery of fetus and placenta. Bleeding source is shown with artery forceps. (b) Superior aspect of uterus with bleeding vessels secured with two artery forceps.
- Superior aspect of uterus after cystectomy and partial salpingectomy.
Immediate postoperative pulse rate was 106 bpm and her BP was 160/100 mmHg. She received magnesium sulfate regimen and tablet Labetalol for 24 hours along with insulin infusion for control blood sugar. The neonate was in neonatal intensive care unit (NICU) on ventilation for 24 hours received one dose of surfactant and had transient hypoglycemia which was treated. Postoperatively the mother received one unit of packed cells and sutures were removed on day 10. Baby was in NICU for 10 days.
DISCUSSION
Pregnancy is expected to decrease the symptoms and signs of endometriosis but cases of endometriotic cyst rupture during early pregnancy were reported in 1993 and 1998.[3,4] This possibility was not thought of in the current woman being reported, as she had treatment for stage IV endometriosis and underwent laparoscopic cystectomy 3 years prior to this pregnancy and its recurrence during this pregnancy was not reported though she had undergone USG several times. Diagnosis of hemoperitoneum during late pregnancy is difficult due to enlarged uterus and the only clinical feature that clinch the diagnosis is sudden onset severe diffused or localized pain and rapid progression to shock.[5] Though this woman had sudden onset abdominal pain which is diffused, she did not develop shock immediately and the only signs are progressive tachycardia and persistent tenderness of abdomen.
Hemoperitoneum can also result due to rupture of aneurysm of splenic artery as well as dilated high pressure veins of ovary and broad ligament. The preoperative diagnosis of hemoperitoneum is difficult even by USG after 32 weeks and can only be performed by diagnostic USG tapping. In this woman, the clinical picture was complicated by eclampsia, and hence abruption and preterm labor were the initial diagnoses. Rupture of subcapsular hematoma of the liver in HELLP syndrome is another differential diagnosis[6] but this lady did not have HELLP syndrome and her hemogram was performed regularly and she did not require antihypertensives as she remained as mild gestational hypertension since admission. Magnetic resonance imaging (MRI) is preferable modality to visualize soft tissues and should be carried out when USG cannot ascertain the cause in acute abdomen during pregnancy. MRI has a sensitivity of 100% and specificity of 98%, but its availability on emergency basis is the limiting factor in most of the centers.
The other obstetric causes of acute abdomen during pregnancy include red degeneration of fibroid uterus, round ligament pain, and torsion of gravid uterus. A case of fibroid uterus with red degeneration at 27 weeks of pregnancy which resulted in hemoperitoneum due to rupture of vessels necessitating hysterectomy and delayed diagnosis was reported.[7] A case of round ligament varicocele presenting as acute abdomen was reported by Cicilet[8] which was diagnosed by Doppler USG and managed conservatively. Spontaneous hemoperitoneum during late pregnancy is also on record; however, later after extensive exploration, this was proved to be chronic bleeding from tubal ectopic pregnancy.[9]
The diagnosis of hemoperitoneum during late pregnancy is rarely made and most often mistaken for abruption due to acute sudden onset abdominal pain. Hemoperitoneum due to rupture of physiologically enlarged utero-ovarian vessels as a result of increased venous pressure was hypothesized. Sudden rise in venous pressure can occur during defecation, coughing, and straining in second stage of labor.[10] Spontaneous rupture of uterine vessels in pregnancy complicated by endometriosis was reported in 1996[11] in a 28-week primigravid woman who had progressive anemia, fetal decelerations, and shock with pain abdomen. At laparotomy, there was 4 L of hemoperitoneum and lacerations at fundus of uterus due to endometriosis. In the present woman also, endometriosis at uterine fundus was more evident in the form of a cyst wall with source of hemorrhage. Hemoperitoneum due to rupture of endometriotic cyst in twin pregnancy following in vitro fertilization (IVF) was reported at 27 weeks of pregnancy in which difficulties were experienced in diagnosis of hemoperitoneum.[12] Preterm labor and acute appendicitis were the initial considerations, and MRI was also inconclusive in diagnosing hemoperitoneum and the woman was taken for laparotomy due to significant decrease in hematocrit. There was 1.5 L of hemoperitoneum and the source of bleeding was from left-sided endometrioma posterior to uterus which was buried in adhesions around sigmoid colon.
A case of hemoperitoneum in twin pregnancy following IVF was reported by Emek Doger and collegues,[12] in which the posterior surface of uterus had a bluish color and bleeding from utero-ovarian vessels. They reviewed the literature and found four such cases of endometriosis associated with twin gestation in IVF pregnancies. They postulated that the damage during ovum pick up might have predisposed to utero-ovarian vessel rupture as they could not ascertain the diagnosis of endometriosis in their case. In the current woman, excessive abdominal pressure by abdominal palpation may be a predisposing factor for rupture of endometriotic cyst which was adherent at fundus of uterus. For the current pregnancy, donar oocytes were used and she underwent only embryo transfer in a cycle downregulated by GnRH agonist. Hemoperitoneum should form one of the differential diagnoses in pregnant women with sudden abdominal pain and nonspecific symptoms such as vomiting. Acute anemia also should be considered as indirect evidence for hemoperitoneum and early intervention is essential to save maternal and fetal life.[13] Labor may mask the symptoms of rupture ovarian cyst which can be diagnosed in the postpartum period if hemorrhage is not catastrophic.[14]
CONCLUSION
Literature and the present study confirm that rupture of endometriotic cyst during pregnancy can occur causing catastrophic intraperitoneal hemorrhage. Development of acute pain abdomen should rise suspicion of hemoperitoneum in women with endometriosis who conceive after ART.
Authors contributions
PD: Overall management of patient and manuscript preparation; MC: Laparotomy and manuscript checking; Priya: Drafting case report; Niranjana: assisting in surgery.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Clinical review − Abdominal pain in pregnancy. https://www.gponline.com/clinical-review-abdominal-pain-pregnancy/obstetrics/obstetrics/article/968728
- Acute abdomen in early pregnancy due to ovarian torsion following successful in vitro fertilization treatment. Taiwan J Obstet Gynecol. 2015;54:438-41.
- [Google Scholar]
- Case report of ruptured endometriotic cyst in pregnancy treated by laparoscopic ovarian cystectomy. Singapore Med J. 1998;39:368-9.
- [Google Scholar]
- Management of acute abdomen in pregnancy: current perspectives. Int J Women Health. 2019;11:119-34.
- [Google Scholar]
- A case of HELLP syndrome resulting in hemoperitoneum and hyperammonemia. Am J Gastroenterol. 2018;113:S1669.
- [Google Scholar]
- A rare case of large uterine myoma in an antenatal women with situs inversus: a case report. Obstet Gynecol Cases Rev. 2019;6:144.
- [Google Scholar]
- Acute groin pain in pregnancy: a case of round ligament varicocele. BJR Case Rep. 2017;3:20150517.
- [Google Scholar]
- Idiopathic spontaneous haemoperitoneum in the third trimester of pregnancy. Ghana Med J. 2012;46:258-60.
- [Google Scholar]
- Spontaneous rupture of the uterine vessels in a pregnancy complicated by endometriosis. Acta Obstet Gynecol Scand. 1996;75:860-2.
- [Google Scholar]
- Spontaneous severe haemoperitoneum in the third trimester leading to intrauterine death: case report. Case Rep Obstet Gynecol. 2011;2011:PMC3335503.
- [Google Scholar]
- Rupture of endometriotic ovarian cyst causes acute hemoperitoneum in twin pregnancy. Fertil Steril. 2011;95:2125.e1-3.
- [Google Scholar]
- Spontaneous rupture of uterine vein in twin pregnancy. Case Rep Obstet Gynecol. 2013;2013:596707.
- [Google Scholar]
- Labor may mask a symptom of the rupture of ovarian endometrial cyst: a case report. Clin Case Rep. 2018;6:1128-31.
- [Google Scholar]







