Translate this page into:
Clomiphene citrate usage pattern in India: A knowledge, attitude, and practice survey among gynecologists
Address for correspondence: Dr. Sonia Malik, Program Director, Southend Fertility and IVF, SVASMED Pvt Ltd, 1st Floor, C-1 Market, Vasant Kunj, New Delhi - 110070, India. E-mail: sm_doc@southendivf.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Clomiphene citrate (CC) has an important place in therapy for management of ovulatory dysfunction. The objective of the present survey was to understand the knowledge, attitude, and practice (KAP) of Indian gynecologists toward the use of CC.
Materials and Methods:
A prospective, cross-sectional, observational, questionnaire-based KAP survey conducted among Indian gynecologists. Out of 22 multiple-choice questions (MCQs), 9 questions were related to efficacy, 5 to safety, and 8 to perception about CC usage in routine clinical practice. Data were summarized by percentages in frequency tables and graphs.
Results:
Seven hundred seventy-one gynecologists in total across India participated in this survey. The majority of the participants preferred CC in treatment of ovulatory dysfunction associated with polycystic ovary syndrome (PCOS). The ovulation rate was reported to vary 21-60% and the pregnancy rate was noticed to be 11-30% by the majority of the participants. CC was reported to have very good to excellent efficacy and tolerability. Resistance to CC was encountered sometimes. Commonly encountered adverse effects included abdominal/pelvic discomfort or pain, ovarian enlargement, and nausea and vomiting. Frequent complications included multiple gestation, ovarian hyperstimulation syndrome (OHSS), and spontaneous abortion. Quite a few doctors reported congenital malformations with CC therapy. A majority of participants preferred CC in a dose of 50-100 mg/day for 5 days starting on the second or third day of the cycle. Most participants advised natural conception to patients receiving CC therapy. Metformin and gonadotropins were the preferred drugs coadministered with CC treatment.
Conclusion:
The present KAP survey highlighted CC as a commonly used agent for ovulatory dysfunction, with very good to excellent efficacy and tolerability.
Keywords
Clomiphene citrate (CC)
India
knowledge attitude and practice (KAP) survey
INTRODUCTION
Ovulatory dysfunction is an important and common cause of failure of reproduction in cases of female infertility,[1] and it is mainly caused by hypothalamic-pituitary failure/dysfunction and ovarian failure.[2] Anovulatory infertility is responsible for approximately 40% of cases of female infertility.[3] Polycystic ovary syndrome (PCOS) is a leading cause and some other causes may be obesity, extreme weight loss, exercise or other stress, hyperprolactinemia, pituitary tumors, or thyroid disease. Anovulatory infertility may require evaluation to detect underlying systemic disease, followed by specific treatment.[4]
Treatment for ovulatory dysfunction is induction of ovulation, and clomiphene citrate (CC) is considered as the drug of choice for the same. CC is a competitive estrogen antagonist used for the induction of ovulation. It binds to the estrogen receptor (ER) and depletes its concentrations by interfering with its replenishment. Decreased estrogen, by feedback mechanism, will trigger pulsatile secretion of hypothalamic gonadotropin-releasing hormone (GnRH) to increase the release of luteinizing hormone (LH) and follicle-stimulating hormone (FSH), which will, in turn, stimulate ovarian follicular activity. In successful cycles, one or more ovarian follicles will mature. CC is given orally, has few side effects, and is easily available and inexpensive, as a result of which this drug is widely prescribed.[3,4]
A knowledge, attitude, and practice (KAP) survey measures, through a structured, standardized questionnaire, changes in the knowledge, attitude, and practice of a person in response to a specific intervention. A KAP survey is a representative survey conducted on a particular population on a specific topic. These surveys are popular and widely used because they utilize fewer resources and tend to be more cost-effective than other social research methods.[5]
There are limited data about the knowledge, perception, and routine clinical usage pattern of CC among medical practitioners in India. The present survey was undertaken to explore Indian medical practitioners' knowledge, perception, and usage of CC in the real-life setting.
MATERIALS AND METHODS
Survey design and setting
This was a prospective, cross-sectional, observational, questionnaire-based survey conducted across India from September 2014 to March 2015.
Survey participants
Registered medical practitioners with recognized qualifications in Obstetrics and Gynecology (MS/MD/DGO) working in public and private clinics/hospitals participated in this survey.
Survey instrument
A specially designed, structured, self-completion survey questionnaire was filled in by gynecologists, based on their prior clinical experience and knowledge of usage of CC. The survey assessed the gynecologists' knowledge, attitude, and practice toward the use of CC in routine clinical practice. The questionnaire consisted of 22 multiple-choice questions (MCQs), out of which 9 questions were related to efficacy, 5 to safety, and 8 to perceptions about CC usage in routine clinical practice.
Efficacy-related questions included the following: The preferred patient profile for CC; observed ovulation rate, thickness of endometrium, and pregnancy rate; cycles of CC required for conception; global assessment of efficacy; additional drug(s) needed for ovulation induction; criteria for CC resistance and its occurrence. Safety-related questions included the following: Commonly observed adverse effects, complications, and any congenital malformations with CC; percentage of patients developing ovarian hyperstimulation syndrome (OHSS); and global assessment of tolerability. Perception-related questions included preferred dose, duration, and day to start CC; size of Graafian follicle to stop CC; additional drug(s) prescribed to improve endometrium; preferred day to start estrogen; method of conception advised; and additional drug(s) prescribed in addition to CC for the same.
Data analysis
Categorical data were summarized by number N and percentage (%) in each category, where N represents the total number of participants responding to each question. Data were summarized in frequency tables and graphs. Not all participants answered all the questions; few participants have responded to more than one option for many of the questions.
Ethical considerations
As this was a survey and no patient-related data were captured, Ethics Committee approval was not necessary and hence not obtained. Similarly, as this was not a clinical trial, no clinical trial registration was required.
RESULTS
In total, 771 gynecologists participated in this survey across India. The final data from 771 participants' responses were evaluated and analyzed as follows.
Efficacy assessment of CC
The majority of participants (89.47%) preferred CC for PCOS. Secondary amenorrhea, psychogenic amenorrhea, amenorrhea-galactorrhea syndrome were other conditions in which CC was preferred [Table 1].

Approximately 77% of the participants reported ovulation rates (percentage of patients ovulating with each cycle of CC 50 mg) varying in the range 21-60% [Figure 1].

- Ovulation rate with CC
Almost 90% of participants reported the thickness of endometrium as being 7-10 mm with CC [Table 2].

A total of 45.3% participants noticed a pregnancy rate [gestational sac on ultrasonography (USG)] of 11-20%, while 34% participants noticed a pregnancy rate of 21-30% with each CC cycle [Figure 2].

- Pregnancy rate with CC
According to a majority of participants (62.76%), 3-4 cycles of CC were required for conception, while 30% of participants observed that almost 5-6 cycles were required for conception [Table 3].

As per the global assessment of efficacy, approximately 65% of participants rated the efficacy of CC as very good to excellent, and 35% rated it as average [Figure 3].

- Global assessment of efficacy of CC
According to 82% of participants, less than half the patients required additional drug(s) for induction of ovulation [Table 4].

A majority of participants (65.13%) considered CC resistance when patients failed to ovulate with the maximum dose of 150 mg of CC in 3 cycles [Table 5].

Approximately 79% and 18% of participants reported that resistance to CC was encountered "sometimes" and "frequently," respectively [Figure 4].
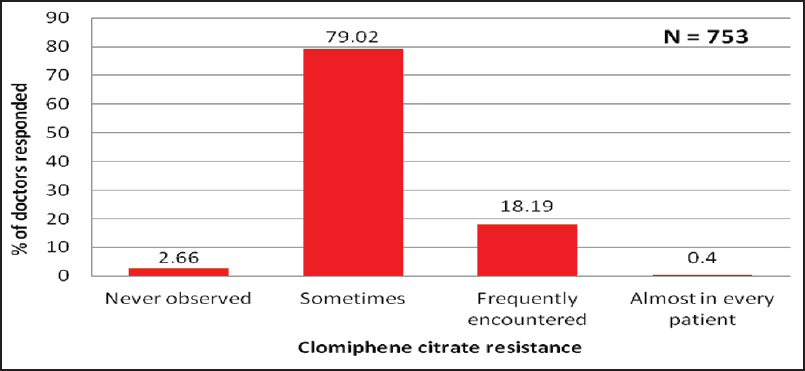
- Occurrence of CC resistance
Safety assessment of CC
Almost 45% of participants reported abdominal/pelvic discomfort or pain as a commonly encountered adverse effect, followed by 33% of participants reporting ovarian enlargement. Nausea and vomiting was reported by 29% of participants [Table 6].

Approximately 54%, 33%, and 16% of participants encountered multiple gestation, OHSS, and spontaneous abortion, respectively, as a frequent complication with CC [Table 7].

However, according to the vast majority of participants (91.28%), only less than 5% of patients developed OHSS with CC [Figure 5].

- Percentage of participants reporting development of OHSS with CC
As per the global assessment of tolerability, approximately 83% of participants felt that CC has very good to excellent tolerability [Figure 6].

- Global assessment of tolerability of CC
Interestingly, as many as 6.45% of participants reported that they had noticed congenital malformations in a child born after CC treatment [Figure 7].
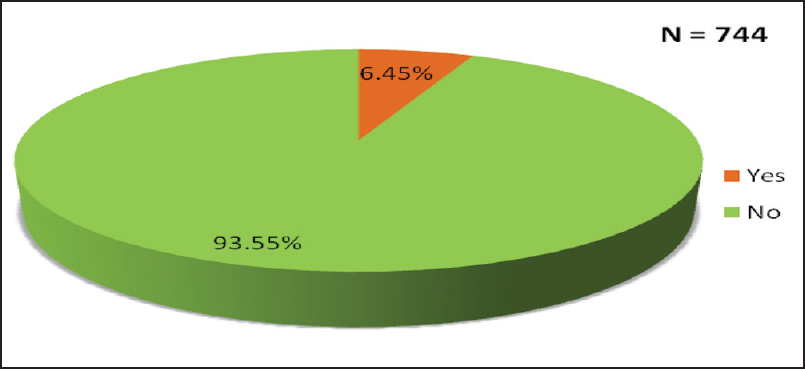
- Participants reporting congenital malformations with CC
Perception about CC
Many participants (62.48%) preferred a dose of 50 mg/day of CC for 5 days, whereas 42.48% of the participants preferred a dose of 100 mg/day for 5 days [Table 8].

According to almost 80% of participants, the preferred maximum duration of CC per cycle was 5 days [Figure 8].

- Preferred duration for CC
Around 53% of participants preferred day 2, whereas 42% preferred day 3 of the cycle to start CC therapy in patients with ovulatory dysfunction [Table 9].

Almost 38%, 24%, 23%, and 15% of participants considered a Graafian follicle size of 18 mm, 12 mm, 14 mm, and 16 mm respectively to anticipate ovulation/give an ovulatory trigger [Table 10].

The majority of participants (76.9%) usually prescribed additional drug(s) to improve endometrium, whereas the remaining 23.1% of participants did not prescribe any additional drug to improve endometrium [Figure 9].

- Participants prescribing additional drug(s) to improve endometrium
Almost 36% of participants preferred the sixth day and 30% of participants preferred the seventh day of the cycle to start estrogen in patients on CC therapy [Table 11].

In total, 85% of the participants advised natural conception as the most preferred method of conception to patients on CC [Figure 10].

- Preferred method of conception with CC
Almost 63% and 53% of participants preferred gonadotropins and metformin respectively as additional drug(s) for patients not responding to CC alone [Table 12].

DISCUSSION
CC is approved for induction of ovulation in patients with persistent ovulatory dysfunction.[3] This drug has been available in India since 1974.[6] This drug has a unique place in therapy and is used and misused very frequently in routine clinical practice. There are limited clinical data on CC in the real-life setting in India. Therefore, the present survey was taken to understand the current knowledge, attitude, and practice of Indian gynecologists related to CC. A KAP survey can be used to analyze the prescribing behavior of doctors.[7] For the purposes of this survey, "knowledge" means knowing about CC, "attitude" refers to the way gynecologists think or feel about CC, and "practice" means the usage pattern of CC in routine clinical practice. To the best of our knowledge, this was the only KAP survey made with the participation of Indian gynecologists.
The most preferred patient profile for CC was PCOS with ovulatory dysfunction, which is as per the reported literature.[1,3,4] Ovulation rate, i.e., the percentage of patients ovulating with each cycle of 50 mg CC was 21-60%, according to most participants. Endometrial thickness with CC was 7-10 mm, as observed by the majority of the participants. The pregnancy rate reported with each CC cycle was 11-30%.
The majority of participating doctors highlighted that anywhere between 3 and 6 cycles of CC were required for conception. According to most participants, CC alone is sufficient for the induction of ovulation in more than 50% of patients. CC resistance, which according to most participants was the failure to ovulate with a 150 mg dose for 3 cycles, was sometimes encountered. The overall global efficacy of CC was rated as very good to excellent.
Commonly observed adverse effects with CC were not serious and included abdominal/pelvic discomfort or pain, nausea, vomiting, hot flushes, and ovarian enlargement. According to most participants, multiple pregnancy and OHSS were frequently encountered complications with CC. Additionally, OHSS was reported in less than 5% of patients.
Overall, the global tolerability of CC was rated as very good to excellent. However, congenital malformations were reported in children born after CC therapy by quite a few participants.
Most of the participants usually preferred standard doses of CC, i.e., 50 mg/day or 100 mg/day prescribed for a maximum of 5 days per cycle starting usually on day 2 or day 3 of the cycle. Different participant doctors preferred different sizes of Graafian follicles, varying from 12 mm to 18 mm, for giving a trigger.
Additional drug(s) were needed to be prescribed to improve the endometrium, of which estrogen was usually started on day 6 or day 7 of the cycle. Metformin and gonadotropins were the most preferred drugs in patients not responding to CC. Most participants advised conception by natural methods and not by assisted reproductive techniques, in patients on CC therapy.
The present KAP survey was conducted across India and included a large number of experienced gynecologists responding to the questionnaire. A KAP survey, however, may have some obvious limitations: The multiple-choice format of the present survey questionnaire makes this survey closed-ended, thereby directing the participants to choose desirable answers. In spite of all these limitations, the present survey was an attempt to understand current knowledge, attitude, and practice among Indian gynecologists. This survey highlighted some interesting facts mentioned above in addition to known information. However, a systematic clinical trial may be further required to confirm these facts.
CONCLUSION
The present KAP survey highlighted that CC is a commonly used agent for ovulatory dysfunction, with or without other agents. On usage of CC, good ovulation and pregnancy rates were reported, with very good to excellent efficacy and tolerability. Resistance to CC was also reported in routine clinical practice.
Financial support and sponsorship
Unichem Laboratories Ltd. was involved in designing, expediting, and analyzing this study. No grant was given to any of the authors.
Conflicts of interest
The authors declare that they have no competing interests. Dr. Swami OC is a full-time employee of Unichem Laboratories Ltd., which actively markets CC.
Acknowledgment
The Indian Fertility Society gratefully acknowledges the assistance given by Unichem Laboratories Ltd. in designing, expediting, and analyzing this study. The authors gratefully acknowledge and thank the 771 gynecologists across India who participated in this survey.
REFERENCES
- Characteristics of infertile patients with ovulatory dysfunction and their relation to body mass index. J Ayub Med Coll Abbottabad. 2009;21:12-6.
- [Google Scholar]
- Letrozole or clomiphene citrate as first line for anovulatory infertility: A debate. Reprod Biol Endocrinol. 2011;9:86.
- [Google Scholar]
- Use of clomiphene citrate in infertile women: A committee opinion. Fertil Steril. 2013;100:341-8.
- [Google Scholar]
- Knowledge, attitude and practice (KAP) survey regarding the safe use of medicines in rural area of Gujarat. Adv Trop Med Pub Health Int. 2011;1:66-70.
- [Google Scholar]
- Approval Status of New Drug during 1971-1998. Available from: http://cdsco.nic.in/writereaddata/1971-98.
- Antibiotic prescribing in DR Congo: A knowledge, attitude and practice survey among medical doctors and students. PLoS One. 2013;8:e55495.
- [Google Scholar]







