Translate this page into:
Comparison of pregnancy outcomes in women undergoing frozen thawed embryo transfer (FET) cycles following ultrasound for endometrial morphology with and without Doppler studies- a prospective cohort study
Address for correspondence: Dr. Vasudha Gupta MBBS, MS (obstetrics and gynecology), DNB, IFS Diploma in clinical ART, Centre of IVF and Human Reproduction, Sir Gangaram Hospital, F-438, 3rd floor, New Rajendra Nagar, New Delhi 110060, India. E-mail: vasudhamamc@gmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
There is a paucity of data evaluating role of endometrial blood flow in frozen thawed embryo transfer cycles (FET cycles) in hormone replacement treatment (HRT) cycles.
Objective:
To compare pregnancy outcomes in women undergoing ultrasound for endometrial morphology alone to those with endometrial morphology with blood flows in frozen embryo transfer cycles.
Patients:
Patients aged 23 to 38 years undergoing first two frozen thawed single blastocyst embryo transfer cycles. From August 2019 to January 2020, 163 patients undergoing hormone replacement frozen embryo transfer cycles were enrolled in the study. Patients were divided in two groups. Patients in group A (n = 92) had ultrasonographic evaluation of endometrial thickness and morphology and in group B (n = 71) patients underwent ultrasound for endometrial thickness, morphology along with Doppler blood flow studies.
Outcome measures:
Primary outcome was clinical pregnancy rate. Secondary outcome measures were pregnancy loss rate, ongoing pregnancy rate, and ectopic pregnancy rate.
Results:
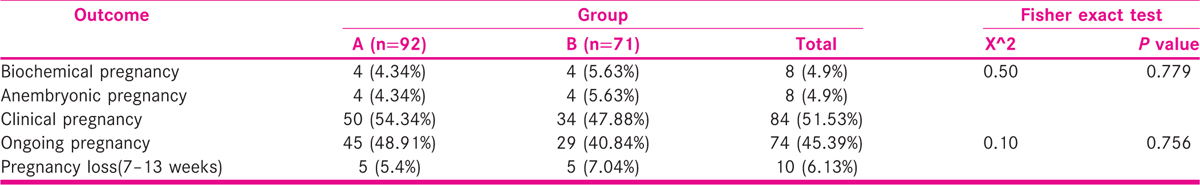
Clinical pregnancy rate in group A and group B was 54.34% and 47.88%. Clinical pregnancy rate was similar between both the groups (P = 0.779). Ongoing pregnancy rate in group A and B was 48.91% and 40.84%, respectively. Pregnancy loss rate (7–13 wks) was 5.4% and 7.04% in group A and group B, respectively. There was no significant difference in ongoing pregnancy rate and pregnancy loss rate between both the groups (P = 0.756).
Conclusion:
Additional measurement of doppler studies do not help in improving implantation and thus seems unnecessary in improving pregnancy rates and reducing pregnancy loss rates in FET cycles.
Keywords
frozen thawed embryo transfer
doppler blood flow studies
endometrial receptivity
clinical pregnancy rate
INTRODUCTION
Infertility varies across different areas of the world and affect around 15% of couples globally.[1]. Implantation is a unique and complicated phenomenon involving apposition and adhesion of a normal euploid blastocyst to a receptive uterine endometrium followed by invasion of trophoblasts between its epithelial cells. Uterine lining is most receptive to embryo during the mid-secretory phase of menstrual cycle which corresponds to 19th to 23rd day of menstrual cycle, also referred to as window of implantation (WOI).[2,3]
Methods for assessing endometrial receptivity are endometrial biopsy, hormonal and ultrasonographic evaluation.[4]. Standard ultrasound markers indicating good endometrial receptivity are endometrial thickness and morphology.[5]. An endometrial thickness of more than or equal to 7 mm along with trilaminar pattern is a universally accepted indicator of adequate implantation. Various studies have been done to evaluate the relationship between endometrial blood flow and clinical pregnancy rates in fresh embryo transfer cycles[6,7,8,9,10,11] but there are only few studies evaluating role of endometrial blood flow in frozen thawed embryo transfer cycles (FET cycles) in hormone replacement treatment (HRT) cycles.
Thus, present study was being planned to analyze the importance of performing endometrial and subendometrial blood flows in addition to measuring endometrial thickness and morphology helping to predict pregnancy outcomes in FET cycles.
AIM AND OBJECTIVES
To compare pregnancy outcomes in women undergoing ultrasound for endometrial morphology alone to those with endometrial morphology with endometrial blood flows in FET cycles.
MATERIALS AND METHODS
It was a prospective cohort study conducted between August 2019 to January 2020 at tertiary care IVF center, New Delhi. We expected to recruit minimum 20 patients per month in a duration of 6 months. Therefore, we thought it would be possible to study 120 patients (60 patients in each arm) due to time constraints and application of strict inclusion and exclusion criteria. All patients underwent ovarian stimulation with recombinant gonadotropins with antagonist or long-agonist protocol. Ovum pick up was done after 36 hours of human chorionic gonadotropin (hCG)/agonist trigger. Fertilization of oocytes was done either by IVF or ICSI procedure. Embryos formed were cultured till blastocyst stage. Cryopreservation was undertaken in all patients for various indications using the process of vitrification following standard protocol provided by the manufacturer.
Consent
Clearance from the Indian Fertility Society (IFS) ethical committee was obtained (F.1/IEC/IFS/2020No.39) and a written informed consent in English/Hindi was taken from all the participants of the study
Inclusion criteria
Age 23 to 38 years
Women undergoing first two FET cycles (HRT cycles)
Single embryo transfer of day 5/6 blastocyst
Exclusion criteria
Severe endometriosis
Intramural, submucous fibroids distorting the cavity
Untreated hydrosalpinx
Endometrial thickness < 6 mm on day of progesterone start.
Blood flows in zone 1 and 2
Methodology
All patients were recruited on day 2/3 of the cycle after taking written informed consent. A detailed history was taken. Ultrasonography was performed for baseline endometrial thickness and blood was sent for serum estradiol and progesterone estimation. Estradiol valerate 6 to 8 mg daily divided dose was started for endometrial preparation and maximum dose of 12 mg was given. Serial ultrasonographic examinations were performed starting from day 10 of HRT till endometrium reached thickness of 6 mm and above. Patients were divided in two groups. In group A, ultrasound was done on day 10 of HRT for endometrial thickness and morphology assessment and was repeated every 3 to 5 days till endometrial thickness of > 6 mm with trilaminar pattern was achieved. In group B patients underwent ultrasound for endometrial thickness, morphology along with Doppler blood flow studies starting from day 10 of HRT and repeated every 3 to 5 days till endometrial thickness > 6 mm with trilaminar pattern along with Doppler endometrial and subendometrial blood flows were present in zone 3 or 4. In group A progesterone supplementation through vaginal route was started when endometrial thickness (ET) ≥ 6 mm with trilaminar pattern and embryo transfer was performed after 5 days of progesterone start. In group B, progesterone was added followed by embryo transfer 5 days later when ET > 6 mm along with doppler endometrial and subendometrial blood flows were present in zone 3 or 4.
Methodology of USG
Baseline pelvic scan for evaluation of uterus and ovaries were performed by B mode. All the transvaginal ultrasound scans were performed with the digital platform Voluson E8 system. Visualization of both uterus and ovaries was initially performed using B mode. When a longitudinal view of the uterus was obtained, endometrium was assessed measuring from outside to inside at its thickest point. Then 2D-power doppler assessment was performed. Same power doppler characteristics were applied for all ultrasounds in all patients: Normal color quality was used with color gain of 3.4. Pulse repetition frequency of 600 Hz and wall motion filter of 50 Hz was applied.
Applebaum criteria was followed for visualizing zones of endometrial blood flow.[12]
Zone 1- vessels penetrating the outer 2 mm hypoechogenic area surrounding the endometrium
Zone 2- Vessels penetrating the hyperechogenic outer margin of the endometrium
Zone 3- Vessels entering the hypoechogenic inner area
Zone 4- Vessels entering the hyperechogenic cavity.
Embryo transfer procedure
Thawing of vitrified embryos was performed using standard protocol provided by manufacturer on the planned embryo transfer day. Embryo transfer procedure was executed according to the standard hospital protocol.
Luteal phase support
Standard luteal phase support was given in form of vaginal progesterone in a divided daily dose of 800 mg. Serum β hCG test was done on day 11 of embryo transfer. Both estradiol and progesterone were continued till 11 weeks of gestation along with tablet folic acid.
A value Serum β hCG >25 IU was taken as positive. Ultrasonography for cardiac activity was done at 7 weeks period of gestation (POG) and if cardiac activity was present, clinical pregnancy was confirmed. Ongoing pregnancy was defined as pregnancy beyond 13 weeks period of gestation. Positive β hCG rate was calculated as the ratio of patients having positive β hCG to number of FET. Clinical pregnancy rate was calculated as the ratio of number of clinical pregnancies upon number of embryo transfers. Ongoing pregnancy rate was calculated as a ratio of ongoing pregnancies beyond 13 weeks to the number of embryo transfers.
Statistical analysis
Data was analyzed using software system statistical package for social sciences (SPSS) version 20 (IBM Corp. Released 2011; IBM SPSS Statistics for Windows, Version 20.0, Armonk, NY: IBM Corp.). Independent t test and Wilcoxon test was used for continuous variables. Chi square and fisher exact test was used for categorical variables. P value < 0.05 was considered significant.
RESULTS
A total of 163 patients undergoing hormone replacement FET cycles were enrolled in the study. Patients were divided in two groups. Patients in group A (n=92) had ultrasonographic evaluation of endometrial thickness and morphology and in group B (n=71) patients underwent ultrasound for endometrial thickness, morphology along with doppler blood flow studies. No patients were lost to follow up. Flow diagram is shown in Figure 1.

- Flow diagram of the study
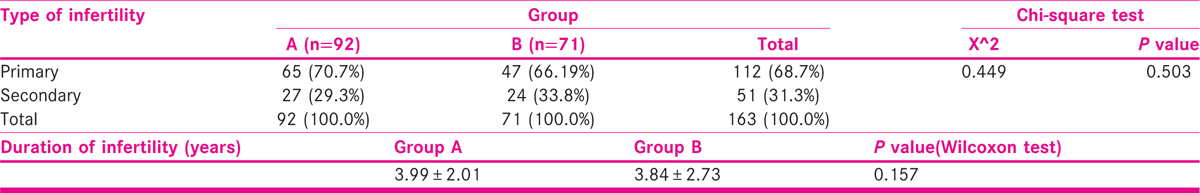
There was no significant difference between both the groups in terms of type and duration of infertility (P = 0.503, P = 0.157) as shown in Tables 2 and 3.
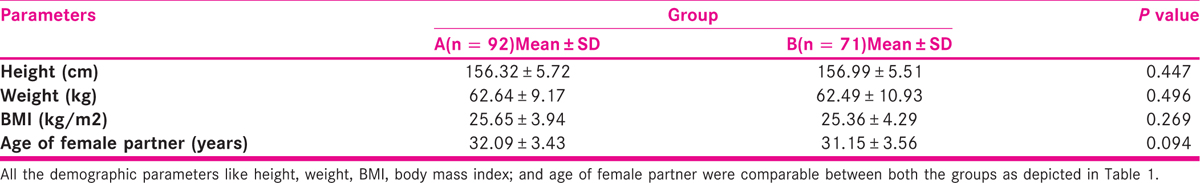
Participants in the group A had the larger proportion of first cycle (87%). Participants in the group B had slightly higher proportion of patients undergoing second cycle (25.4%). There was a significant difference between the two groups in terms of distribution of first and second FET cycle (P = 0.044). There was no significant difference between the two groups in terms of indication of IVF, distribution of semen parameters, distribution of indication of freezing, stage of blastocyst (P = 0.083, P = 0.464, P =0.723, P = 0.367). 89.1% and 91.5% embryos were of good quality in group A and group B, respectively. There was no significant difference between the two groups in terms of quality of embryo (P = 0.166).
The mean endometrial thickness in Group A group was 8.55 ± 1.27 mm. Mean endometrial thickness in Group B was 8.90 ± 1.35 mm. There was no significant difference between both the groups in terms of endometrial thickness (P = 0.090). Doppler blood flows were performed in group B only. 76.1% of the participants in the group B had blood flows in zone 3. 23.9% of the participants had blood flows in zone 4.
Biochemical, anembryonic, and clinical pregnancies were similar between both the groups (P = 0.779). There was no case of ectopic pregnancy in both the groups. Similarly, there was no significant difference in ongoing pregnancy rate and pregnancy loss rate between both the groups (P = 0.756) as shown in table 3 and Figure 2].
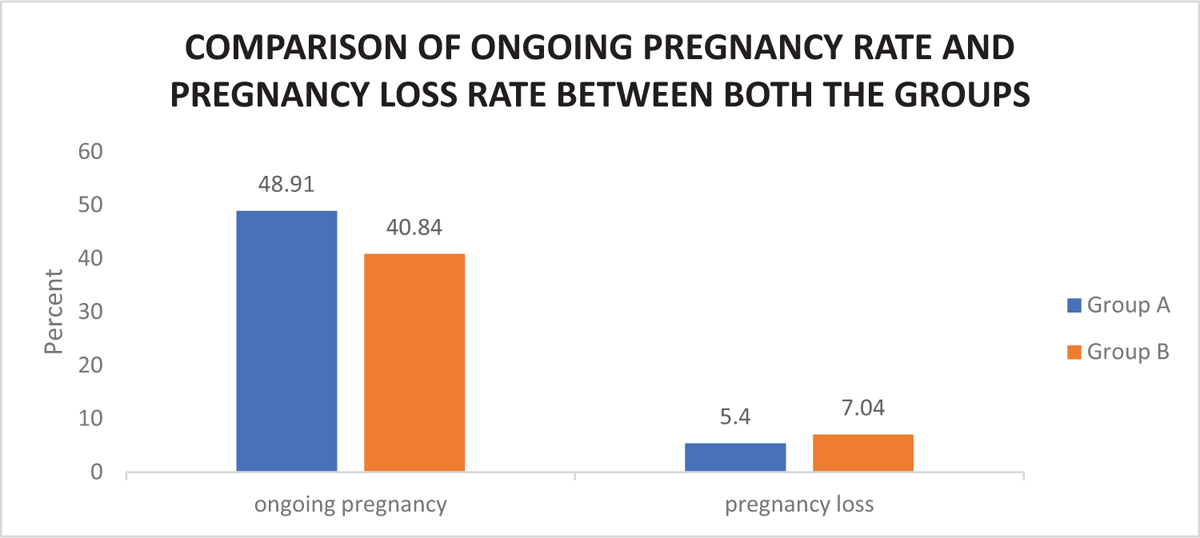
- Bar diagram showing comparison of ongoing pregnancy rate and pregnancy loss rate in both the groups.
A subgroup analysis was done to find the distribution of first or second FET cycle in pregnant and non-pregnant patients of Group A and group B. In group A, 55% patients who underwent first cycle FET got pregnant and 50% patients with second cycle FET got pregnant with no statistical difference in pregnancy rates (P =0.746). In group B, 50.9% patients who underwent first cycle FET got pregnant and 38.9% patients who underwent second cycle got pregnant again with no statistical difference in pregnancy rates in both cycles in this group also (P = 0.376). This analysis was done to remove the bias generated by difference between the two groups in terms of distribution of first and second FET cycle.
In group A, the conception rate was similar across all endometrial thicknesses. There was no difference between pregnant and non-pregnant women in terms of range of endometrial thickness in group A, group B and in whole study cohort (P = 0.939, 0.251, 0.466).
DISCUSSION
Various studies have been performed in past to find out methods for improving pregnancy rates during fresh and FET. Ultrasonographic examination of the endometrial lining has been the only criteria since the beginning on which the decision for embryo transfer is taken. However, in the recent past along with real time ultrasonography of the endometrium, doppler blood flow studies to the endometrial lining, prior to either fresh or frozen embryo transfer has gained importance as an additional measure for assessing endometrial receptivity and improving pregnancy outcomes. Hence, the present study was planned to seek an answer to the particularly important question of, whether the evaluation of this additional parameter of doppler blood flows to the regular real time ultrasonography, benefits the patients undergoing FET cycles.
Bias due to demographic characteristics were taken care of in the present study. Various confounding which could have biased the pregnancy outcomes like age, body mass index (BMI), duration of infertility, stage of blastocyst transfer, number of embryos transferred, and quality of embryos were taken into consideration in the present study.
In the present study we included women undergoing HRT cycles only. Ng EH et al. and Zackova T et al.[13,14] studied frozen embryo transfer in natural and clomiphene induced cycles. Like present study, HRT cycles were included in various studies.[15,16,17,18]. The idea behind recruiting only HRT cycles in the present study was to analyze a consistent study cohort where pituitary downregulation was achieved by use of high dose of estrogens right from the beginning of the cycle, which meant hormone replacement started from day two or three of starting menstruation. For the same reason women who underwent only single blastocyst transfer were included in the study. In other studies, minimum two cleavage stage embryos were transferred in the endometrial cavity. Patients who made only a single embryo were not included in assessment to remove bias of FET from a possibly compromised embryo. Patients who had minimum of two blastocysts were assessed and only FET is first two cycles were considered for evaluation so that cases of recurrent implantation failures could be minimized in both groups.
Studies, which were done in past comparing doppler studies to pregnancy outcomes had a different methodology compared to our study. In majority studies different doppler parameters were assessed in all patients undergoing FET and then patients were divided into two groups whether they got pregnant or not. Doppler parameters were then compared between these two groups.[13,14,16]. However, observational study by Deepika K and Sardana D et al., divided patients into two groups based on doppler studies. Group A comprised of 127 women in whom blood flows were observed in at least sub endometrial region and group B had 38 patients in whom blood flow was not present in sub endometrial region. Out of 127 women of group A, 19 women had blood flows in zone 1, 37 in zone 2, 71 in zone 3 and 4. After this they compared pregnancy rates and implantation rates among groups.[15,17] In the present study we compared pregnancy rates between women undergoing FET cycles with and without Doppler flow studies. In group A Doppler blood flows were not performed and we assumed that it could be in any zone which is unknown to the clinician. The rationale behind this is that there is a tendency of clinicians to cancel FET cycles when blood flows remained in zone 1 and 2 even after appropriate dose administration of estradiol valerate along with optimum endometrial thickness and trilaminar pattern on ultrasonographic examination and we could never get to know the fate of these cycles. So, to remove that bias, Doppler blood flows were not performed in group A and embryo transfer was solely guided by endometrial thickness and trilaminar pattern.
Clinical pregnancy rate in group A and group B was 54.34% and 47.88%, respectively. Biochemical, anembryonic and clinical pregnancy rates were also similar between both the groups (P = 0.779). Ongoing pregnancy rate in group A and B was 48.91% and 40.84%, respectively. There was no significant difference in ongoing pregnancy rate and pregnancy loss rate between both the groups (p=0.756). Therefore, it appears from our observations that doppler blood flows did not provide an additional benefit in predicting clinical pregnancies and pregnancy loss rate. Further analyzing clinical pregnancy rates in women undergoing FET in group B with sub-endometrial blood flow in zone 3 and zone 4 was 44.44% and 58.82%, respectively. Clinical pregnancies were also similar while comparing both subgroups within group B with subendometrial blood flow to either zones 3 or 4 (P = 0.449).
There was no difference between pregnant and nonpregnant woman in terms of range of endometrial thickness. Through present study we can conclude that optimal endometrial thickness for embryo transfer is 6 to 12 mm as there was no significant difference in pregnancy rates across all ranges of endometrial thickness studied.
There is a paucity of data analyzing role of doppler flow studies in FET cycles. All these studies differed from each other greatly in their study population, methodology, FET protocol used, stage of embryo transferred, day of ultrasound assessment. Mishra VV et al. concluded that endometrial and sub endometrial blood flows assessed by 3D power doppler were useful indicator for predicting pregnancy outcomes in FET cycles.[18] Deepika K et al. and Sardana D et al.[15,17] concluded that there was a positive correlation between presence of blood flows in endometrial and subendometrial region and pregnancy outcomes. A meta-analysis was conducted by Wang J et al.[4] and they concluded that the doppler studies could help to identify appropriate timing for FET cycles. All these results were contrary to the present study. Ng EH et al.[13] concluded that endometrial vascularity if assessed at one point in the preprogesterone stage does not give any added benefit in predicting pregnancy. Zackova T et al.[14] concluded that triple line pattern of endometrium was the most important sign that had a positive correlation with pregnancy outcome. Doppler blood flows and blood tests were not of any additional benefit. Similarly, Nandi A et al.[16] concluded that 3DPD angiography is not a sensitive tool to predict the outcome of FET. Results of these studies were consistent with the present study. Hence, there are conflicting results on the doppler blood flow studies on endometrium and subendometrium in predicting pregnancy outcomes in FET cycles. To the best of our knowledge, this is the first Indian study comparing pregnancy outcomes between women undergoing ultrasound for endometrial morphology alone to those with endometrial morphology with endometrial blood flows before FET cycles. Strengths of the study were that it was a prospective cohort study which included elective single blastocyst transfers with a reasonable sample size. Limitations of the study were that in group B where we performed doppler blood flow studies we did not include patients with blood flows in zone 1 and 2 as they were excluded by the clinicians and randomization was not done in the study. Doppler blood flow assessment was done using Applebaum criteria of zone of blood flows which is a subjective assessment. Further studies are recommended evaluating role of endometrial blood flows on endometrial receptivity and pregnancy outcomes in FET cycles on a larger sample size in a multicentric design.
CONCLUSION
Endometrial thickness and pattern are stand-alone good indicators in timing embryo transfer. Through the present study we conclude that additional measurement of doppler studies do not help in improving implantation and thus seems unnecessary in improving pregnancy rates and reducing pregnancy loss rates in frozen thawed embryo transfer cycles.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- A unique view on male infertility around the globe. Reprod Biol Endocrinol. 2015;13:37.
- [Google Scholar]
- Endometrial receptivity markers, the journey to successful embryo implantation. Hum Reprod Update. 2006;12(6):731-46.
- [Google Scholar]
- Embryonic implantation: cytokines, adhesion molecules, and immune cells in establishing an implantation environment. J Leukoc Biol. 2009;85(1):4-19.
- [Google Scholar]
- Association between endometrial/subendometrial vasculature and embryo transfer outcome: a meta-analysis and subgroup analysis. J Ultrasound Med. 2018;37(1):149-63.
- [Google Scholar]
- The role of ultrasonography in the evaluation of endometrial receptivity following assisted reproductive treatments: a critical review. Hum Reprod Update. 1996;2:323-35.
- [Google Scholar]
- Are endometrial parameters by three-dimensional ultrasound and power Doppler angiography related to in vitro fertilization/embryo transfer outcome? Fertil Steril. 2008;89:111-7.
- [Google Scholar]
- Assessment of uterine receptivity by the endometrial-subendometrial blood flow distribution pattern in women undergoing in vitro fertilization-embryo transfer. Fertil Steril. 2002;78:245-51.
- [Google Scholar]
- Endometrial thickness, morphology, vascular penetration and velocimetry in predicting implantation in an in vitro fertilization program. Ultrasound Obstet Gynecol. 1995;6:191-8.
- [Google Scholar]
- Endometrial vascularity and ongoing pregnancy after IVF. Eur J Obstet Gynecol Reprod Biol. 2002;104:137-43.
- [Google Scholar]
- Blood flow changes in uterine and ovarian vasculature, and predictive value of transvaginal pulsed colour Doppler ultrasonography in an in-vitro fertilization programme. Hum Reprod. 1995;10:688-93.
- [Google Scholar]
- Uterine vascularity during stimulation and its correlation with implantation in in-vitro fertilization. Hum Reprod. 1995;10:1497-501.
- [Google Scholar]
- The role of endometrial and sub endometrial vascularity measured by three-dimensional power Doppler ultrasound in the prediction of pregnancy during frozen-thawed embryo transfer cycles. Hum Reprod. 2006;21(6):1612-7.
- [Google Scholar]
- Assessment of endometrial and ovarian characteristics using three dimensional power Doppler ultrasound to predict response in frozen embryo transfer cycles. Reprod Biol Endocrinol. 2009;7:151.
- [Google Scholar]
- Correlation of sub endometrial-endometrial blood flow assessment by two-dimensional power Doppler with pregnancy outcome in frozen-thawed embryo transfer cycles. J Hum Reprod Sci. 2014;7(2):130-5.
- [Google Scholar]
- Assessment of endometrial and subendometrial blood flow in women undergoing frozen embryo transfer cycles. Reprod Biomed Online. 2014;28(3):343-51.
- [Google Scholar]
- Assessment of uterine receptivity by the subendometrial endometrial blood flow distribution pattern in frozen thawed embryo transfer cycles. Int J infertil Fetal Med. 2015;6(1):35-9.
- [Google Scholar]
- Endometrial and subendometrial vascularity by three-dimensional (3D) power doppler and its correlation with pregnancy outcome in frozen embryo transfer (FET) cycles. J Obstet Gynaecol India. 2016;66(suppl 1):521-7.
- [Google Scholar]







