Translate this page into:
Dilemmas in ART – Looking for solutions
Address for correspondence: Dr. Kuldeep Jain, Editor-in-Chief, Fertility Science and Research, 23-24, Gagan Vihar, Main Road (Near Karkardooma Flyover), Delhi 110051, India E-mail: jainravi6@rediffmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Though the assisted reproductive technology (ART) has given hope to a large number of couples suffering from infertility, it has also hosted innumerable technical, ethical, legal, and social challenges for the future.
Advancements in the field have resulted in a landmark shift in the way physicians and the general population perceive infertility and related issues. The reproductive science is unswervingly challenging the society to re-evaluate the way in which human life, social justice, and claims to resulting genetic offspring are viewed. These issues will challenge the technology and legal organizations to modify existing laws to accommodate its unique situations.
We also need to devote resources and energies to identify and remove the environmental and physical causes of infertility. Prevention, education, and increased access to appropriate and cost-effective fertility care, including insurance coverage, are also imperative so that more families throughout the world are able to have children when they are ready safely.
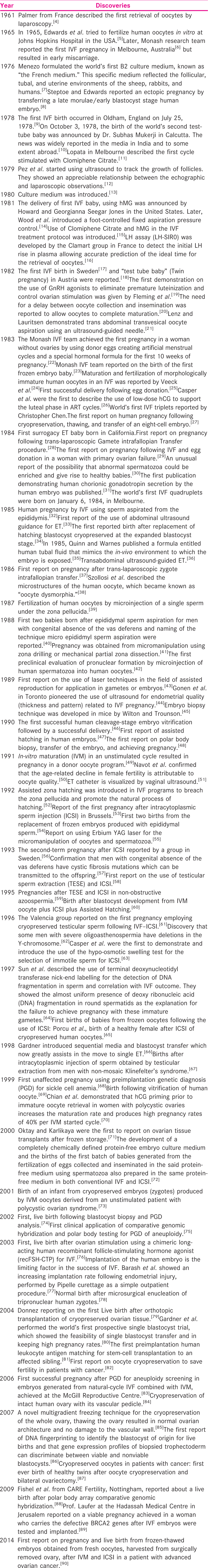
HISTORY AND EVOLUTION OF IN-VITRO FERTILIZATION GLOBALLY
The beginning
The history of in-vitro fertilization (IVF) and embryo transfer (ET) dates back as early as the 1890s when Walter Heape, a professor, and physician at the University of Cambridge, England, who had been conducting research on reproduction in a number of animal species, reported the first known case of embryo transplantation in rabbits, long before the applications to human fertility were even suggested.
In 1934, Pincus and Enzmann,[1] from the Laboratory of General Physiology at Harvard University, published a paper in the Proceedings of the National Academy of Sciences of the USA, raising the possibility that mammalian eggs can undergo normal development in vitro. Fourteen years later, in 1948, Miriam Menken and John Rock[2] retrieved more than 800 oocytes from women during operations for various conditions. One hundred and thirty-eight of these oocytes were exposed to spermatozoa in vitro. In 1948, they published their experiences in the American Journal of Obstetrics and Gynaecology.
However, it was not until 1959 that the indisputable evidence of IVF was obtained by Chang[3] who was the first to achieve births in a mammal (a rabbit) by IVF. The newly ovulated eggs were fertilized, in vitro by incubation with capacitated sperm in a small Carrel flask for 4 h, thus opening the way to assisted procreation.
Professionals in the fields of microscopy, embryology, and anatomy laid the foundations for future achievements. The recent rapid growth of IVF–ET and related techniques worldwide are further supported by the social and scientific climate which favors their continuation.
Through the years, numerous modifications have been made in the development of IVF–ET in humans: refinement of fertilization and embryo culture media; earlier transfer of the embryo; improvements in equipment; use of a reduced number of spermatozoa in the fertilization dish, embryo biopsy among others.
The purpose of this introduction is to acknowledge those who initiated new steps in the development of the treatment protocols and techniques that we now use facilitating such simple and promising IVF–ET procedures.
Evolving assisted reproductive technology in modern era
In 1978, the world witnessed the birth of the first “test tube baby.”[9] Since then, there have been explosive advances in ARTs. Current optimizations surrounding the delivery of IVF including the utilization of minimal stimulation protocols and gonadotropin-releasing hormone (GnRH) agonist cycle triggers are being increasingly utilized to maximize patient safety. Modifications, such as IVM and cryopreservation seen in the embryology laboratory, continue to improve pregnancy rates. Concurrent with these advancements in IVF has been the emergence of related technologies, such as embryonic genetic diagnostic and screening and oocyte freezing, which potentially has broad applications for both fertile and infertile couples. Another technology such as time-lapse imaging may be a powerful tool to select embryos best suited for uterine transfer in IVF cycles. As these relevant applications of ART become increasingly utilized, it is incumbent on the society to ensure that these resources are made available in a morally responsible and equitable manner.
Many aspects of clinical practice in ART raise challenging issues, controversies, and dilemmas for service providers:
(1) Surrogacy: Central concern surrounding the use of surrogates and gestational carriers is the possibility that financial pressures could lead to the exploitation and commercialization of the service.[91] Additionally, the rights of the surrogate or gestational carrier to not relinquish the infant after delivery are not well described.[92]
At present, issues surrounding the individual rights, exploitation, and citizenship of the resulting offspring of international gestational carriers are largely unresolved internationally.[93] The proposed Indian Surrogacy (Regulation) Bill, 2016, inter alia, provides) to allow ethical altruistic surrogacy to the intending infertile Indian married couple only between the age of 23–50 years and 26–55 years for female and male respectively; (c) the intending couples should be legally married for at least five years and should be Indian citizens to undertake surrogacy or surrogacy procedures and prohibits surrogacy for international patients and commercial surrogacy.[94]
One need to debate keeping the individual need of infertile couple who do not have an option other than surrogacy and do not have one in family, whether banning the commercial surrogacy is justified or it requires a regulation.
(2) Donor conception: It would be a challenging issue in coming decades. With growing information and technology, the clientele may not agree for donor cycles. Stimulation protocols and stem cells would play an important role.
(3) PGD: In the near future, with refinements in microarray technology and the definition of genetic sequences associated with certain physical characteristics, it is conceivable that specific physical or mental characteristics may be evaluated to guide the decision as to which embryos to transfer.[95]
(4) Cryofrozen embryos: Embryo freezing is a robust and routine part of the IVF process, and approximately 60% of patients end up with some embryos in storage. This process provides patients with a “back-up” in case the initial fresh ET does not result in a pregnancy and if patients come back after few years to have a second child. Cryofrozen embryos of patients with single child norms would flood our cryobiology laboratories with challenges in disposing them.
However, the legal issues of whether an unborn is entitled to any rights, and if so what they are, have appeared in several different areas of law and need to be resolved.[96]
(5) Fertility preservation: Fertility preservation for patients with cancer using IVM, oocyte Vitrification, and the freezing of intact human ovaries with their vascular pedicles have also been reported.[97] However, this technology at present, in many countries, is only available to those with financial means. This poses ethical and social issues that will certainly see more attention in the future.
(6) Deteriorating male factor: Deteriorating male factor is the reduction of normal sperm count, motility, and morphology, and this increase in the deterioration of male factor and fertility fecundity has been a concern for ages. Various lifestyle factors such as tobacco smoking, chewing, and alcohol use as well as exposure to toxic agents might be attributed to the risk of declining semen quality and increase in oxidative stress and sperm DNA damage.[98] To achieve an acceptable pregnancy rate in such cases, ISCI is the only option. This could be a big challenge in the countries which do not believe in sperm donation. Stem cell biology would play a major role in such cases.
(7) Posthumous use of gametes: Posthumous use of gametes occurs when the surviving partner of a person dying on a battlefield or due to other reasons wishes to obtain and use their gametes (sperm) to conceive a child to continue his lineage. It is not permitted in most of the countries. It is important to refer to the law in each state/territory, and/or National Health and Medical Research Council, to determine whether the removal and or use of gametes after a person dies is permissible, and if so the circumstances in which this may occur because posthumous use of gametes can pose legal issues such as legitimacy of child born, inheritance rights of a child, and lifelong psychosocial implications.[99]
(8) Legal issues: Because of the rapidly evolving nature of the ART, legislation is often unable to keep pace and address all of the ethical and legal issues that are constantly emerging in the field. It is therefore incumbent upon physicians to continually monitor these issues and ensure that ART technologies are offered and delivered in a manner that balances patient care with social and moral responsibility.
CONCLUSION
ART as is a field that is dynamic and ever-changing. As technologies continue to proliferate, ethical and social challenges multiply, with complex questions of justice, rights, and conflicting principles continually rising. As an evolving society, we are long overdue to discuss these issues and to guard against leaving them solely in the province of researchers and reproductive medicine specialist.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Can mammalian eggs undergo normal development in vitro? Proc Natl Acad Sci USA. 1934;20:121-2.
- [Google Scholar]
- In vitro fertilization and cleavage of human ovarian eggs. Am J Obstet Gynecol. 1948;55:440-52.
- [Google Scholar]
- Nezhat’s History of Endoscopy. Society of Laparoscopic Surgeons; 1940. [Chapter 17]. Retrieved January 1, 2016.
- Preliminary attempts to fertilize human oocytes matured in vitro. Am J Obstet Gynecol. 1966;96:192-200.
- [Google Scholar]
- Synthetic medium for gamete survival and maturation and for the culture of fertilized eggs. C R Acad Sci Hebd Seances Acad Sci D. 1976;282:1967-70.
- [Google Scholar]
- Reimplantation of a human embryo with subsequent tubal pregnancy. Lancet. 1976;1:880-2.
- [Google Scholar]
- Architect of India’s first test tube baby: Dr Subhas Mukerji, 16 January 1931 to 19 July 1981. Curr Sci. 1997;72:526-31.
- [Google Scholar]
- Pregnancy following intrauterine implantation of an embryo obtained by in vitro fertilization of a preovulatory egg. Fertil Steril. 1980;33:117-20.
- [Google Scholar]
- Recherche d’une concordance entre l’échographie et l’observation par coelioscopie des follicules stimulés par les inducteurs de l’ovulation. 178 soireé gynéco-obstricale de St Maurice le 9.10.79. Milupa. Bagnolet
- The use of fluorescein diacetate to assess embryo viability in the mouse. J Reprod Fertil. 1980;58:189-96.
- [Google Scholar]
- Technique for collecting mature human oocytes for in vitro fertilization. Br J Obstet Gynaecol. 1981;88:756-60.
- [Google Scholar]
- Pregnancies in humans by fertilization in vitro and embryo transfer in the controlled ovulatory cycle. Science. 1981;212:681-2.
- [Google Scholar]
- Interpretation of plasma luteinizing hormone assay for the collection of mature oocytes from women: Definition of a luteinizing hormone surge-initiating rise. Fertil Steril. 1981;36:50-4.
- [Google Scholar]
- Methods for aspiration of human oocytes by various techniques. Acta Med Rom. 1982;20:370-8.
- [Google Scholar]
- Twin pregnancy after laparoscopic oocyte recovery, in-vitro fertilization and embryo transfer. [Author’s transl.] Geburtshilfe Frauenheilkd. 1982;42:197-9.
- [Google Scholar]
- A new systematic treatment for infertile women with abnormal hormone profiles. Br J Obstet Gynaecol. 1982;89:80-3.
- [Google Scholar]
- Effect of delayed insemination on in-vitro fertilization, culture, and transfer of human embryos. J Reprod Fertil. 1982;64:285-94.
- [Google Scholar]
- Ultrasonically guided percutaneous aspiration of human follicles under local anesthesia: A new method of collecting oocytes for in vitro fertilization. Fertil Steril. 1982;38:673-7.
- [Google Scholar]
- Pregnancy established in an infertile patient after transfer of a donated embryo fertilized in vitro. Br Med J (Clin Res Ed). 1983;286:835-8.
- [Google Scholar]
- Human pregnancy following cryopreservation thawing and transfer of an eight-cell embryo. Nature. 1983;305:707-9.
- [Google Scholar]
- Maturation and fertilization of morphologically immature human oocytes in a program of in vitro fertilization. Fertil Steril. 1983;39:594-602.
- [Google Scholar]
- Non-surgical transfer of in vivo fertilized donated ova to five infertile women: Report of two pregnancies. Lancet. 1983;2:223-4.
- [Google Scholar]
- Enhancement of human implantation by exogenous chorionic gonadotropin. Lancet. 1983;2:1191.
- [Google Scholar]
- Human pregnancy following cryopreservation, thawing, and transfer of an eight-cell embryo. Nature. 1983;305:707-9.
- [Google Scholar]
- Pregnancy after translaparoscopic gamete intrafallopian transfer. Lancet. 1984;2:1034-5.
- [Google Scholar]
- The establishment and maintenance of pregnancy using in vitro fertilization and embryo donation in a patient with primary ovarian failure. Nature. 1984;307:174-5.
- [Google Scholar]
- Male infertility successfully treated by in-vitro fertilization. Lancet. 1984;1:1239-40.
- [Google Scholar]
- Human chorionic gonadotropin secreted by preimplantation embryos cultured in vitro. Science. 1984;223:816-8.
- [Google Scholar]
- Human pregnancy by in vitro fertilization (IVF) using sperm aspirated from the epididymis. J In Vitro Fert Embryo Transf. 1985;2:119-22.
- [Google Scholar]
- Birth after replacement of hatching blastocyst cryopreserved at the expanded blastocyst stage. Lancet. 1985;1:647.
- [Google Scholar]
- Improved pregnancy rate in human in vitro fertilization with the use of a medium based on the composition of human tubal fluid. Fertil Steril. 1985;44:493-8.
- [Google Scholar]
- Pregnancy after translaparoscopic zygote intrafallopian transfer in a patient with sperm antibodies. Lancet. 1986;1:1329.
- [Google Scholar]
- Ultrastructure of the human preovulatory oocyte. J In Vitro Fert Embryo Transf. 1986;3:232-42.
- [Google Scholar]
- Fertilization of human oocytes by microinjection of a single spermatozoon under the zona pellucida. Fertil Steril. 1987;48:637-42.
- [Google Scholar]
- Two births after microsurgical sperm aspiration in congenital absence of vas deferens. Lancet. 1988;2:1364.
- [Google Scholar]
- Implantation of embryos after partial opening of oocyte zona pellucida to facilitate sperm penetration. Lancet. 1988;2:162.
- [Google Scholar]
- A preclinical evaluation of pronuclear formation by microinjection of human spermatozoa into human oocytes. Fertil Steril. 1988;49:835-42.
- [Google Scholar]
- Micromanipulation of sperm by a laser generated optical trap. Fertil Steril. 1989;52:870-3.
- [Google Scholar]
- Endometrial thickness and growth during ovarian stimulation: A possible predictor of implantation in in vitro fertilization. Fertil Steril. 1989;52:446-50.
- [Google Scholar]
- Biopsy of preimplantation mouse embryos: Development of micromanipulated embryos and proliferation of single blastomeres in vitro. Biol Reprod. 1989;40:145-52.
- [Google Scholar]
- Survival and pregnancy outcome after ultrarapid freezing of human embryos. Fertil Steril. 1990;53:469-72.
- [Google Scholar]
- Impairment of the hatching process following IVF in the human and improvement of implantation by assisting hatching using micromanipulation. Hum Reprod. 1990;5:7-13.
- [Google Scholar]
- Analysis of the first polar body: Preconception genetic diagnosis. Hum Reprod. 1990;5:826-9.
- [Google Scholar]
- Pregnancy after in vitro fertilization of human follicular oocytes collected from nonstimulated cycles, their culture in vitro and their transfer in a donor oocyte program. Fertil Steril. 1991;55:109-13.
- [Google Scholar]
- Poor oocyte quality rather than implantation failure as a cause of age-related decline in female fertility. Lancet. 1991;337:1375-7.
- [Google Scholar]
- Ultrasound-guided embryo transfer: A controlled trial. Fertil Steril. 1991;55:559-62.
- [Google Scholar]
- Implantation enhancement by selective assisted hatching using zona drilling of human embryos with poor prognosis. Hum Reprod. 1992;7:685-91.
- [Google Scholar]
- Pregnancies after intracytoplasmic injection of single spermatozoon into an oocyte. Lancet. 1992;340:17-8.
- [Google Scholar]
- Replacement of frozen embryos generated from epididymal spermatozoa: The first two pregnancies. Hum Reprod. 1992;7:652-3.
- [Google Scholar]
- Erbium YAG laser for micromanipulation of oocytes and spermatozoa. Lancet. 1992;340:115-6.
- [Google Scholar]
- Hamberger xx. In: Gordts S, ed. Proceedings of European Symposium on Micromanipulation. Leuven, Belgium: Drukkerij Nauwelaerts; 1993. p. :85.
- [Google Scholar]
- Aetiology of congenital absence of vas deferens: Genetic study of three generations. Hum Reprod. 1993;8:215-20.
- [Google Scholar]
- Conventional in-vitro fertilization versus intracytoplasmic sperm injection for patients requiring microsurgical sperm aspiration. Hum Reprod. 1994;9:1705-9.
- [Google Scholar]
- Pregnancies after testicular sperm extraction and intracytoplasmic sperm injection in non-obstructive azoospermia. Hum Reprod. 1995;10:1457-60.
- [Google Scholar]
- Blastocyst development and birth after in-vitro maturation of human primary oocytes, intracytoplasmic sperm injection and assisted hatching. Hum Reprod. 1995;10:3243-7.
- [Google Scholar]
- Pregnancies after intracytoplasmic sperm injection with cryopreserved testicular spermatozoa. Hum Reprod. 1996;11:1309-13.
- [Google Scholar]
- Severe oligozoospermia resulting from deletions of azoospermia factor gene on Y chromosome. Lancet. 1996;347:1290-3.
- [Google Scholar]
- The hypo-osmotic swelling test for selection of viable sperm for intracytoplasmic sperm injection in men with complete asthenozoospermia. Fertil Steril. 1996;65:972.
- [Google Scholar]
- Detection of deoxyribonucleic acid fragmentation in human sperm: Correlation with fertilization in vitro. Biol Reprod. 1997;56:602-7.
- [Google Scholar]
- Birth of a healthy female after intracytoplasmic sperm injection of cryopreserved human oocytes. Fertil Steril. 1997;68:724-6.
- [Google Scholar]
- A prospective randomized trial of blastocyst culture and transfer in in-vitro fertilization. Hum Reprod. 1998;13:3434-40.
- [Google Scholar]
- Births after intracytoplasmic injection of sperm obtained by testicular extraction from men with nonmosaic Klinefelter’s syndrome. N Engl J Med. 1998;338:588-90.
- [Google Scholar]
- First unaffected pregnancy using preimplantation genetic diagnosis for sickle cell anemia. JAMA. 1999;281:1701-6.
- [Google Scholar]
- Birth following vitrification of a small number of human oocytes: Case report. Hum Reprod. 1999;14:3077-9.
- [Google Scholar]
- Priming with human chorionic gonadotrophin before retrieval of immature oocytes in women with infertility due to the polycystic ovary syndrome. N Engl J Med. 1999;341:1624-6.
- [Google Scholar]
- Ovarian function after transplantation of frozen, banked autologous ovarian tissue. N Engl J Med. 2000;342:1919.
- [Google Scholar]
- Formulation of a protein-free medium for human assisted reproduction. Hum Reprod. 2000;15:145-56.
- [Google Scholar]
- Pregnancy and delivery after cryopreservation of zygotes produced by in-vitro matured oocytes retrieved from a woman with polycystic ovarian syndrome. Hum Reprod. 2001;16:1700-2.
- [Google Scholar]
- First live birth following blastocyst biopsy and PGD analysis. Reprod Biomed Online. 2002;4:35.
- [Google Scholar]
- First clinical application of comparative genomic hybridization and polar body testing for preimplantation genetic diagnosis of aneuploidy. Fertil Steril. 2002;78:543-9.
- [Google Scholar]
- First live birth after ovarian stimulation using a chimeric long-acting human recombinant follicle-stimulating hormone (FSH) agonist (recFSH-CTP) for in vitro fertilization. Fertil Steril. 2003;79:621-3.
- [Google Scholar]
- Local injury to the endometrium doubles the incidence of successful pregnancies in patients undergoing in vitro fertilization. Fertil Steril. 2003;79:1317-22.
- [Google Scholar]
- Normal birth after microsurgical enucleation of tripronuclear human zygotes: Case report. Hum Reprod. 2003;18:1319-22.
- [Google Scholar]
- rebirth after orthotopic transplantation of cryopreserved ovarian tissue. Lancet. 2004;364:1405-10.
- [Google Scholar]
- Single blastocyst transfer: A prospective randomized trial. Fertil Steril. 2004;81:551-5.
- [Google Scholar]
- Oocyte cryopreservation in oncological patients. Eur J Obstet Gynecol Reprod Biol. 2004;113(Suppl 1):S14-6.
- [Google Scholar]
- First successful pregnancy outcome after preimplantation genetic diagnosis for aneuploidy screening in embryos generated from natural-cycle in vitro fertilization combined with an in vitro maturation procedure. Fertil Steril. 2006;85:1510.e9-e11.
- [Google Scholar]
- Cryopreservation of intact human ovary with its vascular pedicle. Hum Reprod. 2006;21:3258-69.
- [Google Scholar]
- Yale Practice. 2007;12:2.
- Novel strategy with potential to identify developmentally competent IVF blastocysts. Hum Reprod. 2008;23:1748-59.
- [Google Scholar]
- Healthy twins delivered after oocyte cryopreservation and bilateral ovariectomy for ovarian cancer. Reprod Biomed Online. 2008;17:265-7.
- [Google Scholar]
- Live birth after polar body array comparative genomic hybridization prediction of embryo ploidy − The future of IVF? Fertil Steril. 2010;93:1006.e7-e10.
- [Google Scholar]
- Preimplantation genetic diagnosis for BRCA1/2-A novel clinical experience. Prenat Diagn. 2009;29:508-13.
- [Google Scholar]
- First pregnancy and live birth from cryopreserved embryos obtained from in vitro matured oocytes after oophorectomy in ovarian cancer patient. Hum Reprod. 2014;29:276-8.
- [Google Scholar]
- Crossing the line: The legal and ethical problems of foreign surrogacy. Reprod Biomed. 2009;19:151-2.
- [Google Scholar]
- 2016. The Surrogacy (Regulation) Bill. Available from: www.dhr.gov.in/sites/default/files/surrogacyregbill
- The ethical, legal and social issues impacted by modern assisted reproductive technologies. Obstet Gynecol Int 2012:686253.
- [Google Scholar]
- Frozen embryos: What are they and how should the law treat them. Clev State Law Rev. 1990;38:585.
- [Google Scholar]
- Fertility preservation in women undergoing cancer treatment. Lancet. 2004;363:1829-30.
- [Google Scholar]
- Environmental & lifestyle factors in deterioration of male reproductive health. Indian J Med Res. 2014;140:S29-35.
- [Google Scholar]
- Posthumous reproduction and its legal perspective. Int J Infertil Fetal Med. 2011;2:9-14.
- [Google Scholar]