Translate this page into:
Embryo reduction in a myomatous uterus and polypectomy during embryo transfer: Challenges well overcome
Address for correspondence: Dr. Nikita Naredi, ART Centre, Army Hospital (R&R), New Delhi - 110 010, India. E-mail: nikitanaredi@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Fibroids of the uterus, the most common benign pelvic tumors in women, as a sole cause of infertility has been debatable, as the incidence of fibroids as the cause of infertility in the absence of other obvious causes has been reported to be just 2-3%. Thus the management of myomas in the setting of infertility has also been controversial. However myomectomy has been considered ideal in a woman with sub fertility because the surgical removal of fibroid has definitely demonstrated improvement in pregnancy rate especially after assisted reproduction. Assisted Reproductive Technologies have resulted in an increase in the incidence of higher order multiple pregnancies which in turn is complicated by increased perinatal morbidity and mortality. Thus embryo reduction is offered to decrease the complication of prematurity and preterm birth due to multiple gestation. The technique of multifetal pregnancy reduction is not without risks especially in the presence of other pathology like multiple myomas. Herein we present a case of long duration infertility in the presence of multiple fibroids uterus which gets complicated by triplet gestation after IVF. Embryo reduction in the presence of these myomas is is a challenge both to the clinician in terms of the procedure and the patient because of the risks but subsequently has a successful pregnancy outcome.
Keywords
Multifetal pregnancy reduction (MFPR)
myomectomy
fibroid
INTRODUCTION
Fibroids of the uterus or uterine leiomyomas are the most common benign pelvic tumors in women during their reproductive years with an incidence of 25-40%, and this keeps increasing with advancing age. Fibroid, as a sole cause of infertility, has been a debatable issue and the incidence of fibroids in the absence of other obvious causes has been reported to be just 2-3%.[1,2] Thus, management of a myoma in the setting of infertility has been surrounded by considerable controversy and uncertainty. The treatment of fibroids can be medical, surgical, or the newer modalities like bilateral uterine artery embolization (UAE), laparoscopic myolysis, etc. However, it is myomectomy that is considered the ideal treatment in a woman with subfertility but this surgical modality is guided by the size, number, and precise location of the myoma.[3] Nonetheless, surgical removal of fibroid has demonstrated improvement in pregnancy rate, whether spontaneous or after assisted reproduction.[4]
Multifetal pregnancy constitutes a common iatrogenic complication of assisted reproductive technology (ART) and its incidence is directly related to the number of transferred embryos.[5] As multifetal gestation has a higher likelihood of obstetric and perinatal morbidity and mortality, first trimester transvaginal embryo reduction that is a safe and effective option is resorted to in order to decrease this complication.[6]
Here, we present a case of long duration infertility in the presence of pathology like multiple fibroid uterus that gets complicated by triplet gestation, an iatrogenic sequel of in vitro fertilization (IVF). In spite of myomectomy, residual multiple fibroids persisted and the lady underwent embryo reduction in the presence of these myomas that was the first challenge to both the clinician in terms of the procedure and the patient because of the risks. The second challenge ensued when a large cervical polyp was encountered during embryo transfer, which was removed at that particular time. In spite of the hindrances, the lady subsequently had a successful pregnancy outcome.
CASE REPORT
A 28-year-old lady a case of primary infertility married for 8 years was detected to have multiple uterine fibroids on evaluation for her subfertility. The male factor was within normal limits. The lady had fibroids ranging 2.5-6.5 cm, which were primarily intramural in location. She underwent laparoscopic myomectomy wherein three fibroids were removed. After myomectomy, in spite of cohabitation with husband for 2 years she was not able to conceive and thus, reported for treatment. On repeat evaluation and on ultrasonography, she was found to have three fibroids measuring 3.1 cm, 2.8 cm, and 2.56 cm each on the fundus, anterior wall, and posterior wall, respectively, and multiple seedling fibroids were observed as well. None of them were indenting the endometrial cavity. This was confirmed by a hysteroscopy. She underwent her first IVF cycle after downregulation with long agonist protocol and controlled ovarian hyperstimulation with recombinant gonadotropins. Two embryos of grade I at cell stage 4 were transferred; however, the result was unsuccessful. After a gap of 3 months, she was taken up for a second IVF cycle by the same protocol. During oocyte retrieval, 18 oocytes were recovered. Postovum pickup, her ovaries were enlarged and there was fluid in the pouch of Douglas. As she was at risk of developing ovarian hyperstimulation syndrome (OHSS), she was managed conservatively with vascular endothelial growth factor (VEGF) antagonist cabergoline and intravenous fluids and monitored closely, both clinically and ultrasonologically. She was planned for a frozen embryo transfer and thus, her embryos were vitrified. After 2 months of oocyte recovery, a frozen embryo transfer cycle was started and the endometrium was prepared from the second day of menstruation with oral administration of estradiol valerate (Progynova 2 mg) tablets twice a day for 4 days and thrice a day thereafter for 8 days. After 12 days of endometrial priming when the endometrial thickness reached 7.5 mm, micronized progesterone 100 mg was injected intramuscularly and oral administration of dydrogesterone 10 mg (Duphaston 10 mg; Solvay) was started and embryo transfer was carried out on the third day. At the time of embryo transfer, per speculum examination revealed a cervical fibroid polyp measuring 2.5 cm that was extruding from the cervical canal. As the embryos were already thawed for the transfer, the patient underwent polypectomy by manual rotation and embryo transfer was done. Three embryos of grade I were transferred in view of her second IVF cycle with coexistent pathology in the form of multiple fibroids persisting in the uterus. This time, all the three embryos got implanted and resulted in a triplet pregnancy [Figure 1]. She underwent embryo reduction transvaginally under ultrasound guidance at 8 weeks 3 days period of gestation after proper counseling about the complications and a written informed consent was obtained. Embryo reduction was done transvaginally by intracardiac instillation of potassium chloride in one of the fetal thorax of the triplet pregnancy, which was farthest from the cervix. The embryo reduction needle had to traverse through one of the large fibroids and smaller seedling myomas [Figure 2]. The negotiation of the embryo reduction needle through the fibroids was difficult because of its consistency and the larger distance to be traversed before reaching the sac. Asystole of the fetal cardiac activity was confirmed and the procedure was successful and one fetus was reduced. The patient was hospitalized and monitored for any complications in the form of bleeding, infection, etc. She was discharged on the third day. The lady underwent close antenatal care. She had a premature rupture of membranes at 36 weeks 2 days period of gestation and delivered healthy twins.

- Line diagram of the ultrasound picture of triplet gestation in a myomatous uterus
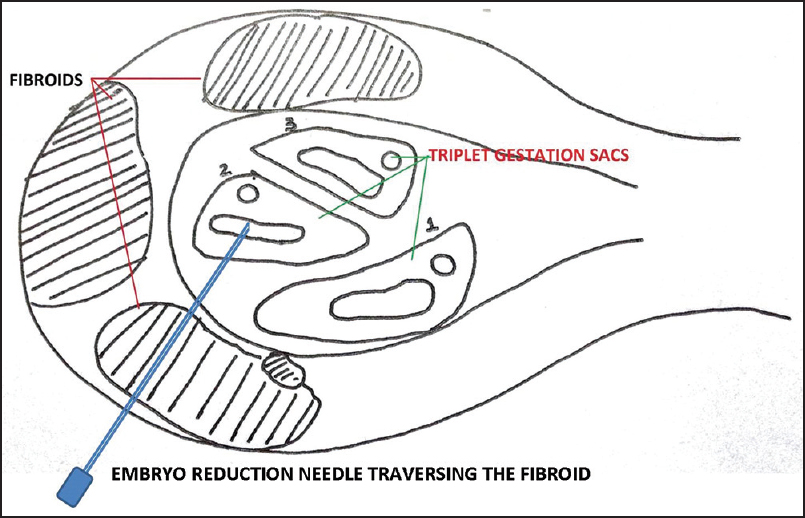
- Line diagram of the ultrasound picture showing embryo reduction through the fibroid
DISCUSSION
Although the relationship between fibroids and infertility is inconclusive, several mechanisms have been postulated by which fibroids may reduce fertility. It is believed that fibroids may interfere with sperm migration, ovum transport, and embryo implantation.[7] The various detrimental effects that have been proposed are the following: Alteration of the uterine cavity contour causing mechanical pressure, occurrence of dysfunctional uterine contractility interfering with ovum or sperm transport, and an inadequate blood supply to the endometrium, resulting in focal endometrial attenuation to explain reduced embryo implantation.[8] However, these lesions have been elucidated to be responsible for only 2-3% of infertility cases.[1,2] Nevertheless, with the advent of ARTs, particularly IVF, the relationship between fibroids and infertility has become clearer. The results from IVF cycles have provided precious information on the impact of myomas on embryo implantation. Various studies have documented a significant negative impact of both submucosal and intramural fibroids on pregnancy rate.[9,10] Workers have also revealed that the size of the fibroids is positively related to implantation failure, in particular when the diameter of the lesion exceeds 4 cm.[11]
The management of uterine leiomyomas in the setting of subfertility has been suggested to be primarily surgical. The surgical removal of myomas, i.e., myomectomy is, however, guided by the number, size, and precise location of the fibroids in the uterus. It is generally accepted that regardless of the means by which myomectomy is performed (hysteroscopy, laparoscopy, or laparotomy), excision of submucous myoma improves the chances to conceive, whereas myomectomy of large intramural fibroids can improve the overall outcome of pregnancy.[1] With the postsurgical pregnancy rate across various studies being as good as 57-61%, our patient was also taken up for myomectomy and the three accessible and large fibroids were removed, as complete eradication of fibroids in cases with multiple fibroids is an impossible task with available uterine preserving therapies.[1] Small seedling fibroids can grow in size anytime during the reproductive years as in our case.
The efficacy of myomectomy on IVF outcome has also been varied, with some suggesting a better pregnancy rate while others documenting a significant improvement in pregnancy outcome; however, previous myomectomy has not affected IVF cycles negatively. Nevertheless, our patient did not conceive after the first IVF cycle but the second cycle was successful and she had a triplet gestation in spite of multiple seedling fibroids.
Higher-order multiple gestation, an iatrogenic complication of ART, is associated with an increased risk of premature delivery and its attendant sequel of increased perinatal morbidity and mortality. Multifetal pregnancy reduction (MFPR) is an effective procedure that was designed to decrease the likelihood of prematurity in these patients by reducing the number of live fetuses.[12] Nevertheless, this invasive procedure is not without risks with the potential to result in loss of the entire pregnancy as a major risk and the other complications being spotting, infection, and miscarriage of one of the remaining sacs.[13] It also causes considerable emotional and psychological distress for some couples and thus, we had counseled our patient about the pros and cons of the procedure. Apart from the inherent risks of the technique of MFPR, carrying out the reduction in the presence of multiple fibroids is a challenge in itself. The difficulties encountered are due to the number of fibroids, the consistency of the fibroids through which the needle has to negotiate, and the size of the uterus that increases due to the myomas. The challenges in the form of IVF with fibroids, embryo transfer immediately after an endocervical polypectomy, and embryo reduction in the presence of myomas were all circumvented successfully and our patient, with close supervision and regular antenatal care, delivered two healthy babies.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- What are the implications of myomas on fertility? A need for a debate? Hum Reprod. 2002;17:1424-30.
- [Google Scholar]
- Controversies and challenges in the modern management of uterine fibroids. BJOG. 2004;111:95-102.
- [Google Scholar]
- Fibroids and infertility: An updated systematic review of the evidence. Fertil Steril. 2009;91:1215-23.
- [Google Scholar]
- Fibroids and female reproduction: A critical analysis of the evidence. Hum Reprod Update. 2007;13:465-76.
- [Google Scholar]
- Reducing multiple pregnancies by restricting the number of embryos transferred to two at the first embryo transfer attempt. Hum Reprod. 1998;13:3550-4.
- [Google Scholar]
- Multifetal pregnancy reduction: A review of the world results for the period 1993-1996. Eur J Obstet Gynecol Reprod Biol. 1997;75:183-90.
- [Google Scholar]
- The ultrastructure of fibromyomatous myometrium and its relationship to infertility. Hum Reprod Update. 1998;4:520-5.
- [Google Scholar]
- Doppler ultrasound examination of uterine arteries on the day of oocyte retrieval in patients with uterine fibroids undergoing IVF. Hum Reprod. 2002;17:765-70.
- [Google Scholar]
- Fibroids and infertility: A systematic review of the evidence. Obstet Gynecol Surv. 2001;56:483-91.
- [Google Scholar]
- Effect of fibroids on fertility in patients undergoing assisted reproduction. A structured literature review. Gynecol Obstet Invest. 2005;59:225-30.
- [Google Scholar]
- Impact of subserosal and intramural uterine fibroids that do not distort the endometrial cavity on the outcome of in vitro fertilization-intracytoplasmic sperm injection. Fertil Steril. 2004;81:582-7.
- [Google Scholar]
- Pregnancy outcome after multifetal reduction via early transvaginal embryo aspiration: Mansoura fertility care unit experience. Middle East Fertil Soc J. 2007;12:168-73.
- [Google Scholar]
- Multifetal pregnancy reduction by transvaginal puncture: Evaluation of the technique used in 134 cases. Am J Obstet Gynecol. 1993;168:799-804.
- [Google Scholar]







