Translate this page into:
Fertility preservation in Females—where are we today?
Address for correspondence: Dr Rupali, Senior Consultant, IVF & Reproductive Medicine Indraprastha Apollo Hospital, New Delhi, India. e-mail: rupalibassi@hotmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
With improvement in the survival rates of cancer, Fertility Preservation is the need of the hour. The modalities for fertility preservation vary from the classical method of ovarian transposition to simple treatments like giving drugs to reduce the chances of gonadotoxicity to oocyte and ovarian tissue cryopreservation. Various factors influence the decision of the treatment in cases of cancer survivors primarily being the age of the patient and the time in hand to do the treatment. This article is a review of the options of treatment available and increasing the awareness amongst the other clinicians.
Keywords
Chemotherapy
cryopreservation
fertility preservation
gonadotoxicity
radiotherapy
random start protocols
INTRODUCTION
There is an increasing incidence of cancer all around the world. Newer developments in cancer therapy have been a boon to the patents suffering from cancer.
In the year 2018, there were 1,15,896 new cases of cancer diagnosed in the Indian subcontinent.[1]
With an improved long-term survival and the potential gonadotoxicity of these therapeutic modalities, fertility preservation forms an integral part in the management of the young cancer survivors.
FEMALE FERTILITY AND CANCER THERAPY
The effects of various chemotherapeutic and radiotherapy agents could vary from no effect, transient reversible damage to permanent infertility. The extent of damage an agent could cause may also differ from person to person. There are various factors that would alter the gonadotoxic effect of various agents.
AGE
Chemotherapy has differential effects on primordial, dormant follicles and growing, larger ovarian follicles. Chemotherapy targets actively dividing cells and therefore, destroys mature ovarian follicles during treatment, specifically by inducing apoptosis in granulosa cells.[2]
Clinically, patients exposed to chemotherapy initially stop menses as a result of the destruction of growing follicles and resume cycling after a period of recovery. Even low doses of chemotherapy can wipe out the population of maturing follicles, but partial ovarian reserve remains intact, allowing for the eventual resumption of menses. The means by which chemotherapy induces damage to the primordial follicle stockpiles, which represent future fertility potential, remains unclear.
In a study by Meirow and Dow of 168 individuals it was observed that the patients who maintained ovarian function post treatment were found to be significantly younger (27.4 + 8.3 years) than those who lost ovarian function (34.7 + 8 years).[3]
In a study of 78 patients who were undergoing treatment for Hodgkin lymphoma, it was observed that there was a significantly less gonadotoxicity when the age of the patient was less than 25 years.[4]
This age effect is mostly owing to the strong negative correlation between age and the nongrowing follicle population, representing ovarian reserve. Older women have diminished primordial follicular pool as a result the effects of chemotherapy seem more marked in these group of women.[1]
CHEMOTHERAPEUTIC AGENTS AND FERTILITY POTENTIAL
There are six main classes of chemotherapeutic drug groups: alkylating agents, platinum derivatives, antibiotics, antimetabolites, plant alkaloids, and the taxanes.
The extent of ovarian damage is influenced by the type of drug being administered.[5] Alkylating agents are often and effectively used in combination chemotherapy treatment but they are also associated with particularly high levels of premature ovarian failure. It has been observed that alkylating agents are associated with one of the highest age-adjusted risk of ovarian failure rates, followed by other drug families. The least gonadotoxic agents would be anti-metabolite and antibiotic categories.[6] Although there are limited data on the effects the taxane family on ovarian failure rates, however, inclusion of paclitaxel, a member of the taxane family, to traditional AC (doxorubicin, cyclophosphamide) treatment significantly increases the risk of ovarian damage after treatment in patients undergoing chemotherapy.[7]
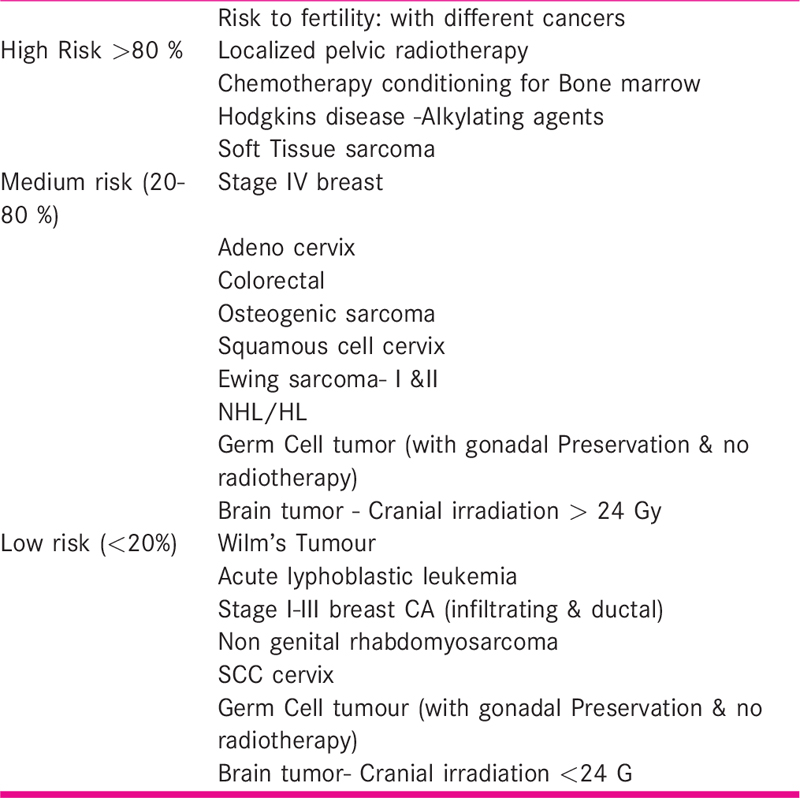
The degree of goandotoxicity varies with the associated cancer as listed in Table 1.
TYPE OF PROTOCOL
In the current era, the main modality of chemotherapy is a combination protocol. These drugs have varied effects, especially when used in a combination.
In breast cancer survivors, it was observed that the patients who underwent combination chemotherapy with regimens containing cyclophosphamide, methotrexate and fluorouracil had highest incidence of amenorrhoea in the post treatment period. Furthermore, the treatment protocol of cyclophosphamide, doxorubicin and fluorouracil (CAF) also induced high rates of ovarian failure. Patients on therapy with AC (doxorubicin and cyclophosphamide) showed a better eventual recovery of ovarian function after treatment.[8]
In patients who have undergone bone marrow transplantation (BMT) there is an extremely high ovarian failure rates. There is a significant risk of ovarian failure after treatment with total body irradiation (TBI). In a large study by Sanders et al.[9] of 718 long-term survivors, treated with chemotherapy and/or TBI as conditioning treatment before a bone marrow transplant, 532 had received TBI (10–15.75 Gy, single exposure or fractionated) and 186 chemotherapy, with either cyclo-phosphamide or busulphan. It was observed that after TBI, 90% of the patients developed ovarian failure and after cyclophosphamide or busulphan 60% had failure of ovarian function.
MECHANISM OF OVARIAN DAMAGE
Follicular apoptosis
Chemotherapy has been suggested to induce damage to primordial follicles by inducing apoptosis. Electron microscopy has shown that within hours of chemotherapy exposure, primordial follicles become surrounded by abnormally thick basal lamina.[10]
Cortical fibrosis
Chemotherapeutic agents are known to cause ovarian cortical fibrosis and blood vessel damage. The main effect of these chemotherapeutic agents on ovarian tissue is by hyalinisation of cortical blood vessels, neovascularisation and cortical fibrosis. These further lead to local ischemia, thereby affecting the growth and survival of primordial follicles. In vivo experiments have shown that there are triangular areas of fibrosis coinciding with a depletion of primordial follicles. It has also shown to impair neovascularisation, which is critical for normal follicle growth within the territory of the damaged vasculature.[11]
Follicular “Burn-Out” hypothesis
A novel hypothesis to explain the loss of primordial follicular pool is the “burn-out” mechanism. In patients undergoing chemotherapy, the growing follicles are destroyed and as a result, there is a possible decrease in granulosa cell-derived paracrine growth factors such as anti-Mullerian hormone (AMH). There is an increased activation of primordial follicles, resulting in greater numbers of large follicles that undergo atresia, and eventually resulting in a premature “burn-out” of the primordial follicle reserve.[12]
Radiation-induced damage
Malignancies of the central nervous system and hematology require high-dose ionising radiation. It is an established practice to shield the gonads from the field of radiation whenever possible. However, this may not be feasible in cases when the radiation field overlaps with the ovaries or when total body irradiation is required as a conditioning treatment for bone marrow transplantation.
Radiotherapy to the pelvis results in ovarian injury and diminished follicle reserve; the extent of damage is largely based on patient’s age, treatment dose and the irradiation field.
The location of the radiation field impacts the degree of ovarian damage. In cases of total body irradiation including the abdominal field ovarian failure has been observed in approximately 90% to 97% of patients in long-term follow-up.[9,13]
Age of the patient is an important prognosticating factor as the ovary is more resistant to radiation earlier in life, and the sensitivity progressively increasing with age.[14]
Age of the patient would also alter the gonadotoxic effect. Young prepubertal patients can tolerate a radiotherapy up till 15 Gy with a risk of amenorrhoea being 30–70%. Whereas in the reproductive age group, this value reaches as low as 5–6 cGy.[15]
The dose of radiation is an important factor for determining the risk of premature ovarian failure in cancer survivors. In a study by Wallace et al.[14] showed that the lethal dose of radiation is 2 Gy, and at this dosage approximately half of the total number of nongrowing follicles would be lost (LD50).
Approach to a patient for fertility preservation
A multidisciplinary team can assist in navigating the conflicting view points in the patient-parent-physician triad.[16] A multidisciplinary team for fertility preservation would include the oncologist, a general paediatrician or adolescent medicine physician, a gynaecologist or reproductive endocrinologist, a therapist or psychiatrist, a social service representative and an ethics committee.[16,17]
Counselling
Counselling in fertility preservation plays a major role in the patient management, as the ongoing negative experiences are associated with decisional conflict and decisional regret.[18,19]. It can sometimes be overwhelming for the patients as well as the parents, and could suffer from information overload.[20] So, a very careful and thoughtfully devised way of counselling should be adopted.
Various decision aids such as brochures, handouts and information booklets are utilised to enhance the confidence of knowledge about oocyte cryopreservation. Integrating a nurse navigator in the programme has shown to increase the frequency of fertility preservation referrals without increased time to cancer treatment.[21,22]
Genetic counselling by the experts also forms an integral part of the counselling, where the future impact of fertility potential and risk of transmission of the malignancy in the offspring should be discussed with the patient and her family members.
METHODS OF CRYOPRESERVATION
Oocyte cryopreservation
Embryo cryopreservation is a well-established modality in the field of assisted reproductive technology. Oocyte cryopreservation became standard of care in 2013.[23,24]
Oocyte cryopreservation is considered only if the chemotherapy can be delayed by 2–3 weeks. It is mainly utilised in the post pubertal adolescent age group, so as to allow for future reproductive flexibility, as they typically might not have a long-term partner and often would not desire to choose an anonymous sperm donor.
The live birth rates from embryos created from oocyte cryopreservation appear to be equivalent to cryopreserved embryos.[25,26]. Studies have shown that there is no increased risk of aneuploidy in the embryos created from cryopreserved oocytes, even with long-term storage.[27] Although, as of now there are limited data on the duration of storage, though a child was recently born in the United Kingdom from an oocyte reportedly frozen 14 years prior to fertilisation.[28]
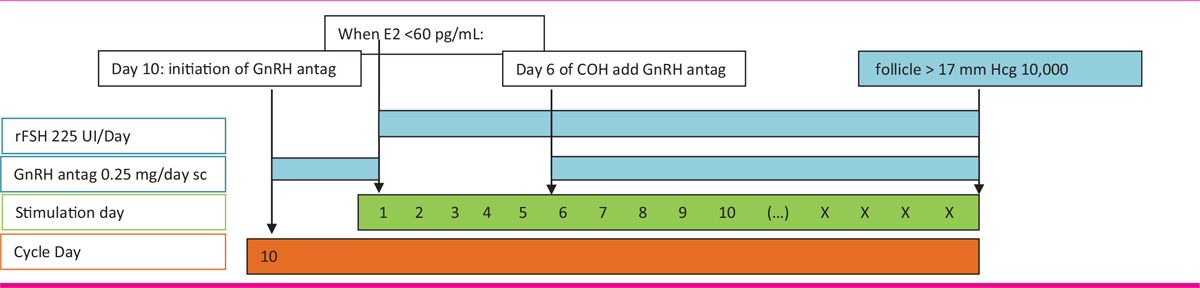
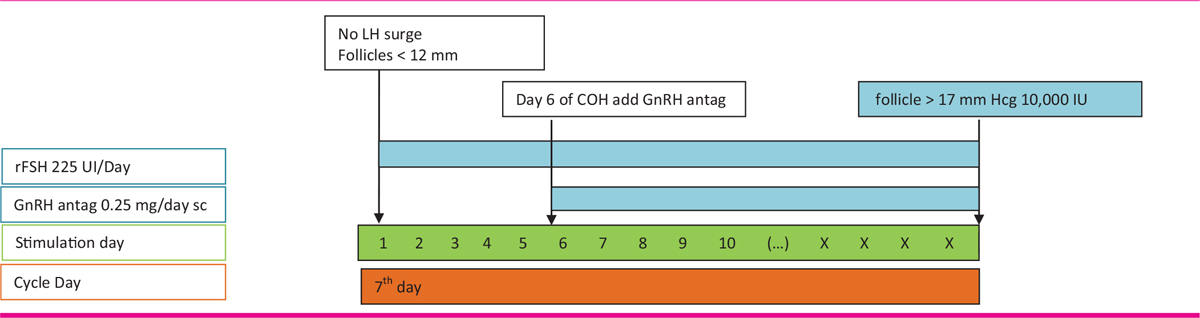
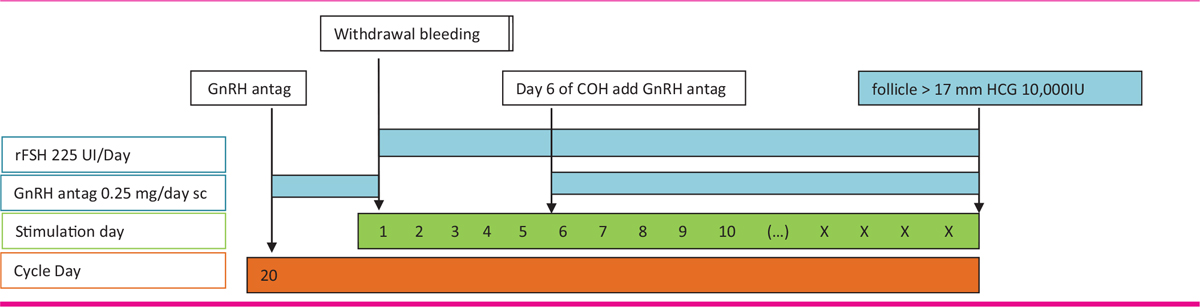
For controlled ovarian stimulation “random start” protocols are utilised, where stimulation can be started at any given point in the menstrual cycle. This usually requires 2–3 weeks to complete the procedure, which is typically acceptable to oncology providers. Studies have shown that the random start protocols appear to be as effective as conventional start protocols.[29,30]
The random start cycles, as the name implies, can be started at any time of the cycle, either in the mid-follicular phase or the luteal phase. During the stimulation, an initial transvaginal ultrasound may be performed to evaluate the status of the ongoing mature follicle, the number and size of antral follicles.
Studies have shown that the presence of corpus luteum or the levels of serum progesterone do not adversely affect neither the outcome in terms of fertilisation or the synchronisation of the cohort of the follicles.[31]
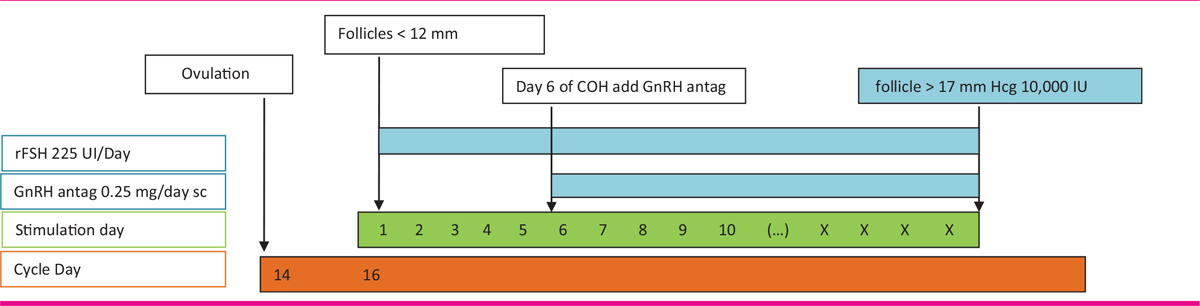
If the patient reports in the early follicular phase and the leading follicle has not reached 12 mm, a conventional stimulation with gonadotropins along with the gonadotropin-releasing hormone (GnrH) antagonists can be started.
For stimulation in the later part of the follicular phase, ovulation can be triggered using Hcg and after 2 to 3 days of ovulation, the gonadotropins may be started. In this scenario the important thing to make note is that the Serum Progesterone levels are of no significant value for the dose of gonadotropins or the total period of stimulation.
While patients requiring stimulation in the mid-follicular phase or in Luteal halt protocols, a higher dose of Gnrh Antagonist (3 mgs single) or 250 mcg daily multiple doses may be required for bringing down the Estradiol levels to below 60 pg/ml.[32,33] Once the desired levels are achieved then the stimulation could be started with Recombinant FSH followed by GnRH antagonist at the follicular sizes of 12 to 14 mm.[34] This would subsequently be followed by a trigger at 18 mm size of the follicles.
Presence of a corpus luteum does not hamper the stimulation of the ovaries. Indeed, studies have shown that a similar number of oocytes retrieved in both the ovaries were similar in cases of presence of Corpus Luteum.
GnRH antagonist administration may be required for a slightly longer duration than a conventional cycle. The GnRH ensures prevention of spontaneous ovulation and the cycle is monitored closely with the blood analysis and transvaginal ultrasounds. Once adequate follicular development is achieved, oocyte retrieval is performed as an outpatient procedure under conscious sedation with ultrasound-guided transvaginal aspiration of each follicle.
Use of Aromatase Inhibitors, such as Letrozole, during COH helps the clinician to keep the levels of estradiol below the supraphysiological levels. This is more important in cases of estrogen-sensitive cancers, such as estrogen receptor positive breast cancer or endometrial cancer.[35,36] Letrozole may be continued even after the stimulation is over if the estradiol levels are < 500pg/ml.[31]
Tamoxifen is a Selective estrogen receptor Modulator, is used in patients with estrogen-sensitive breast cancer. The anti-estrogenic effect on the hypothalamic/pituitary axis causes a negative feedback effect on the levels of circulating estrogen and thereby resulting in an increase in GnRH secretion from the hypothalamus and a subsequent release of FSH from the pituitary-stimulating follicular development. It is used in a dose of 20–60 mg/day.
Multiple stimulations in the same cycle may be required in patients of advanced age and/or a poor ovarian reserve. Using the random start protocols, stimulation can be restarted within a few days after ovulation. The different protocols of stimulation have been demonstrated in the enclosed Tables 2-5.
Ovarian transposition
Ovarian transposition is an age old and effective method considered in all age groups from pre-pubertal to pre-menopausal women and girls requiring pelvic radiation for conditions not involving the ovary.[37,38,39]
The preferred method for ovarian transposition is by laparoscopic route.[40,41] It involves fixing of the ovaries to the anterolateral abdominal wall. After fixation 5 mm metallic clips are placed at the base of the ovary for radiologic identification.
This method has shown that ovarian function is preserved in approximately 90% of the cases. Side effects like ovarian cysts have been observed in 14% of the patients and metastasis in 0.9% of patients.[41,42]
Gonadotropin-releasing hormone (GnRH) agonist
Chemotherapeutic agents have a differential toxicity towards the different stages of growing follicles. The gonadotoxicity is lesser on the resting primordial follicles as compared to the actively growing follicles.[43]
GnRH agonist acts by suppression of pituitary-hypothalamic axis, decreased utero-ovarian perfusion and activation of GnRH alpha receptors on the ovary to decrease apoptosis.[44,45]
There are several recent meta-analyses that show no difference in gonadotoxicity in the GnRH agonist group and the control group.[46,47]
The current status of GnRH agonists for fertility preservation remains controversial and current ASCO guidelines do state that GnRHa may be offered to patients in the hope of reducing the likelihood of chemotherapy-induced ovarian insufficiency. However, GnRHa should not be used in place of proven fertility preservation methods, do not recommend relying on this method alone for fertility preservation.[23]
EXPERIMENTAL METHODS OF FERTILITY PRESERVATION
Ovarian tissue cryopreservation
Ovarian tissue cryopreservation (OTC) is currently one of the primary options available to pre-pubertal girls to preserve fertility prior to gonadotoxic treatment. The first transplantation of frozen-thawed ovarian tissue was performed in the year 2000, and since then, over 86 live births have been reported.[48,49,50]
The overall live birth rate after autotransplantation of frozen-thawed ovarian cortex has been reported to be around 30%.[49,51]
One of the main advantages of the procedure is it does not require any delay in the treatment as no ovarian stimulation is required.
Due to non-delay of therapy this can also be offered to adult women who are not candidates for oocyte/embryo cryopreservation. The amount of tissue harvested from the patient differs depending on surgical technique. Oocyte tissue cryopreservation is still experimental and further research needs to be undertaken before standardized protocols are established.
Strips of cortical tissue are created with approximate dimensions of 1 cm x 5 mm x 1 mm, each are to be fashioned. A total of 4–5 strips are to be prepared in an individual for autotransplantation and further use. The mean duration of the graft longevity has been reported up to 8 years.[52]
In vitro maturation (IVM)
IVM refers to the process by which the immature oocytes are aspirated after minimal or no stimulation followed by maturation in vitro. These mature oocytes are then cryopreserved directly or may be fertilised and preserved as embryos.
Immature oocytes can also be collected in the luteal phase and from antral follicles in the ovarian tissue removed for cryopreservation.
The main advantage of this procedure is shorter period of stimulation which is of utmost importance in case of oncology patients undergoing fertility preservation. This technique has been performed experimentally and with good success in girls as young as 5 years. So far, this technique has mainly been used in polycystic ovary syndrome patients, and data on efficacy and safety of IVM in cancer patients are not available. Pregnancy rates with IVM are low being between 10% and 15%.
Practical and ethical aspects on fertility preservation
This field of medicine is still under developed due to various factors that have hindered the further development in the field.
Poor knowledge of the treating physicians regarding the availability of fertility preservation services is a big barrier in the management of these patients. The current American Society of Clinical oncology released guidelines in 2018, which clearly mentions that all treating oncologists should discuss the possibility of fertility preservation with the patient at the time of diagnosis, wherever applicable.
Psychological stress, on being diagnosed with the cancer, plays a major role in the decision made by the patient and her relatives, further worsens the prospects of fertility preservations.
The financial aspects also should be discussed with the patient, as this is an additional stress, over and above the therapeutic costs of the cancer.
A disciplined and coordinated team effort is integral for a successful programme and ensure betterment of the patient.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Cancer Statistics. Indian Council of Medical Research; 2019.
- Toxicity of chemotherapy and radiation on female reproduction. Clin Obstet Gynecol. 2010;53:727-39.
- [Google Scholar]
- Epidemiology and infertility in cancer patients. In: Togas T, Roger G, eds. Preservation of Fertility. London: Taylor and Francis Publishing; 2004. p. :21-38.
- [Google Scholar]
- Treatment of early-stage Hodgkin’s disease with four cycles of ABVD followed by adjuvant radiotherapy: analysis of efficacy and long-term toxicity. Haematologia. 2000;85:1032-9.
- [Google Scholar]
- American Society of Clinical Oncology recommendations on fertility preservation in cancer patients. J Clin Oncol: Official J Amer Soc Clin Oncol. 2006;24:2917-31.
- [Google Scholar]
- Reproduction post-chemotherapy in young cancer patients. Mol and Cell Endocr. 2000;169:123-31.
- [Google Scholar]
- Incidence, time course, and determinants of menstrual bleeding after breast cancer treatment: a prospective study. J Clin Oncol. 2006;24:1045-51.
- [Google Scholar]
- Epidemiology and infertility in cancer patients. In: Togas T, Roger G, eds. Preservation of Fertility. London: Taylor and Francis Publishing; 2004. p. :21-38.
- [Google Scholar]
- Pregnancies following high dose cyclo- phosphamide with or without high-dose busulfan or total body irradiation and bone marrow transplantation. Blood. 1996;87:3045-52.
- [Google Scholar]
- Infertility: ultrastructure of human ovarian primordial follicles after combination chemotherapy for Hodgkin’s disease. Hum Reprod. 1993;8:2080-7.
- [Google Scholar]
- Cortical fibrosis and blood-vessels damage in human ovaries exposed to chemotherapy. Potential mechanisms of ovarian injury. Hum Reprod. 2007;2:1626-33.
- [Google Scholar]
- Control of primordial follicle recruitment by anti-Mullerian hormone in the mouse ovary. Endocrinology. 1999;140:5789-96.
- [Google Scholar]
- Ovarian failure following abdominal irradiation in childhood: natural history and prognosis. Clin Oncol (Royal Coll Radiologists (Gr Br)). 1989;1:75-9.
- [Google Scholar]
- Reproductive potential in survivors of childhood malignancy. Pediatrician. 1991;18:61-70.
- [Google Scholar]
- Oncofertility for adolescents: when parents and physicians disagree about egg cryopreservation for a mature minor. AMA J Ethics. 2015;17:826-33.
- [Google Scholar]
- Developing a referral system for fertility preservation among patients with newly diagnosed cancer. J Natl Compr Canc Netw. 2011;9:1219-25.
- [Google Scholar]
- Patient perceptions of reproductive health counselling at the time of cancer diagnosis: a qualitative study of female California cancer survivors. J Cancer Surviv. 2012;6:324-32.
- [Google Scholar]
- Deciding about fertility preservation after specialist counselling. Hum Reprod. 2014;29:1721-9.
- [Google Scholar]
- Early referral makes the decision-making about fertility preservation easier: a pilot survey study of young female cancer survivors. Support Care Cancer. 2015;23:1663-7.
- [Google Scholar]
- Fertility preservation in young female cancer patients: development and pilot testing of an online decision aid. J Adolesc Young Adult Oncol. 2018;7:30-6.
- [Google Scholar]
- Does a dedicated program for young breast cancer patients affect the likelihood of fertility preservation discussion and referral? Breast. 2016;27:22-6. 44
- [Google Scholar]
- Fertility preservation in patients with cancer: ASCO Clinical Practice Guideline Update. J Clin Oncol. 2018;36:1994-2001.
- [Google Scholar]
- Oocyte cryopreservation: where are we now? Human Reproduction Update. 2016;22:440-9.
- [Google Scholar]
- A comparison of live birth rates and perinatal outcomes between cryopreserved oocytes and cryopreserved embryos. J Assist Reprod Genet. 2017;1-8(34):1359-66.
- [Google Scholar]
- Practice Committee of American Society for Reproductive Medicine. Fertil Steril. 2014;101:1237-43.
- [Google Scholar]
- Long-term cryopreservation of human oocytes does not increase embryonic aneuploidy. Fertil Steril. 2015;103:662-8.
- [Google Scholar]
- Female fertility preservation in the pediatric and adolescent cancer patient population. Best Pract Res Clin Obstet Gynaecol. 2018;48:147-57.
- [Google Scholar]
- Effective method for emergency fertility preservation: random-start controlled ovarian stimulation. Fertil Steril. 2013;100:1673-80.
- [Google Scholar]
- Random-start ovarian stimulation in women desiring elective cryopreservation of oocytes. Reprod BioMed. 2017;35:400-6.
- [Google Scholar]
- Random-start ovarian stimulation in patients with cancer. Current Opinion in Obstetrics and Gynecology. 2015;27:215-21.
- [Google Scholar]
- Preliminary experience of the use of a gonadotrophin-releasing hormone antagonist in ovulation induction/in-vitro fertilization prior to cancer treatment. Hum Reprod. 1999;14:2665-8.
- [Google Scholar]
- Reproductive outcome using a GnRH antagonist (cetrorelix) for luteolysis and follicular synchronization in poor responder IVF/ICSI patients treated with a flexible GnRH antagonist protocol. Reprod Biomed Online. 2005;11:679-84.
- [Google Scholar]
- Fertility preservation in women with breast cancer. Clin Obstet Gynecol. 2010;53:753-62.
- [Google Scholar]
- Ovarian stimulation and fertility preservation with the use of aromatase inhibitors in women with breast cancer. Fertil Steril. 2012;98:1363-9.
- [Google Scholar]
- Long-term safety of letrozole and gonadotropin stimulation for fertility preservation in women with breast cancer. J Clin Endocrinol Metab. 2016;101:1364-71.
- [Google Scholar]
- Ovarian transposition in young women and fertility sparing. Eur Rev Med Pharmacol Sci. 2015;19:3418-25.
- [Google Scholar]
- Outcomes of ovarian transposition in gynaecological cancers; a systematic review and meta-analysis. J Ovarian Res. 2014;7:69.
- [Google Scholar]
- Preservation of ovarian function by ovarian transposition performed before pelvic irradiation during childhood. J Pediatr. 1992;121:880-4.
- [Google Scholar]
- Laparoscopic unilateral ovarian transposition prior to irradiation: prospective study of 20 cases. Cancer. 1996;77:2638-45.
- [Google Scholar]
- A new approach for laparoscopic ovarian transposition before pelvic irradiation. Gynecol Oncol. 2007;105:234-7.
- [Google Scholar]
- Ovarian transposition in young women and fertility sparing. Eur Rev Med Pharmacol Sci. 2015;19:3418-25.
- [Google Scholar]
- Utility of GnRH-agonists for fertility preservation in women with operable breast cancer: is it protective? Curr Breast Cancer Rep. 2013;5:302-8.
- [Google Scholar]
- How to preserve fertility in young women exposed to chemotherapy? The role of GnRH agonist cotreatment in addition to cryopreservation of embrya, oocytes, or ovaries. Oncologist. 2007;12:1044-54.
- [Google Scholar]
- Hyperstimulation and a gonadotropin-releasing hormone agonist modulate ovarian vascular permeability by altering expression of the tight junction protein Claudin-5. Endocrinology. 2006;147:694-9.
- [Google Scholar]
- GnRH-analogues and oral contraceptives for fertility preservation in women during chemotherapy. Hum Reprod Update. 2008;14:543-52.
- [Google Scholar]
- Gonadotropin-releasing hormone analog cotreatment for preservation of ovarian function during gonadotoxic chemotherapy: a systematic review and meta-analysis. Fertil Steril. 2011;95:906-14.
- [Google Scholar]
- Ovarian function after transplantation of frozen, banked autologous ovarian tissue. N Engl J Med. 2000;342:1919.
- [Google Scholar]
- Current success and efficiency of autologous ovarian transplantation: a meta-analysis. Reprod Sci. 2017;24:1111-20.
- [Google Scholar]
- Ovarian cortex transplantation: 60 reported live births brings the success and worldwide expansion of the technique towards routine clinical practice. J Assist Reprod Genet. 2015;32:1167-70.
- [Google Scholar]
- Efficacy of ovarian tissue cryopreservation for fertility preservation: lessons learned from 545 cases. Hum Reprod. 2017;32:1046-54.
- [Google Scholar]
- Assessment of long term endocrine function after transplantation of frozen-thawed human ovarian tissue to the heterotopic site: 10 year longitudinal follow-up study. J Assist Reprod Genet. 2012;29:489-93.
- [Google Scholar]







