Translate this page into:
Maternal age and its impact on implantation and clinical pregnancy rates in patients undergoing day 3 versus day 5 embryo transfer in Indian population
Address for correspondence: Kumkum Rana, N-17 (1004), Jaypee Aman, Sector 151, Noida, Uttar Pradesh, India. E-mail: ranakumkum25@gmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objective:
The present study compared the reproductive outcomes (implantation rate, pregnancy rate) between day 3 and day 5 transfers in two different age groups of patients (aged <36 years vs. aged ≥36 years).
Materials and methods:
The present study was conducted in the RIDGE IVF Centre, Gouri Hospital, New Delhi (India), after obtaining institutional ethical committee clearance. For frozen embryo transfers (FETs), day 3 embryos were thawed using Origio vitrification warming kit. The outcome parameters [anti mullerian hormone (AMH), antral follicle count (AFC), follicle-stimulating hormone, E2, mean number of oocytes retrieved, embryo grades A, B, and C, beta human chorionic gonadotropin (HCG), number of sacs, miscarriages, and live birth rate] were compared between age <36 versus >36 years, day 3 versus day 5 embryo, and fresh versus frozen embryo. The unpaired t test was used for comparing quantitative variables and Chi-squared test was used for comparing qualitative variables.
Results:
The mean age of the study population was 31.84 ± 3.74 years. The mean AMH, AFC, and oocytes retrieved were significantly more among <36 years compared to ≥36 years age group. Beta HCG and number of sacs did not differ between <36 years and ≥36 years age groups. The number of sacs formed and live birth were significantly more among frozen embryo. Day 5 embryo had significantly more positive rate of beta HCG, more number of sac formations, and live birth.
Conclusion:
The present study dictates that in vitro fertilization rate showed better success with women <36 years of age than >36 years old. Day 5 blastocysts had good implantation rates along with higher resulting pregnancy rates. The FET had better live birth rate.
Keywords
Beta HCG
frozen embryo transfer
IVF rate
INTRODUCTION
The prevalence of infertility is increasing in the current scenario. Apart from certain medical conditions, this could be attributed to couples prioritizing lifestyle and career over family planning.[1] At the same time with advancement in medical science, the options for infertility treatments are improving. However, maternal age is one of the most important factors affecting outcomes of in vitro fertilization (IVF) as it is well known that the fertility potential of women decreases with increasing age.
EFFECT OF MATERNAL AGE ON IVF OUTCOMES
There is a strong relationship between advanced maternal age, decreased ovarian reserve, and increased chromosomal abnormalities in the oocytes and the formation of aneuploid embryos with very low implantation rates.[2,3] Women of advanced age respond poorly to exogenous hormones thereby leading to retrieval of a lower number of competent oocytes.[4] An oocyte which is able to resume meiosis, get fertilized, create two pronuclei, and reach the blastocyst stage, implant, and result in a live birth, is considered to be a competent oocyte. It is well known that there are age-related changes in the molecular mechanisms involved in oogenesis and therefore result in poor quality oocytes. In addition, processes such as dysfunctional cohesins, shortening of telomeres, lowered surveillance of spindle-assembly checkpoints, impaired metabolic activity of the mitochondria leading to improper chromosomal segregation and therefore, impacting the competence of the embryo.
Moreover, advancing age cannot compensate for basic physiologic preconditions of reproductive senescence.[5] Hence, for a reproductive medicine specialist, it is essential to determine the day of embryo transfer (ET), to achieve favorable outcomes. Following IVF, ET is performed typically at the cleavage stage, on day 3 after fertilization or on day 5 after fertilization, that is, at the blastocyst stage, after morphologic assessment of the embryos. However, it has been shown that embryo morphology is not dependent on the age of the woman.[6,7] On the contrary, the age-related competence of an embryo is associated with increasing aneuploidy rate in the embryos.
Day 3 transfers
There is a great biologic variability in a woman’s hormonal response to quantity and quality of embryo number and development. For women who have few embryos, it is often better to do a day 3 transfer rather than “push” these few or suboptimal embryos to day 5 for a blast transfer; these embryos may “arrest” and so there may be no transfer on day 5. In addition, a day 3 transfer is more preferable as it allows the patient to get more than one chance of an ET as generally on day 3, there are more number of embryos available than on day 5. A day 3 transfer may also enhance the receptivity of the endometrium, as the chemokine receptors required for implantation are expressed only in the presence of an embryo, and transferring on day 3 may provide enough exposure to enhance the endometrial receptivity.
For an improved pregnancy rate, multiple embryos are transferred into the uterus, resulting in multiple pregnancies and other associated complications such as abortions and premature deliveries. Therefore, the American Society for Reproductive Medicine has formed guidelines for transferring no more that two to three embryos for women aged 35 to 37 years and three to four for women aged 38 to 40 years. Moreover, the adverse outcomes arising from twin pregnancies which may arise due to transferring multiple embryos have led the clinicians toward blastocysts transfers, which reduces the number of embryos being transferred.
Day 5 transfers
A blastocyst transfer is considered more beneficial, as it increases the chances of a successful pregnancy; however, the rate of blastocyst formation has been observed to reduce with increasing maternal age. In a naturally occurring pregnancy, the embryo is thought to traverse the uterotubal junction late on day 3 or early on day 4, and so transferring the embryo later may result in timing of exposure of the embryo to the uterine environment that is more analogous to a natural cycle.[8] There is an increase in the rate of implantation due to better endometrial synchronicity. Moreover, the activation of the genome at day 4 enables identification of embryos capable of forming blastocysts in vitro and enables selection of those with the highest implantation potential.[9,10,11] It also reduces the risk of multiple gestations as fewer blastocysts are transferred.
Despite the thought that the transfer of high-quality blastocysts will result in higher implantation rates,[12] give a better synchronization between the blastocyst and the endometrium,[13] and generate higher pregnancy and live birth rates in comparison with transfer of cleavage-stage embryos, there may be resulting complications such as higher incidence of monozygotic twinning rates[14]; risk of premature deliveries of babies with lower birth weights[15]; generation of epigenetic mutations in offspring[16]; and altered sex ratios.[13] Previous literature also suggests that the cumulative clinical pregnancy rate for cleavage-stage embryos is higher than that for blastocysts.[17]
Previous studies have also found that frozen thawed embryos tend to give better results. This may be due to the hormonal milieu being similar to that of a natural cycle as well as favors embryo-endometrial receptivity. However, adverse outcomes such as postpartum hemorrhage, macrosomia, and hypertensive disorders have also been found to be increased in FET. Therefore, in order for the clinician to give optimum result, it becomes important to decide the not only the day of transfer but also the ET should be performed in the next cycle.
The aim of this retrospective prospective study is to compare the reproductive outcomes (implantation rate, pregnancy rate) between day 3 and day 5 transfers in two different age groups of patients (aged <36 years vs. aged ≥36 years). Additionally, quality of embryo will also be evaluated, with respect to fresh ET or freeze-all ET strategy. The study results should provide valuable information to clinicians in making better decisions about selection of appropriate day of ET in these patients.
Advanced female age is associated with increased incidence of infertility and pregnancy loss, as well as decreased success of assisted reproductive technology (ART). The reason lies in both quantitative and qualitative declines in ovarian reserve. The use of new sequential culture media for production of blastocysts has high viability as evidenced by an implantation rate of 50% and a pregnancy rate of 65% post ET at blastocyst stage.[12] ET is a crucial step in IVF and a great challenge for desired outcomes is selecting the day of transfer. Many studies were conducted to find out whether ET at day 3 or day 5 gives the best clinical results in advanced aged females.
In a randomized prospective study by Kaur et al., the efficacy of blastocyst transfer in comparison with cleavage-stage transfer was studied in 300 females aged 25 to 40 years undergoing IVF/intracytoplasmic sperm injection (ICSI) cycle in an infertility center in Jaipur, India. They found that clinical pregnancies were significantly higher after blastocyst transfer compared to cleavage-stage ET (44.0% vs. 29.33%; P < 0.01). Implantation rate for blastocyst transfer group was also significantly higher (P < 0.001). The study concluded that in females with advanced age groups, blastocyst transfer is having higher implantation rate and clinical pregnancy rate.[18]
Sotiroska et al. conducted a prospective study to compare the reproductive outcomes between the transfer of cleavage-stage embryos and blastocysts in two different age groups: age <36 years (group 1) and aged ≥36 years (group 2). These groups subdivided according to the day of ET: day 3 (ET3) and day 5 (ET5). In both age groups, transfer of blastocysts resulted in a higher clinical pregnancy rate and deliveries. An increased twin birth rate was observed in patients younger than 36 years on both transfer days compared with ≥36 years of age. Monozygotic twins rate were observed only among younger patients (<36 years), specifically on ET5 compared with ET3. No significant difference noted in mean birth weight of single and twins between ET3 and ET5 subgroups in younger age group of patients except for the triplets who were significantly heavier in the ET5 group compared with the older group (>36 years). This study indicates that if blastocyst can be obtained in patients of advanced age (>36 years), it improves their baby take-home rates. Younger patients (36 years) should undergo elective single blastocyst transfers to reduce multiple pregnancy rates.[19]
A similar study was conducted by Chang et al. to compare the clinical pregnancy rates in women with advanced pregnancy age (≥40 years) after ET at day 3 or day 5 of embryo culture. Out of 251 women, 141 had ET after day 3 of embryo culture, among which 26.4% had clinical pregnancy and 111 cycles had ET after day 5, out of which 40.9% had clinical pregnancy. The study reported that high clinical pregnancy rates are achievable after day 5 of ET in women of advanced maternal age.[20]
Early positive results for FET led to a shift to a “freeze-all” ET strategy than fresh ET. Studies showed that FET significant improvements in terms of implantation rates and clinical and ongoing pregnancy rates.[21,22] In a prospective study, Zhou et al. analyzed the optimal FET strategy in young and advanced age women who underwent IVF. Two FET strategies were studied: strategy A − transfer of thawed cleavage-stage embryos and strategy B − blastocysts cultured from thawed cleavage-stage embryos. The clinical and neonatal outcomes of two FET strategies were compared in young (<35 years) and advanced (>35 years) age women. They found in young age, the clinical outcomes per transfer cycle were better in strategy B than strategy A. As the clinical pregnancy and live births per thaw cycle were significantly higher in strategy A than in strategy B. In advanced age, the clinical outcomes per transfer cycle were better in strategy B and clinical pregnancy and live birth rates per thaw cycle were significantly higher in strategy B than in strategy A.[23]On the contrary, a retrospective study of 882 women aged 20 to 44 years undergoing their first or second IVF/ICSI cycle showed that there was no benefit on live birth rate of freeze-all versus fresh transfer in normo-ovulatory women undergoing IVF.[24]
Therefore, more studies are required to find out whether maternal age has impact on day 3 versus day 5 transfer. Additionally, the importance of freeze-all ET needs to be validated in comparison to fresh ET.
LACUNAE IN LITERATURE
There is a gap in the knowledge about the impact of maternal age on ET. Number of studies has been conducted around the world but no conclusive results for the clinician are yet available. The reason for this can be small sample size and lack of evaluation of data with respect to all the clinical outcomes of pregnancy post IVF.
Duration of study: prospective − September 2020 to February 2021; retrospective − September 2019 to February 2020
Sample size: prospective − 82; retrospective − 83
Inclusion criteria: tubal infertility, unexplained infertility, anovulation, mild male factor, no uterine anomaly
Exclusion criteria: SOATS, donor cycles/surrogates cycle, endometrium <7 mm, cycles undergoing PGT-A, adenomyosis, infections
Demographic and cycle characteristics of female patients at ET3 and ET5: age, primary/secondary infertility, history/previous ART failure, body mass index, anti-Müllerian hormone, antral follicle count, follicle-stimulating hormone, E2, number of oocytes retrieved, grading of embryos (as per Istanbul consensus), number of embryos transferred (fresh/frozen), implantation rate, clinical outcome
PATIENT STIMULATION AND OOCYTE RETRIEVAL
Ovarian stimulation will be achieved by using Gonal.F (Merck Serono, Darmstadt, Germany)/HMG (Bharat Serum). Pituitary suppression will be achieved by cetrorelix (German Remedies) as a subcutaneous injection at 0.25 mg/day when the largest follicle will reach a diameter of 14 mm (antagonist flexible cycle).
When the largest follicles reach a diameter of 18 to 20 mm, a subcutaneous injection of 10,000 IU of human chorionic gonadotropin (Lupin) or injection Lupride 1 mg (Sun Pharma) will be given as a trigger. Oocyte retrieval will be performed by transvaginal ultrasound-guided (GE Healthcare) follicle aspiration under GA using Cook aspiration needle and suction pump (kraft) 34 to 36 hours after the trigger.
OOCYTE INSEMINATION AND EMBRYO CULTURE
After aspiration, the oocyte–cumulus complex will be collected into GMOPS Plus medium (Vitrolife, Sweden), washed and incubated in GIVF Plus medium (vitrolife, USA) for 3 to 4 hours before insemination by IVF/ICSI. For ICSI, denudation of oocytes will be performed using Hyaluronidase (Sage) and cultured in G1Plus medium. Embryo culture will be performed in 20 μL drops of G1Plus culture medium under Ovoil in an atmosphere of 6% CO2 in air at 37°C. On day 3, embryos will be transferred to G2Plus medium for blast culture, in case day 5 transfer.
Pronuclear formation evaluation 16 to 18 hours after insemination and only zygotes displaying two pronuclei will be selected for culture.
Embryo grading will be carried out according to Istanbul Consensus.
Grading will be given to score and select embryos for transfer and cryopreservation according to the factors observed in the embryo. Cryopreservation will be carried out using Origio vitrification cooling kit.
EMBRYO TRANSFER
Transfer of one or two embryos will be the routine of this study in blastocyst stage but if not good-grade embryos available, more than two embryos can be transferred at cleavage stage. Transfer will be performed conducted by two-bubble method using Cook catheter in G2Plus medium (Vitrolife).
For frozen ETs (FETs), day 3 embryos will be thawed using Origio Vitrification warming kit. For day 3 transfer, ET will be carried out on the same day. For day 5 transfer, embryos will be cultured further for 2 days and then the transfer will be carried out [Figure 1].
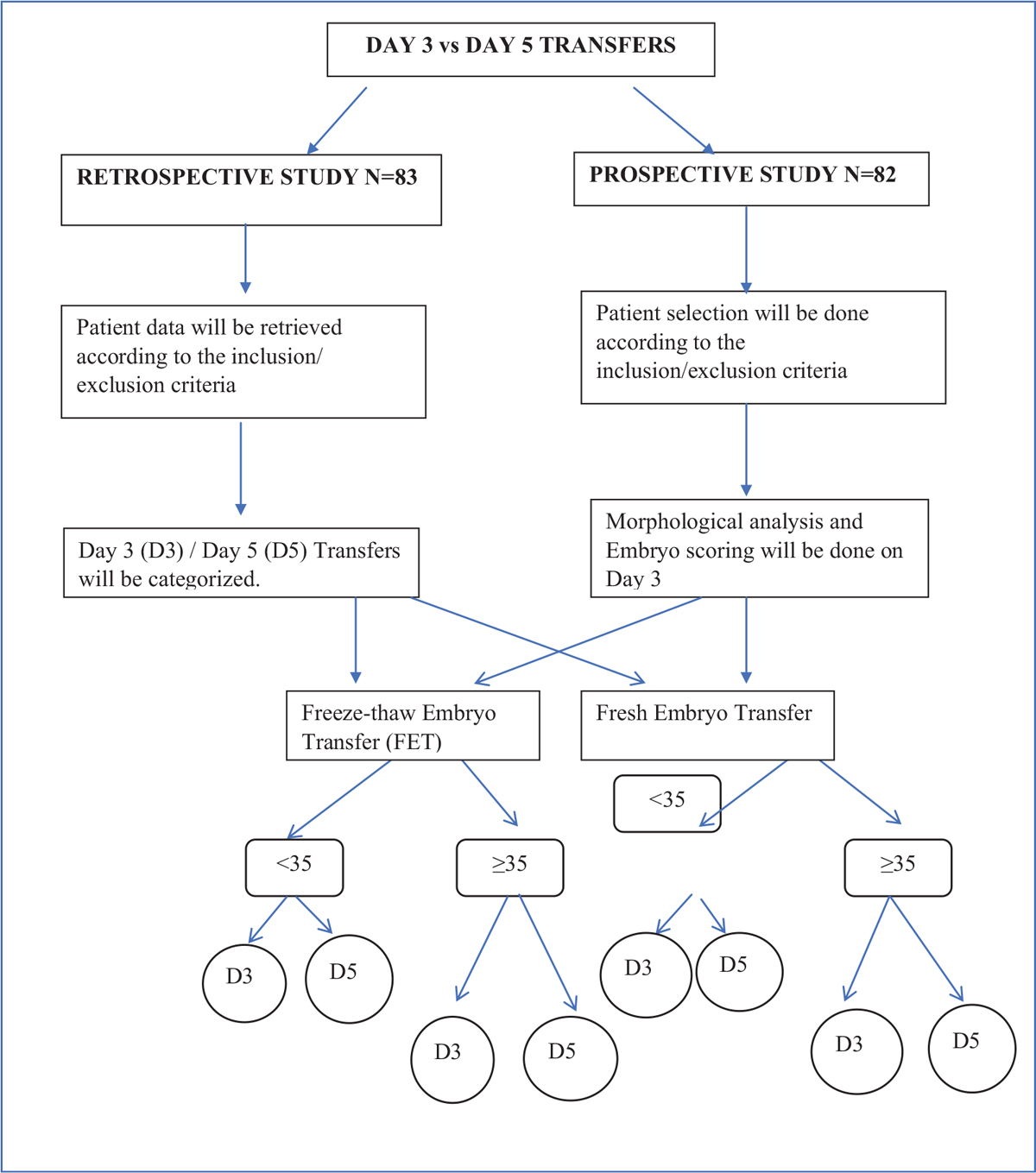
- Methodology flowchart.
OUTCOME MEASURES
Primary outcome
Implantation rate: The number of gestational sac/number of transferred embryos observed on TVS 3 to 5 weeks after transfer.
Clinical pregnancy rate: Defined as the presence of the gestational sac with a fetal pole with cardiac activity on transvaginal ultrasound at 6 weeks.
Secondary outcome
Fertilization rate: It is the percentage of eggs fertilized out of eggs inseminated or injected.
Cleavage rate: total number of day 3 embryos by total number of fertilized oocytes.
Multiple pregnancy rates
Mean number of embryos/blastocysts transferred
Biochemical pregnancy
Ectopic pregnancy
Miscarriages
Live births
For tests of association using bivariate correlations, a moderate correlation between maternal age on implantation and clinical pregnancy rates in patients undergoing day 3 versus day 5 ET will be considered meaningful. To detect a moderate correlation (r = 0.25), a sample of 165 analyzable subjects will provide 90% power to discover that the correlation is significantly different from there being no correlation (i.e., that the correlation would be 0) at the 0.05 level.
Formula used
N = [(Zα + Zβ)/C]2 + 3
where
The standard normal deviate for α = Zα =1.96 The standard normal deviate for β = Zβ =1.282C = 0.5 * ln[(1 + r)/(1−r)]
= 0.5 * ln[1.25/0.75]
= 0.5 * 0.511
= 0.255
N = [(1.96 + 1.282)/0.255]2 + 3
= [3.242/0.255]2 + 3
= 161.11 + 3
= 164.11
Statistical methods
Categorical variables will be presented in number and percentage and continuous variables will be presented as mean ± standard deviation and median. Normality of data will be tested by Shapiro–Wilk test. If the normality is rejected, then nonparametric test will be used. Quantitative variables will be compared using paired t test/Wilcoxon test (when the data sets were not normally distributed) for pre- to postvalues. A P-value of <0.05 will be considered statistically significant. Normally distributed continuous variables will be compared between the groups (freeze and fresh) using the unpaired t test, whereas the Mann–Whitney U test will be used for those variables that were not normally distributed. The data will be entered in MS EXCEL spreadsheet and analysis will be performed using Statistical Package for Social Sciences version 21.0 (SPSS-IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp. IBM Corp. Released 2013).
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- International estimates of infertility prevalence and treatment-seeking: potential need and demand for infertility medical care. Hum Reprod. 2007;22:1506-12.
- [Google Scholar]
- Serum anti-Müllerian hormone levels reflect the size of the primordial follicle pool in mice. Endocrinology. 2006;147:3228-34.
- [Google Scholar]
- Age is a better predictor of pregnancy potential than basal follicle-stimulating hormone levels in women undergoing in vitro fertilization. Fertil Steril. 2003;79:63-8.
- [Google Scholar]
- The relevance of age in female human reproduction-current situation in Switzerland and pathophysiological background from a comparative perspective. Gen Comp Endocrinol. 2013;188:166-74.
- [Google Scholar]
- Extended culture up to the blastocyst stage: a strategy to avoid multiple pregnancies in assisted reproductive technologies. Biol Res. 2011;44:195-9.
- [Google Scholar]
- Impact of day 3 or day 5 embryo transfer on pregnancy rates and multiple gestations. Fertil Steril. 2009;91:1717-20.
- [Google Scholar]
- Day three versus day two embryo transfer following in vitro fertilization or intracytoplasmic sperm injection. Cochrane Database Syst Rev 2004:CD004378.
- [Google Scholar]
- High outcome predictability after IVF using a combined score for zygote and embryo morphology and growth rate. Hum Reprod. 2002;17:2402-9.
- [Google Scholar]
- Morphological systems of human embryo assessment and clinical evidence. Reprod Biomed Online. 2013;26:210-21.
- [Google Scholar]
- Day 3 and day 5 morphological predictors of embryo viability. Reprod Biomed Online. 2003;6:323-31.
- [Google Scholar]
- A prospective randomized trial of blastocyst culture and transfer in in vitro fertilization. Hum Reprod. 1998;13:3434-40.
- [Google Scholar]
- Impact of blastocyst transfer on offspring sex ratio and the monozygotic twinning rate: a systematic review and meta-analysis. Fertil Steril. 2009;91:2381-90.
- [Google Scholar]
- Practice Committee of the Society for Assisted Reproductive Technology Blastocyst culture and transfer in clinical-assisted reproduction. Fertil Steril. 2006;86:S89-92.
- [Google Scholar]
- IVF Directors Group of Canadian Fertility and Andrology Society. Increased risk of preterm birth in singleton pregnancies after blastocyst versus Day 3 embryo transfer: Canadian ART Register (CARTR) analysis. Hum Reprod. 2013;28:924-8.
- [Google Scholar]
- Epigenetics and assisted reproductive technology: a call for investigation. Am J Hum Genet. 2004;74:599-609.
- [Google Scholar]
- Cleavage stage versus blastocyst stage embryo transfer in assisted reproductive technology. Cochrane Database Syst Rev. 2012;7:CD002118.
- [Google Scholar]
- A comparative study between cleavage stage embryo transfer at day 3 and blastocyst stage transfer at day 5 in in- vitro fertilization/intra-cytoplasmic sperm injection on clinical pregnancy rates. J Hum Reprod Sci. 2014;7:194-7.
- [Google Scholar]
- The day of embryo transfer affects delivery rate, birth weights, female-to-male ratio, and monozygotic twin rate. Taiwan J Obstet Gynecol. 2015;54:716-21.
- [Google Scholar]
- Day 3 versus day 5 embryo transfer in women of advanced maternal age. Fertil Steril. 2010;93:S10.
- [Google Scholar]
- Fresh versus elective frozen embryo transfer in IVF/ICSI cycles: a systematic review and meta-analysis of reproductive outcomes. Hum Reprod Update. 2019;25:2-14.
- [Google Scholar]
- Evidence of impaired endometrial receptivity after ovarian stimulation for in vitro fertilization: a prospective randomized trial comparing fresh and frozen-thawed embryo transfer in normal responders. Fertil Steril. 2011;96:344-8.
- [Google Scholar]
- Clinical and neonatal outcomes of patients of different ages following transfer of thawed cleavage embryos and blastocysts cultured from thawed cleavage-stage embryos. PLoS One. 2018;13:e0207340.
- [Google Scholar]
- Elective frozen embryo transfer does not improve reproductive outcome in normo-responder patients. Hum Reprod. 2015;30:i112-3.
- [Google Scholar]







