Translate this page into:
Oocyte recovery rates in flushing versus nonflushing during oocyte retrieval in assisted reproductive techniques
Address for correspondence: Prof Abha Majumdar and Dr Shweta Mittal Gupta, Center of IVF and Human Reproduction, Sir Ganga Ram Hospital, New Delhi- 110027, India. E-mails: abhamajumdar@hotmail.com; mshwets@hotmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Follicular aspiration under transvaginal ultrasound guidance is performed as part of assisted reproductive technology (ART) to retrieve oocytes for in vitro fertilization (IVF). However, controversy as to whether follicular flushing following aspiration yields a larger number of oocytes than aspiration only is ongoing. The aim of this study was to assess the safety and efficacy (oocyte recovery rates) of follicular flushing when compared with aspiration only performed in women undergoing ART. The study was conducted at Sir Gangaram Hospital, New Delhi. Retrospective data of 100 females undergoing ART was taken from September 2019 to September 2020. Patients were divided into two groups of 50 each. In first group, patients underwent oocyte retrieval using double lumen needle (flushing technique) and in the second group, single lumen needle (no flushing) were used. Females with age ≤37 years who were having ≤9 follicles, size ≥14 mm during oocyte retrieval when undergoing ARTs. Categorical variables were presented in number and percentage (%) and continuous variables, as mean ± standard deviation and median. Normality of data was tested by Kolmogorov–Smirnov test. If the normality was rejected, then nonparametric test was used. Quantitative variables were compared using Mann–Whitney test. Follicular flushing had significantly better oocyte recovery rates when compared with no flushing (P < 0.05). There was no significant difference (P > 0.05) in M2 rates in patients undergoing intracytoplasmic sperm injection (ICSI) when compared in both the groups. There was no significant difference (P > 0.05) in fertilization rates in patients undergoing IVF and ICSI, respectively, in both the groups. Double lumen needle with flushing technique gives better oocyte recovery rates in low responder women undergoing ARTs. Hence, follicular flushing may be considered in such patients for oocyte retrieval.
Keywords
ART
COS
flushing
nonflushing
oocytes
INTRODUCTION
Follicular aspiration under transvaginal ultrasound guidance is performed as part of assisted reproductive technology (ART) to retrieve oocytes for in vitro fertilization (IVF). However, controversy as to whether follicular flushing following aspiration yields a larger number of oocytes than aspiration only is ongoing. Flushing of follicles was a routine procedure in IVF treatments at the beginning of ultrasound-guided follicular aspiration.[1] The purpose of the flushing procedure was to increase oocyte yield, possibly by improved detachment of the cumulus–oocyte complex (COC) from the follicular wall. However, several studies have shown that follicular flushing neither increased oocyte yield nor pregnancy rate per cycle, in patients with a normal response to gonadotropin stimulation.[2] However, in poor responder patients, the benefit of follicular flushing has been a subject of controversy.[3] One randomized controlled trial (RCT) has reported increased oocyte yield following follicular flushing in poor responders.[4] On the contrary, another study has found no benefits of follicular flushing for increasing oocyte yield.[5] Nevertheless, various studies have suggested that the number of oocytes is an important prognostic variable for IVF success, that is, live-birth rate (LBR), hence the need to retrieve maximum oocytes during IVF.[6,7] Therefore, we undertook this study to evaluate the benefit of flushing, if any, on oocyte yield.
The aim of the study was to assess the efficacy (oocyte recovery rates) of follicular flushing when compared with aspiration only in low responder women undergoing controlled ovarian stimulation (COS) during ARTs.
MATERIALS AND METHODS
The study was conducted at Centre of IVF & Human Reproduction, Sir Gangaram Hospital, New Delhi. It was a retrospective observational study. The study included patients undergoing COS with IVF from September 2019 to September 2020. Total 671 patients underwent COS with IVF during this period. After fulfilling the selection criteria, the first 50 low responders who underwent oocyte retrieval using no follicular flushing technique (with single lumen needle) formed the first group and the first 50 low responders who underwent oocyte retrieval using follicular flushing technique (with double lumen needle), formed the second group. In flushing technique, follicles were flushed with 1 ml media after aspiration and the media was reaspirated. Normally single lumen needle is used for oocyte retrieval at our center, but in poor responders double lumen needle is used for flushing follicles. The data of these 100 patients were analyzed in the study. In the first group, 33 patients underwent intracytoplasmic sperm injection (ICSI) and 17 patients underwent IVF. In the second group, 31 patients underwent ICSI and 19 patients underwent IVF.
Selection criteria
Females with age ≤37 years, having ≤9 follicles ≥14 mm during oocyte retrieval while undergoing ARTs.
Exclusion criteria
Females >37 years of age and females showing normal response to COS during IVF.
Statistics
Categorical variables were presented in number and percentage (%) and continuous variables were presented as mean ± standard deviation and median. Normality of data was tested by Kolmogorov–Smirnov test. If the normality was rejected, then nonparametric test was used. Quantitative variables were compared using Mann–Whitney test (as the data sets were not normally distributed) between the two groups. A P-value of <0.05 was considered statistically significant. The data were entered in MS EXCEL spreadsheet and analysis was carried out using Statistical Package for Social Sciences (SPSS) version 21.0 (Statistical package for social sciences (SPSS) software, IBM manufacturers, Chicago, USA).
Outcomes
Primary outcome measures: oocyte recovery rates.
Secondary outcomes measures: M2 rates, fertilization rates in IVF and ICSI.
Oocyte recovery rate (%) = Number of oocytes/Numbers of aspirated follicles × 100
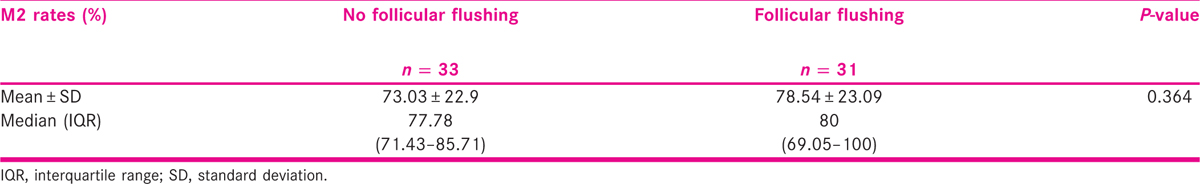
M2 rates (%) = M2 oocytes/Total retrieved oocytes × 100
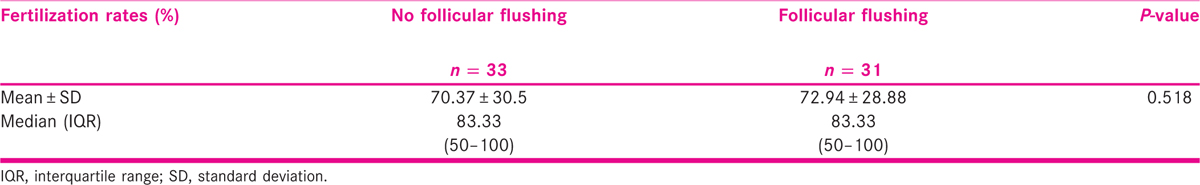
Fertilization rate in IVF (%) = Total 2 pronuclei (pn)/Total retrieved oocytes × 100
Fertilization rate in ICSI (%) = Total 2 pn/Total injected oocytes × 100
RESULTS
Tables 1-4 illustrate that oocyte recovery rates were significantly better when flushing technique was used when compared with nonflushing during oocyte retrieval. There was no statistically significant difference in M2 rates, fertilization rates in IVF, and fertilization rates in ICSI.


DISCUSSION
In our study, it was observed that flushing improved oocyte yield in low responder women undergoing COS during IVF. In low responders, even a single oocyte is precious. Flushing helps in detachment of COC from follicular wall. Hence, no follicle is left wasted.
One RCT demonstrated that this approach did not improve oocyte yield instead led to a 32% longer operation time.[8] Two other RCTs were also consistent with the above study, as none of these found an increased oocyte yield by flushing the follicles.[4,9] Cochrane review[10] also supports the above findings. In contrast, two large retrospective studies revealed a higher number of oocytes if follicles were flushed.[11,12] One RCT concluded that flushing of follicles at the time of oocyte retrieval was of benefit in women with poor response to controlled ovarian stimulation (COS) in terms of higher number of oocyte recovery and therefore a greater number of embryos available for transfer. Even though the procedure and anesthesia time were longer, it was worth flushing follicles in women with poor response to COS for better LBRs and significantly improved clinical pregnancy rates.[13] In yet another study, it was seen that age adjusted cumulative LBR (CLBR) was strongly influenced by oocyte number, with CLBR significantly increasing with increase in oocyte yield. To increase LBR/CLBR, we need to maximize the number of oocytes.[14] Considering oocyte numbers as an important marker for IVF outcomes, flushing is a simple and effective technique to increase oocyte yield especially in poor responders.
Limitation
The M2 rates were calculated only in ICSI cycles. The study had a small sample size and it was a retrospective study.
CONCLUSION
To conclude, it appears that flushing increases oocyte yield in low responder women undergoing COS for IVF and can be considered in these women as a reasonable method for better oocyte yield.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- A prospective study to investigate the value of flushing follicles during transvaginal ultrasound-directed follicle aspiration. Fertil Steril. 1992;57:221-3.
- [Google Scholar]
- Follicular flushing during oocyte retrieval in assisted reproductive techniques. Cochrane Database Syst Rev. 2018;26(4):CD004634.
- [Google Scholar]
- ESHRE consensus on the definition of “poor response” to ovarian stimulation for in vitro fertilization: the Bologna criteria. Hum Reprod. 2011;26:1616-24.
- [Google Scholar]
- Follicular flushing and in vitro fertilization outcomes in the poorest responders: a randomized controlled trial. Hum Reprod. 2013;28:2990-5.
- [Google Scholar]
- Ovarian follicular flushing among low-responding patients undergoing assisted reproductive technology. Fertil Steril. 2009;91(suppl 4):1381-4.
- [Google Scholar]
- Association between the number of eggs and live birth in IVF treatment: an analysis of 400 135 treatment cycles. Hum Reprod. 2011;26:1768-74.
- [Google Scholar]
- Oocyte number as a predictor for ovarian hyperstimulation syndrome and live birth: an analysis of 256, 381 in vitro fertilization cycles. Fertil Steril. 2014;101:967-73.
- [Google Scholar]
- Direct aspiration versus follicular flushing in poor responders undergoing intracytoplasmic sperm injection: a randomised controlled trial. BJOG. 2017;124:1190-6.
- [Google Scholar]
- Randomized, open trial comparing a modified double-lumen needle follicular flushing system with a single-lumen aspiration needle in IVF patients with poor ovarian response. Hum Reprod. 2017;32:832-5.
- [Google Scholar]
- Follicular flushing in patients with poor ovarian response: a systematic review and meta-analysis. Reprod Biomed Online. 2018;36:408-15.
- [Google Scholar]
- Effect of follicular flushing on reproductive outcomes in patients with poor ovarian response undergoing assisted reproductive technology. J Assist Reprod Genet. 2017;34:1353-7.
- [Google Scholar]
- Follicular flushing increases the number of oocytes retrieved in poor ovarian responders undergoing in vitro fertilization: a retrospective cohort study. BMC Womens Health. 2018;18:186.
- [Google Scholar]
- To flush or not to flush: a randomized controlled trial comparing follicular flushing and direct aspiration at oocyte retrieval in poor responders undergoing IVF. Fertil Steril. 2017;108:e237-8.
- [Google Scholar]
- Live birth and perinatal outcomes following stimulated and unstimulated IVF: analysis of over two decades of a nationwide data. Hum Reprod. 2016;31:2261-7.
- [Google Scholar]







