Translate this page into:
Pregnancy outcome after endometrial scratching in intrauterine insemination: A randomized controlled trial
Address for correspondence: Priyanka Singh, Department of Obstetrics & Gynecology, JN Medical College, Aligarh Muslim University, Aligarh, Uttar Pradesh, India. E-mail: priyankasinghbi@gmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objective:
To study the effect of local endometrial scratching on the outcomes of intrauterine insemination cycle.
Design:
Randomized controlled trial.
Study setting:
Department of Obstetrics & Gynecology, JN Medical College, Aligarh Muslim University, Aligarh.
Materials and methods:
A total of 77 patients were enrolled in the study. Patients undergoing controlled ovarian stimulation with intrauterine insemination were randomly allocated in two groups. In group A (n = 31), endometrial scratching was carried out on D8/D9 of same menstrual cycle in which intrauterine uterine insemination (IUI) was performed and in group B (control group; n = 31), endometrial scratching was not performed. Primary outcome was measured by pregnancy rate, while secondary outcome was measured by endometrial indices.
Results:
Pregnancy rate was 16.2% in group A in which endometrial scratching was carried out in IUI cycle, whereas in group B, pregnancy rate was 9.6%. Although in group A, pregnancy rate was higher when compared with group B, the results were not statistically significant (P > 0.05). The mean endometrial thickness of women in group A was 9.329 ± 0.934 which was significantly higher than endometrial thickness of group B, that is, 7.72 ± 2.0. In group A, greater number of women (41.93%, n = 13) had zone 3 endometrial flow than group B (19.35%, n = 6). However, the difference was not statistically significant (P > 0.05).
Conclusion:
Endometrial scratching in follicular phase in the same cycle of stimulation with IUI gives better pregnancy rate in comparison with IUI without endometrial scratching. However, the results can be of proven clinical significance only if larger group of population is studied.
Keywords
Endometrial scratching
intrauterine insemination
controlled ovarian stimulation
INTRODUCTION
Endometrium is a complex tissue consisting of distinct cellular compartment including epithelial cells, endothelial cells, stromal cells, and leukocytes. It is also a dynamic tissue which undergoes a series of morphological, biochemical, and molecular changes during the menstrual cycle. It provides an optimum environment for opposition, attachment, and invasion of embryo during a defined implantation window period for establishing pregnancy.[1]
Implantation is the rate limiting step in natural pregnancies as well as in artificial reproductive techniques. About 75% of pregnancies are lost soon after conception, implicating either the implantation failure or early embryopathy.[2] The causes for repeated implantation failure may be reduced endometrial receptivity, embryonic defects, or multifactorial. Various uterine pathologies, such as thin endometrium, altered expression of adhesive molecules, and immunological factors may decrease endometrial receptivity, whereas genetic abnormalities of male and female, sperm defects, embryonic aneuploidy, or zona hardening are among the embryonic reasons for failure of implantation.[3]
The opposition and attachment process of embryo to the endometrium are the primary stages of implantation. Following which, there is subsequent invasion into the stroma of uterine wall. It is a complex and multistage process involving several cytokines and growth factors as well as synchronization between the embryonic tissue and endometrium.[4] Implantation is affected by receptivity of endometrium and interaction between endometrium and embryo. Receptivity of endometrium depends on estrogen and progesterone.[5] Endometrial receptivity is a time period in which the endometrium becomes capable of receiving and adhering the human embryo.[3,4] This endometrial receptivity is usually limited to 19 to 24 days of menstrual cycle.[6]. Uterine receptivity is enhanced by local endometrial injury which facilitates the embryo implantation. Endometrial injury before in vitro fertilization (IVF) among women with previous repeated IVF failures is associated with increased rates of implantation, clinical pregnancy, and live birth.[7]
The present study was planned to see the effect of local endometrial injury on pregnancy rate in intrauterine insemination.
MATERIALS AND METHODS
This is a randomized controlled trial conducted in the outpatient department (OPD) and fertility clinic of Department of Obstetrics and Gynecology of Jawaharlal Nehru Medical College and Hospital, Aligarh Muslim University (AMU) Aligarh from November 2015 to November 2017. Approval was taken from the ethical committee of the institution (document attached). It has also been registered under Clinical Trial Registry India.
Inclusion criteria:
Below 40 years of age
Body mass index (BMI) less than 35 kg/m2
Bilateral/unilateral tubal patency
Mild male factor subfertility: sperm count >5×106/ml motility >10%
Exclusion criteria:
Women above 40 years of age
BMI more than 35 kg/m2
Bilateral tubal blockage
Severe medical disorder
Severe male factor subfertility: sperm count <5×106/ml and motility <10%
Patients were recruited from gynecology OPD and fertility clinic. Initial infertility evaluation including complete detailed history, examination, and relevant investigations was carried out in all patients. Consent was taken from all the patients who were fulfilling the inclusion criteria, and the patients were divided into two groups through computer-based randomization.
Group A: Patients who underwent endometrial scratching on day 8 of menstrual cycle of intrauterine uterine insemination (IUI).
Group B: Patients who did not undergo endometrial scratching in IUI cycle.
Day 2 antral follicle count was carried out and dose of Clomiphene was decided according to ovarian reserve. Controlled ovarian hyperstimulation was started with tablet Clomiphene citrate, administered orally from day 2 to day 6 of the cycle. On day 8/9, transvaginal sonography was performed to monitor the follicular response to therapy and according to the response gonadotropin was added. On the same day, in group A, endometrial scratching was carried out with pipelle. The procedure was carried out with all aseptic precautions. Folliculometry was carried out from day 8/9 on alternate day. When the dominant follicle reached 18 mm and triple line preovulatory endometrial maturation with thickness >7 mm was present, then trigger was given with injection human chorionic gonadotropin (HCG) and IUI was carried out 34 to 36 h after HCG trigger.
On the day of IUI, the husband was instructed to give semen that was prepared by swim up technique or double density gradient method according to the semen parameters. After centrifugation of a semen sample in a discontinuous density gradient column, the total motile sperm count was obtained by multiplying the total sperm count by the prewash percentage of motility. The postwash sample parameters were assessed according to World Health Organization criteria.
All the women were provided with luteal phase support with natural micronized progesterone tablet Susten (manufactured by Sun Pharmaceutical Industries Limited, Chennai, Tamil Nadu, India) 200 mg per vaginum daily for 2 weeks. If the menstrual cycles were delayed, urine pregnancy test was carried out. When positive, a transvaginal ultrasound was performed 6 weeks later to confirm clinical pregnancy. The primary end point of this study was a positive urine pregnancy test.
Data were analyzed using the t test, Chi-squared test, and analysis of variance test. A P-value of <0.05 was considered statistically significant.
RESULTS
The basic demographic profile was comparable in both the groups. The prevalence of primary infertility was more than secondary infertility in both the groups. Maximum number of patients (61.29%, n = 38) were in the age group of 26 to 30 years and maximum number of them (74.19%, n = 46) presented within first 5 years of infertility.
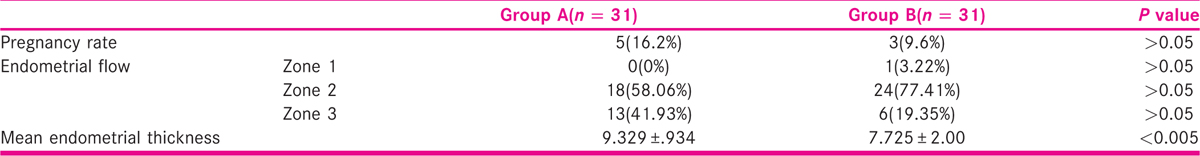
Pregnancy outcome
Pregnancy outcome was more in group A when compared with group B. Five women conceived in group A, whereas in group B, only three women conceived. Though more females conceived in group A, but the results were not statistically significant (χ2 = 0.574, P > 0.05).
Endometrial thickness
The mean value of endometrial thickness in group A was 9.329 ± 0.93 mm, which was higher than mean value of endometrial thickness (ET) in group B, that is, 7.725 ± 2.00 mm. There was a significant association between intervention and ET (60 = 15.94, P < 0.005).
Endometrial flow
Maximum number of patients (67.74%, n = 42) have zone 2 endometrial flow in both the groups. In group A, greater number of patients had zone 3 endometrial flow than group B. The difference between the groups was not statistically significant (χ2 = 4.436, P > 0.05) [Figure 1].

- Consort flow diagram.
DISCUSSION
Endometrial scratching has been suggested as one of the interventions to improve pregnancy outcome. In our study, mean ET was 9.32 ± 0.98 in group A, whereas in group B, it was 7.35 ± 0.512 mm. The difference between the two groups was highly significant. Similarly, in randomized control trial (RCT) conducted by Wadhwa et al.[8] Mean ET was 8.4 ± 1.84 mm and 7.4 ± 1.8 mm in endometrial biopsy group and control group, respectively. ET obtained on day of HCG trigger was significantly high in endometrial biopsy group (P = 0.002) [Tables 1 and 2].

Parsanezhad et al.[9] found mean ET to be 8.94 ± 1.21 mm in endometrial injury group and 9.18 ± 1.3 mm in control group which was also in agreement with our study.
Esmailzadeh and Faramarzi[10] found mean ET to be 10.1 ± 3.0 mm in women who achieved clinical pregnancy after IUI. In women who did not achieve clinical pregnancy mean ET was 7.7 ± 3.5 mm. They concluded that ET can be considered as a main predictor of pregnancy rate in IUI cycle.
In studies conducted by Inal et al.[11] and Soliman and Harira[12] the mean ET was higher in endometrial biopsy group than control group. This was in coherence with our study.
Possible explanation of this increase in pregnancy outcome may be endometrial decidualization, angiogenesis, and inflammatory mechanism induced by endometrial injury or scratching making the endometrium more receptive for implantation.
Pregnancy rate
Randomized controlled trial conducted by us showed that there was increase in pregnancy outcome in the patients which underwent endometrium scratching in IUI cycle than those in which scratching of endometrium was not carried out.
In our study, pregnancy rate was 16.12% in group A and 9.6% in group B (P < 0.05).
This was in agreement with the study conducted by Soliman and Harira[12] who evaluated the effect of endometrial scratching on fertility outcome. They observed clinical pregnancy rate of 22.6% versus 11.3% in the experimental group and control group, respectively (P = 0.02).
Similar to our study, Bahaa Eldin et al.[13] found clinical pregnancy rate of 18.93% in the experimental group and 7.42% in control group (P = 0.003). Salaheldin Abdelhamid[14] compared the fertility outcome after endometrial scratching in the cycle preceding IUI versus injury in the intervention cycle compared to classic IUI. They concluded that endometrial scratching increases pregnancy outcome when it is carried out in proliferative phase of same cycle, cycle preceding IUI cycle than pregnancy rates with IUI alone 36%, 38% versus 18%, respectively.
In the study conducted by Barash et al.,[15] 45 randomly selected patients underwent endometrial injury in IVF-ET. The rate of implantation, clinical pregnancy, and live birth in the endometrial injury group was 28%, 67%, and 49%, and in the control group was 14%, 30%, and 23%, respectively (P = 0.00009). They also postulated that endometrial injury promotes decidualization of endometrium making it more receptive for implantation.
Similarly, in study conducted by Raziel et al.,[16] clinical pregnancy rate was 30% in endometrial injury group versus 12% in control group (P = 0.02). In RCT conducted by Zhou et al.,[1] effect of endometrial injury on COS cycle and incidence of embryo implantation in IVF-ET was observed. There was significant increase clinical pregnancy rate, 66.7% in endometrial injury group versus 30.3% in control group (P = 0.00009).
In retrospective study by Nastri et al.,[17] the clinical pregnancy rate came out to be 49.4% in endometrial injury group versus 29.1% in control group (P = 0.01). Mooney et al.[18] found clinical pregnancy rate to be 71% in endometrial injury group versus 39% in control group.
Wadhwa et al.[8] conducted prospective randomized controlled study to see the effect local endometrial injury on IUI in COS cycle. They found clinical pregnancy rate of 31.11% in endometrial injury group versus 9.3% in control group (P<0.001).
Another randomized controlled trial conducted by Parsanezhad et al.[9] in which they induced local endometrial injury after COS during preovulatory days then followed regularly timed intercourse. They observed pregnancy rate of 14.9% versus 5.8% (P = 0.03) in endometrial injury group and control group, respectively.
Zarei et al.[6] found that application of local endometrial injury in the cycle before the IUI cycle is not associated with increased pregnancy rate. The clinical pregnancy rate was 13.5% in the endometrial injury group versus 13.3% in control group (P = 0.389) in their study.
Karimzade et al.[19] found negative impact of endometrial scratching on clinical pregnancy rate which was 12.3% in endometrial injury group versus 32.9% in control group (P<0.05). The conflicting result may be due to endometrial scratching on the day of oocyte retrieval, so there was no adequate for the tissue repair, gene transcription and for cytokine production which were required for implantation.
CONCLUSION
Endometrial scratching is a simple, low cost, and minimally invasive procedure that may enhance biochemical and clinical pregnancy rates. Endometrial tissue repair process following endometrial injury is mediated by expression of immunological factors by endometrial epithelial cells including adhesion molecules, cytokines, growth factors, and other immune mediators which are involved in implantation process. It also promotes decidualization of endometrium making it more receptive for implantation. Endometrial gene modulation following endometrial injury has also been hypothesized to increase endometrial receptivity.
In our study, there was significant increase in ET and blood flow following endometrial scratching which in turn resulted in improved pregnancy rates. In developing countries like India, endometrial scratching can prove itself beneficial as an affordable low-cost intervention. It can be carried out as an OPD procedure before ovulation induction and IUI, thereby improving pregnancy rates before proceeding for other high-cost alternative ART procedures.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Local injury to the endometrium in controlled ovarian hyperstimulation cycles improves implantation rates. Fertil Steril. 2008;89:1166-1176.
- [Google Scholar]
- Conception to ongoing pregnancy: the ‘black box’ of early pregnancy loss. Hum Reprod Update. 2002;8:333-343.
- [Google Scholar]
- Promoting implantation by local injury to the endometrium. Fertil Steril. 2010;94:2026-2029.
- [Google Scholar]
- Endometrial receptivity: clinical assessment in relation to fertility, infertility, and antifertility. Med Res Rev. 2006;26:699-746.
- [Google Scholar]
- The effects of endometrial injury on intrauterine insemination outcome: a randomized clinical trial. Iran J Reprod Med. 2014;12:649-652.
- [Google Scholar]
- Endometrial injury to overcome recurrent embryo implantation failure: a systematic review and meta-analysis. Reprod Biomed Online. 2012;25:561-571.
- [Google Scholar]
- Effect of endometrial biopsy on intrauterine insemination outcome in controlled ovarian stimulation cycle. J Hum Reprod Sci. 2015;8:151-158.
- [Google Scholar]
- Pregnancy rate after endometrial injury in couples with unexplained infertility: a randomized clinical trial. Iran J Reprod Med. 2013;11:869-874.
- [Google Scholar]
- Endometrial thickness and pregnancy outcome after intrauterine insemination. Fertil Steril. 2007;88:432-437.
- [Google Scholar]
- The effect of local injury to the endometrium for implantation and pregnancy rates in ICSI-ET cycles with implantation failure. Eur J Gen Med. 2012;9:223-9.
- [Google Scholar]
- Local endometrial scratching under ultrasound-guidance after failed intrauterine insemination and cycle outcome: a randomized controlled trial. Middle East Fertil Soc J. 2017;22:60-66.
- [Google Scholar]
- Endometrial injury may increase the pregnancy rate in patients undergoing intrauterine insemination: an interventional randomized clinical trial. Reprod Sci. 2016;23:1326-1331.
- [Google Scholar]
- The success rate of pregnancy in IUI cycles following endometrial sampling. A randomized controlled study. Arch Gynecol Obstet. 2013;288:673-678.
- [Google Scholar]
- Local injury to the endometrium doubles the incidence of successful pregnancies in patients undergoing in vitro fertilization. Fertil Steril. 2003;79:1317-1322.
- [Google Scholar]
- Favorable influence of local injury to the endometrium in intracytoplasmic sperm injection patients with high-order implantation failure. Fertil Steril. 2007;87:198-201.
- [Google Scholar]
- Endometrial injury in women undergoing assisted reproductive techniques. Cochrane Database Syst Rev 2015:CD009517.
- [Google Scholar]
- Effect of hysteroscopy performed in the cycle preceding controlled ovarian hyperstimulation on the outcome of in vitro fertilization. Fertil Steril. 2003;79(3):637-638.
- [Google Scholar]
- Local injury to the endometrium on the day of oocyte retrieval has a negative impact on implantation in assisted reproductive cycles: a randomized controlled trial. Arch Gynecol Obstet. 2010;281:499-503.
- [Google Scholar]







