Translate this page into:
To study the effect of autologous platelet-rich plasma instillation on suboptimal endometrium and pregnancy outcomes in infertile women undergoing frozen embryo transfer cycle
Address for correspondence: Dr R.K. Sharma, MD, Primus Super Specialty Hospital, Chandragupta Marg, Chanakyapuri, Delhi, India. e-mail: dr_sharma1957@yahoo.co.in
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
This pilot study was done to evaluate the effectiveness of intrauterineinstillation of autologous platelet rich plasma in the treatment of infertile woman with ≥2 IVF failures due to thin endometrium not responding to empirical medical therapies.
Design:
Prospective interventional study.
Material and Methods:
Intra uterine instillation of PRP was done in 50 women between 23 to 38 years with suboptimal endometrial receptivity, ≥ 2 IVF failures and HRT cycle cancellations over a course of 9 months. Frozen embryo transfer was done when optimal endometrial thickness and vascularity was achieved.
Results:
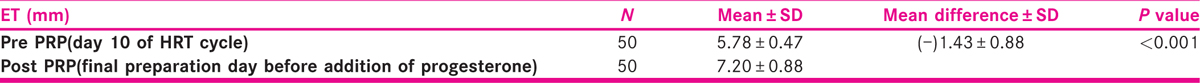
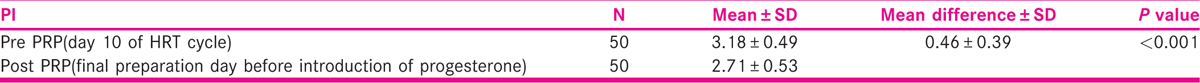
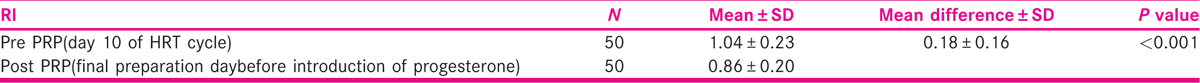
The mean endometrial thickness pre PRP was 5.78mm which increased to 7.20mm post-PRP (P value < 0.001). There was a statistically significant increase in endometrial vascularity. The mean PI uterine artery pre-PRP was 3.18 which decreased to 2.71 post PRP (P-value < 0.001). There was a statistically significant fall in uterine artery RI from 1.04 to 0.86 after PRP therapy. The implantation rate, clinical pregnancy rate were 15.3% & 33.3% respectively. One patient had early clinical pregnancy loss. Cervical ectopic pregnancy was diagnosed in 1 patient. 4 patients had DADC twins.
Conclusion:
PRP is a safe, inexpensive and acceptable alternative for endometrial preparation of infertile patients with ≥2 IVF failures due to suboptimal endometrium.
Keywords
Endometrial receptivity
frozen embryo transfer
PRP
thin endometrium
INTRODUCTION
Infertility is defined as failure to concieve after 1 year of unprotected intercourse in women < 35 years and 6 months in women >35 years.[1] Infertility is managed by medical, surgical measures or by assisted reproductive technology. In today’s era of ART, ovarian stimulation generates more embryos, which requires cryopreservation and subsequently thawed embryos are transferred. FET cycles give a contribution of 25% to ART births.[2] Successful embryo implantation in FET cycle requires superior quality embryos, favourable culture conditions, adequate endometrial receptivity & effective communication between embryo and endometrium. Endometrial receptivity is defined as a critical period when endometrium accepts blastocyst.[3] Ultrasound biophysical scoring inclusive of parameters like endometrial thickness, vascularity, uterine artery pulsitality and resistance index are the most important predictors of endometrial receptivity. Uterine artery RI < 0.9 is the most sensitive predictor for successful IVF outcome with diagnostic accuracy of 85%.[4]
HRT is preferred for endometrial preparation because of increased endometrial receptivity. Empirically many medications have been employed for improving endometrial thickness and vascularity in HRT cycles like exogenous estrogens,[5] low dose ecosprin,[6] argiprime, vaginal sildenafil,[7] vit E,[8] pentoxyfylline[9] and G-CSF.[10] But still some patients do not respond to these medications resulting in persistent thin endometrium. The reported incidence of thin endometrium in patients undergoing assisted reproductive technology is 2.4%.[11] This poses a major challenge in ART leading to cycle cancellations, lower implantation rates, lower clinical pregnancy rates and increased cost of ART.[12]
Intrauterine instillation of platelet-rich plasma has emerged as a contemporary therapy for endometrial regeneration in IVF cycles. PRP is defined as an autologous concentration of human platelets that is 3 to 5 times greater than physiological concentration of platelets in whole blood.[13] Platelet activation causes release of numerous growth factors like PDGF, EGF, VEGF, TGF and several other cytokines.[14] These factors promote chemotaxis, mesenchymal cell migration, proliferation, differentiation, extracellular matrix production and neoangiogenesis leading to endometrial tissue repair. PRP has been used for the treatment of nerve injury, tendinitis, arthritis, bone regeneration, cardiac muscle repair and plastic surgery. Intrauterine PRP is now used in treatment of refractory endometrium of infertile patients undergoing ART. It has been tried in cases of Ashermann syndrome, chronic endometritis, adenomyosis and other cases of recurrent implantation failure. But method of preparation is not standadarized. The effect of PRP on endometrial thickness, endometrial blood flows and putative molecular mechanisms are not clearly known. Knowledge of the identity, concentration, and discrete effects of the platelets will produce repeatable results in infertile patients. The results of this study will extrapolate the effect of platelet-rich plasma on endometrial receptivity and pregnancy outcomes up to 13 weeks in frozen embryo replacement cycle
MATERIAL AND METHODS
This prospective interventional study recruited 50 infertile patients attending our fertility centre from July 2019 to March 2020. The inclusion criteria were (1) age of 23-38 years, (2) ≥ 2 failed IVF cycles due to thin endometrium, (3) ≥2 cancelled HRT cycle due to thin endometrium (<7mm), (4) suboptimal endometrial receptivity. Suboptimal endometrial receptivity was identified as (i) endometrial thickness of <7mm despite standard dose of estradiol valerate (12mg/ day) on day 10 of FET cycle. (ii) Suboptimal endometrial vascularity. Suboptimal endometrial vascularity was defined as (a) <5 vascular signals reaching central zone (zone 3 and 4) of endometrium as measured by power doppler by the same observer on day 10 of the cycle, (b) Suboptimal uterine artery doppler indices : PI>3, RI >0.8. Exclusion criteria were (a) immunological disorders, (b) congenital or acquired abnormalities of uterus, (c) poor quality embryo, (d) parental genetic and chromosomal disorders, (e) hematological Disorders (Hb <9g%, platelet count <1,00,000), (f) uncontrolled endocrine disorders (g) medical conditions such as thyroid disorders, hyperprolactinemia.
Preparation of autologous PRP
PRP was prepared by drawing approx. 15 ml of blood into two collecting tubes, 7.5 ml each. This collecting tube was prefilled with 1.5ml of ACDA (Acid citrate dextrose anticoagulant) and centrifuged at 1600g for 10min. The blood was divided into 3 layers: red cell at the bottom, cellular plasma in supernatant and a buffy coat layer between them. The plasma and buffy coat layer were collected to another tube and recentrifuged at 3500g for 5 min. The resulting pellet of platelets was mixed with 1 ml of supernatant. This platelet-rich plasma was 4 to 5 times more concentrated.
FET cycle
Estrogen 12 mg/day was started from day 2 of the HRT cycle. On day 10 of HRT cycle, TVS was done using transvaginal probe of 7.5MHz. Endometrial thickness, endometrial vascularity and uterine artery doppler indices were noted. In patients with ET <7 mm on day 10 of HRT cycle, 0.5 ml of PRP was instilled into uterine cavity through IUI cannula under USG guidance within 1 hour of PRP preparation. Prophylactic antibiotics were given for 3 days to all the patients. Patient was asked to continue estrogen in same doses as before. TVS was repeated 72 hours later by the same observer. On day 13 of HRT cycle, ET, endometrial vascularity, uterine artery doppler indices PI and RI were noted. In patients with endometrial thickness ≥ 7mm, embryo transfer was done after 3 days of progesterone supplementation. In patients with ET <7mm, PRP was repeated. ET was measured after 72 hours. On day 16 of cycle, if ET was < 7 mm, cycle was cancelled. In patients with optimal ET ≥ 7 mm, embryo transfer was conducted after 3 days of progesterone administration. Appropriate luteal phase support was provided. Beta HCG was measured from peripheral blood 14 days later. Beta hcg > 50 IU/ml was considered to be positive.
The primary objective of the study was to measure change in the endometrial thickness and endometrial vascularity after PRP instillation. The variables (ET and endometrial vascularity) of recent cycle were compared with previous HRT cycles. The previous cycle acting as control. In the previous cycle, endometrial preparation was done with exogeneous estrogens. The outcomes were implantation rate, clinical pregnancy rate.
Data analysis
Statistical analysis was performed by the statistical package for the social sciences. Continous variables were presented as mean± SD, and categorical variables were presented as absolute numbers and percentage. Data were checked for normality before statistical analysis. Normally distributed continuous variables were compared from pre-post treatment using the paired t-test. Otherwise Wilcoxon signed rank test was used for non normally distributed data. Categorical variables were analyzed using either the chi-square test or Fisher’s exact test. P value< 0.05 was considered as statistically significant.
Ethics approval
The study was approved by IEC IFS.
RESULTS
39 of 50 recruited patients underwent embryo transfer. 3 patients had bleeding after intrauterine PRP instillation. In 8 patients, cycle was cancelled as optimal endometrial thickness of 7 mm was not achieved.
The mean age of patients was 33.28 years. The mean BMI was 25.14. The mean duration of infertility was 8.8 years. The mean number of failed IVF was 2.24. PRP was done once in 36 patients and twice in 14 patients. The mean platelet concentration pre-PRP was 2,58,000/cumm and mean platelet concentration post-PRP was 11,70,000/cumm.
The effect of PRP on endometrium is summarized in Tables 1-4. The mean endometrial thickness pre-PRP was 5.78 ± 0.47 mm. The mean endometrial thickness post-PRP was 7.20 ± 0.88 mm. The mean increase in endometrial thickness after PRP therapy was 1.43 ± 0.88 (P value < 0.001). 92% of patients had sparse vascularity pre PRP. 8% of patients displayed modest vascularity. After intrauterine PRP instillation, 64% of patients displayed excellent vascularity, 20% had modest vascularity and only 16% had sparse vascularity. In 3 patients, sparse vascularity improved to modest but embryo transfer was not done as endometrial thickness was <7mm. There was a statistically significant increase in endometrial vascularity after intrauterine PRP instillation (P value < 0.001). The mean uterine artery PI pre-PRP and post PRP was 3.18± 0.49 and 2.71± 0.53 respectively. There was a statistically significant reduction in pulsitality index after intrauterine PRP instillation (P value < 0.001). The mean uterine artery RI pre and post PRP was 1.04± 0.23 and 0.86± 0.20 respectively. There was a statistically significant reduction in uterine artery RI after intrauterine PRP instillation (P-value < 0.001).

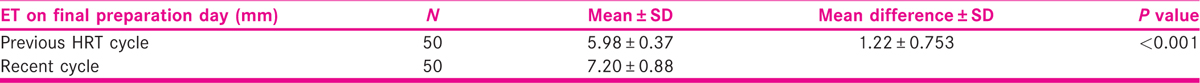
Comparision of recent cycle variables with previous cycle
Variables in recent and previous cycles are compared in Tables 5-7. In the recent cycle, the mean endometrial thickness on final preparation day was 7.20 ± 0.88 mm compared to 5.98 ± 0.37mm in previous cycle. There was a statistically significant difference in the endometrial thickness on final preparation day in between the two cycles (P value < 0.001). In recent cycle, endometrial vascularity was sparse in only 16% of patients compared to 40% in previous cycle. Endometrial vascularity on final endometrial preparation day was modest in 20% of patients in recent cycle compared to 60% in previous cycle. However, 64% of patients in recent cycle displayed excellent vascularity. No patient had excellent vascularity in previous cycle. There was a statistically significant difference in endometrial vascularity on final preparation day in between these two cycles (P value <0.001).


DISCUSSION
Chang et al.[15] were first to show promising role of PRP therapy in women with suboptimal endometrium undergoing IVF. He reported pregnancies in all 5 patients following PRP therapy.
Different authors have used different methods for preparing PRP. Higher centrifugation speeds lead to higher concentration of platelets which has paradoxical inhibitory effect on endometrium. So we used two-step centrifugation process. First centrifugation involoves 1600g for 10 minutes followed by 3500g for 5 minutes. Similar procedure was used by Eftekhar et al.[16] resulting in fraction of plasma with 4 to 5 times higher concentration of platelets.
There is a controversy regarding use of buffy coat rich in leukocytes. One school of thought says that leukocytes increases inflammation that can impede tissue rejuvination. On the other hand, inflammation fights infection and induces healing. In our study we are using L −PRP. Kim et al.[17] also advocated that leukocyte rich plasma improves implantation rate.
Since PRP is prepared from autologous blood, there is minimal risk of immunological reactions and infections.
Many studies showed positive effects of PRP therapy in patients with suboptimal endometrium, however change in endometrial thickness post PRP is variable (0.6-2.22mm). In 2019, Chang et al reported mean increase in endometrial thickness of 1.33mm (pvalue<0.05 at 95% confidence interval) after PRP therapy.[18] We used 0.5 ml of PRP for instillation into uterine cavity. Different studies have evaluated ET after 48 and 72 hours which does not appear to influence the end point.
In a recent study on 24 patients, Kim et al.[18] reported that an average increase in endometrial thickness after PRP therapy was 0.6mm (17). In our study mean increase in endometrial thickness after PRP instillation was 1.43mm. This difference may be due because the first study included patients with intrauterine adhesions in the study group. Patients with asherman have refractory endometrium which is nonresponsive to most of the medical therapies. Hence endometrial thickness didnot improve significantly after PRP therapy. These patients were excluded from our study. So endometrial thickness responded well to PRP therapy in our study.
Zadehmoddares[19] reported endometrial thickness of >7mm in all patients after PRP therapy. However in our study optimal endometrial thickness could be attained in only 78% of cases. This may be because the sample size in the first study was much smaller than our study.
Intrauterine PRP releases VEGF and other cytokines which acts on subendometrial microvasculature and promotes angiogenesis thereby improving endometrial receptivity. Subendometial blood flow study is simple, easy to perform and does not require much expertise. But weather subendometrial blood flow parameters are equally reliable and possibly more cost-effective tool to measure the effectiveness of intrauterine PRP, needs further studies.
Tandulwadkar et al performed intrauterine PRP instillation in 68 women between 22-40 years of age with ET< 7 mm and suboptimal endometrial blood flow.[20] On Power doppler, 4 patients continued to have poor endometrial vascularity after PRP therapy. In 47 patients, sparse vascularity improved to modest. 17 (25%) patients with sparse to modest vascularity showed excellent vascularity following PRP. In the present study, we found that 32 patients (64%) with sparse to modest vascularity displayed excellent vascularity following PRP instillation. In 8 (16%) patients, vascularity continued to be sparse. Thus, we observed a greater increase in endometrial vascularity after intrauterine PRP instillation. This may be attributed to younger population in our study group. Also we used a higher dose of progynova (12 mg) from day 2 of periods for endometrial preparation.
In 1995, Steer et al advocated that RIF may be due to lower uterine perfusion which can be detected by uterine artery pulsed wave doppler.[21] Uterine artery doppler is a more reliable and reproducible parameter to predict pregnancy. Our study is probably the first study to evaluate the effect of intrauterine instillation of autologous PRP on uterine artery doppler. In our study there was a significant decline in uterine artery impedance (P value <0.001) following PRP therapy. The pregnancy rate was 33.33%. But molecular mechanisms that contribute to the improvement in uterine perfusion are not clear. More studies are required to establish the use of uterine artery doppler indices to evaluate the effect of intrauterine PRP therapy in patients with RIF due to suboptimal endometrium.
Eftekhar et al.[16] reported an implantation rate of 21% after PRP therapy. However in our study, implantation rate was 15.3%. This may be due to differences in characteristics of included population groups. In the first study, the common etiology of infertility was male factor (32.5%) and unexplained infertility (35%). In these cases, implantation rates are higher during IVF. In contrast of this, our study group was inclusive of patients with tubal factor (44%) and PCOS (30%). PCOS patients have a higher BMI. Because of higher PCOS patients in our study, 52% of patients had BMI of ≥25 which may be contributory to decreased implantation. Also, recurrent implantation failures were the main inclusion criteria of our study but not so in the first study. Hence, implantation rates are not comparable. Madhavan et al reported pregnancy rate of 47.6% after PRP therapy in a RCT.[22] This was higher than our study (33.33%). This may be because of more number of patients with secondary infertility in the first study and patients with secondary infertility are known to have better results in IVF. Also, Madhavan included patients with atleast 1 failed IVF cycle however our study included patients with atleast 2 failed IVF cycles and success rates in IVF decline with previous failed IVF cycles.
Molina et al reported an ongoing pregnancy rate of 26.3% after PRP therapy.[23] The study included patients with age 33 to 45 years. In our study, the ongoing pregnancy rates were 28.2% which was similar to the first study despite younger population in our study. This may be because in the first study 2 out of 5 patients with ongoing pregnancies were oocyte recepients. However in our study, own oocytes were used.
In the present study, we compared treatment cycle outcomes with the previous cycle. The previous cycle acts as a control. There was no difference in clinical characteristics of patients like age, BMI, duration of infertility, etiology of infertility. So, there was no confounding factor in our study.
There were few limitations in our study. Firstly, ours is not a RCTs, thus effectiveness was evaluated by comparing treatment cycle with previous cycle. Sample size was small due to time bonding. Follow up was upto 13 weeks only. So, we can’t comment on live birth rate. Also anomaly scan could not be followed, so we don’t know whether PRP is associated with fetal anomalies or not. Long term implications of PRP on obstetric and perinatal outcomes are not known. As these were FET cycles, patients were already on ecosprin, argiprime and sildenafil so we are not sure that increase in endometrial thickness and vascularity was due to PRP alone or a combination of all preparations.
CONCLUSION
Well designed RCTs and metanalysis are required to understand the molecular mechanisms underlying PRP therapy. Despite some limitations of our study, we conclude that PRP is a safe, inexpensive and acceptable alternative for endometrial preparation of infertile patients with ≥2 failures due to suboptimal endometrium.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- American college of obstetricians and gynecologists. revitalize. In: Gynecology data definitions. Washington DC: American college of obstetrician and gynecologist; 2017.
- [Google Scholar]
- International committee for monitoring Assisted Reproductive Technology (ICMART) world report: Assisted reproductive technology 2003. Fertil Steril. 2011;95:2209-22. 22.e1-17
- [Google Scholar]
- The relationship between uterine artery two-dimensional color doppler measurement and pregnancy outcome: a prospective observational study. J Reprod Infertility. 2017;18:251-6.
- [Google Scholar]
- Endometrial preparation: effect of estrogen dose and administration route on reproductive outcomes in oocyte donation cycles with fresh embryo transfer. J Hum Reprod. 2016;31:1755-64.
- [Google Scholar]
- Does low dose aspirin improve pregnancy rate in women undergoing frozen thawed embryo transfer cycle? A pilot double blind, randomized placebo controlled trial. J Obstet and Gynaecol Research. 2018;45
- [Google Scholar]
- An overview on sildenafil and female infertility. Ind J Health Sci & Biomed Res Kleu. 2016;9:131-6.
- [Google Scholar]
- Endometrial growth and uterine blood flow: a pilot study for improving endometrial thickness in patients with a thin endometrium. Fertil Steril. 2010;93:1851-58.
- [Google Scholar]
- The use of combination of pentoxyfylline and tocopherol in women with a thin endometrium undergoing assisted conception therapies-a report of 20 cases. Hum Fertil (Camb). 2009;12:198-203.
- [Google Scholar]
- Therapeutic role of granulocyte colony stimulating factor(G CSF) for infertile women under in vitro fertilization and embryo transfer (IVF ET) treatment: a meta-analysis. Arch Gynecol Obstet. 2018;298:861-71.
- [Google Scholar]
- Endometrial thickness and pregnancy rates after IVF; A systematic review and meta-analysis. Hum Reprod Update. 2014;20:530-41.
- [Google Scholar]
- The impact of a thin endometrial lining on fresh and frozen-thaw IVF outcomes: an analysis of over 40000 embryo transfers. Hum Reprod. 2018;33:1883-88.
- [Google Scholar]
- Is platelet rich plasma a future therapy in pain management? Med Clin North AM 2016
- [Google Scholar]
- Platelet rich concentrates differentially release growth factors and induce cell migration in vitro. Clin Orthop Relat Res. 2015;473:1635-43.
- [Google Scholar]
- Autologous platelet rich plasma promotes endometrial growth and improves pregnancy outcomes during in vitro fertilization. Int J Clin Exp Med. 2015;8:1286-90.
- [Google Scholar]
- Can autologous platelet rich plasma expand endometrial thickness and improve pregnancy rate during frozen-thawed embryo transfer cycle? A randomized clinical trial. Taiwanese Journal of Obstetrics and Gynecology. 2018;57:810-813.
- [Google Scholar]
- Effect of autologous platelet rich plasma treatment on refractory thin endometrium during the frozen embryo transfer cycle: a pilot study. Front Endocrinol. 2019;10:61-9.
- [Google Scholar]
- Autologous platelet rich plasma infusion improves clinical pregnancy rate in frozen embryo transfer cycles for women with thin endometrium. Medicine (Baltimore). 2019;98:e14062.
- [Google Scholar]
- Treatment of thin endometrium with autologous platelet rich plasma: a pilot study. JBRA Assist Reprod. 2017;21:54-6.
- [Google Scholar]
- Autologous intrauterine platelet rich plasma instillation for suboptimal endometrium in frozen embryo transfer cycles: A pilot study. J Human Reprod Sci. 2017;10:208-12.
- [Google Scholar]
- Vaginal color doppler assessment of uterine artery impedance correlates with immunohistochemical markers of endometrial receptivity required for implantation of an embryo. Fertil Steril. 1995;63:101-8.
- [Google Scholar]
- Intrauterine autologous platelet-rich plasma therapy to improve implantation rates in patients undergoing frozen embryo transfer: a pilot study. Onco Fertil Journal. 2018;1:81-85.
- [Google Scholar]
- Platelet rich plasma as an adjuvant in the endometrial preparation of patients with refractory endometrium. JBRA Assist Reprod. 2018;22:42-8.
- [Google Scholar]







