Translate this page into:
Uterine cavity assessment prior to IVF: comparison of 2D, 3D ultrasound, and hysteroscopy
Address for correspondence: Dr. Sonia Malik, IVF Specialist in New Delhi India. Currently, She is Centre Head of Southend Fertility & IVF Centre; Dr. Sandeep Talwar, IVF Specialist in New Delhi, India. Currently, She is a Consultant in Southend Fertility & IVF Centre, New Delhi, India. E-mail: sm_doc@southendivf.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
There is a conflicting evidence that prior hysteroscopy in IVF treatment is beneficial in terms of successful pregnancy rate and subsequent live birth rate. So a study was planned to compare 2D TVS & 3D USG in detecting uterine anomalies in infertile patients & to know whether prior hysteroscopy has any effect on Clinical Pregnancy and Abortion rate. A sample size of 90 was selected and further randomized into 3 groups. Patients were randomized over 6-month time. All patients underwent same baseline investigations. In group 1 subjects, 2D TVS was done to detect uterine anomalies, in group 2 3D USG was performed and group 3 subjects underwent gold standard diagnostic hysteroscopy. Subjects in group 1 & 2 who tested positive for uterine anomalies were confirmed with diagnostic hysteroscopy and subsequently excluded from the study. Those subjects who had false positive results in group 1 & 2 were included in group 3 for Frozen Embryo transfer. This procedure was done till each of the 3 groups had 30 subjects. Furthermore, subjects in group 1 & 2 who tested negative for uterine anomalies, underwent IVF but did not conceive further underwent diagnostic hysteroscopy to confirm the diagnosis as a part of calculating Sensitivity and Specificity of 2D TVS and 3D USG. A total of 160 patients were accessed and finally 90 were included in the study. There was no significant difference in baseline demographic characteristics, type of infertility, duration of infertility, hormonal profile & mean antral follicle count and size. The Sn, Sp, PPV for 2D TVS & 3D USG was found to be 66.6%, 90%, 75% & 90.9%, 95% and 90.9% respectively. There was no difference in CPR and miscarriage rate in patients who conceived in each group. The results of the study are in line with the previous studies. Larger scale RCTs need to be conducted to ascertain the exact role of prior hysteroscopy in pregnancy outcome in infertile patients with no uterine anomalies.
Keywords
2D TVS
3D USG
hysteroscopy in uterine anomaly
prior hysteroscopy
hysteroscopy in infertility
INTRODUCTION
It has been estimated that approximately 15% of the couples are suffering from subfertility, which can be defined as not able to conceive after regular unprotected intercourse continuously for 12 months. In women with age more than 35 years cut-off is generally taken as 6 months. Approximately, 50% of the couples have female factor infertility and in 20% of cases of subfertility the cause remain unexplained. In 10% of the women with subfertility and approximately 50% of women with recurrent implantation failure, uterine cavity abnormalities are detected.[1] Given the chance that uterine anomaly may contribute to reduced fertility and recurrent implantation failure (RIF), evaluation of the uterine cavity is suggested as a routine test in the evaluation of infertile women.
There are many causes of in-vitro fertilization (IVF) failure especially factors such as uterine anomalies, thrombophilias, metabolic, and hormonal misbalance as well as infections and immunological factors.
For improving the outcome of intra-cytoplasmic sperm injection (ICSI) in case of IVF failure, various methods have been used, for example attempts have been made to make the quality of embryos better and increase the receptivity of endometrium, or improve the interaction between embryos and endometrium.[2,3] It has been reported in the past that if hysteroscopy is done in the preceding cycle in cases of three or more failed embryo transfer (ET),[4] it improves pregnancy outcome. But, a recent multicenter, randomized control trial has opposite results and according to the authors of the study prior hysteroscopy has no value in improving pregnancy outcome.[5]
Transvaginal sonography (TVS) has been the traditional screening test for diagnosing uterine malformations. TVS has been an important part of IVF management and is a process quite familiar among women; In addition, it is very well tolerated. A positive predictive value in baseline perivulatory TVS has been reported to be up to 85% to 95%. There are certain conditions, which cannot be distinguished on TVS alone like a sumucosal fibroid associated with multiple fibroids, polyp or just thickened endometrium, septatate, or acuate uterus.
Three-dimensional USG evaluation of uterine cavity has recently gained traction in the IVF treatment as it provides a detailed 3D image of the uterine cavity. The widespread use of transvaginal three dimensional ultrasound gives the benefit of more close to real diagnosis yet being able to give the benefit of being completely noninvasive and on outpatient basis.
In view of the above, there is a conflicting evidence that prior hysteroscopy in IVF treatment is beneficial in terms of successful pregnancy rate and subsequent live birth rate. Similarly, few studies are available depicting the role of 3D USG prior to IVF treatment improving the pregnancy rate and outcome.
Currently, there is no published literature comparing the above two methods in terms of their successful pregnancy rate.
The current study compares prior 2D USG, 3D USG, and hysteroscopic evaluation of uterine cavity in IVF patients in terms of evaluation of unknown uterine anomalies and successful pregnancy rate with following objectives:
Primary objective: Comparison of 2D TVS, 3D USG, and hysteroscopy in IVF patients in evaluation of uterine pathologies.
Secondary objectives: (A). Comparison of 2D TVS, 3D USG, and hysteroscopy in IVF patients in evaluation of clinical pregnancy rate in patients with normal uterine cavity. (B). Comparison of 2D TVS, 3D USG, and hysteroscopy in IVF patients in evaluation of miscarriage rate with normal uterine cavity.
METHODOLOGY
To achieve abovementioned objectives, a prospective comparative study was planned to be carried out in Outpatient department, Southend Fertility centre (Vasant Vihar, Max Hospital Saket, and Birla Hospital Gurgaon). Study subjects were chosen to be infertile patients undergoing IVF with having age < 42 years, No known uterine anomalies, no male factor infertility. Patients with age ≥ 42 years, male factor infertility, previously known uterine anomalies, stage III or IV endometriosis were not included in the study.
Sample size was determined by using study by Sahu L et al. who reported that rate of abnormal findings in infertile patient who underwent diagnostic hysteroscopy was 34.88% after examining 324 patients in Gynae OPD of Maulana Azad Medical College since diagnostic hysteroscopy is the gold standard test for detecting uterine pathologies. Taking into account the proportion of 35% as rate of uterine pathology in infertile patients, 95% confidence interval with a 10% margin of error, sample size comes out to be 88 using the following formula rounded off to 90.
Baseline blood testing were done to all recruited patients for hemoglobin, complete blood picture, blood glucose, liver function tests, kidney function tests. A detailed meticulous infertility work up was done. Husband semen analysis after abstinence for 3 to 5 days was done at our facility at Southend Fertility centre. Baseline levels of FSH, LH, TSH, prolactin, AMH were done on day 2 to 3 of the cycle. Antral follicle count for ovarian reserve was also done on day 2 to 3 of cycle. The subjects were further randomized into three groups and received the treatment according to the protocol. Randomization was done using computer generated random number tables.
Group 1 and 2 (n = 30 and 30): After undergoing baseline investigations patients were subjected to 2D TVS and 3D USG, respectively in the follicular phase of the menstrual cycle. Those with suspected uterine anomalies were subjected to diagnostic and therapeutic hysteroscopy. Those patients with confirmed uterine pathology on hysteroscopy were treated and subsequently excluded from the study. Those with normal hysteroscopy findings were recruited to Group 3. Frozen embryo transfer (blastocyst) was performed for all to remove confounding.
Group 3 (n = 30): After undergoing baseline investigations patients were subjected to hysteroscopy in the follicular phase of the menstrual cycle. Those with uterine anomalies were treated in the same sitting but excluded from the study. Those with normal hysteroscopy findings were recruited to this group. Frozen embryo transfer (blastocyst) was performed for all to remove confounding.
This was the protocol followed in the first part of the study. By the first part of the study we were only able to calculate the positive predictive value (PPV) and negative predictive value (NPV) of 2D and 3D USG. Sensitivity and specificity could only be calculated if the data on false negative results was available in each group. That is, the number of patients who appeared apparently normal on 2D and 3D USG but showed intrauterine pathology on subsequent hysteroscopy. Hence, in the second part of the study, all patients belonging to group 1 and 2, who did not conceive, were subjected to diagnostic hysteroscopy. Considering hysteroscopy as the gold standard tool in diagnosis of intrauterine pathology, sensitivity and specificity of each diagnostic modality was then calculated after all patients in groups 1 and 2 underwent hysteroscopy and presence/absence of intrauterine pathology was confirmed.
Data were analyzed using descriptive statistics, chi-square test, and Mann Whitney U test to compare the three groups using 2D TVS, 3D USG, and hysteroscopy. Variables were summarized using summary statistics like, mean, standard deviation, and percentage. Sensitivity, Specificity, Positive Predictive Value was calculated using 2 × 2 table. Proportion of uterine pathologies, clinical pregnancy and miscarriage in three unmatched groups was compared through chi-square test and Mann Whitney U test.
The study was started after approval from the Independent Ethics Committee, Indian Fertility Society (DCR/2019/NS/1002) written consent was taken from all participants before interview and examination. The treatment of all patients was done fairly and squarely according to established protocols.
RESULTS
Among a total of 160 patients who were assessed for eligibility 20 patients did not meet the inclusion criteria, 15 patients refused to participate in the study, eight other reasons and 27 patients were subsequently excluded due to abnormal uterine findings leaving 90 patients (30 for each group) for the further analysis [Figure 1].

- Consort diagram of results of the study.
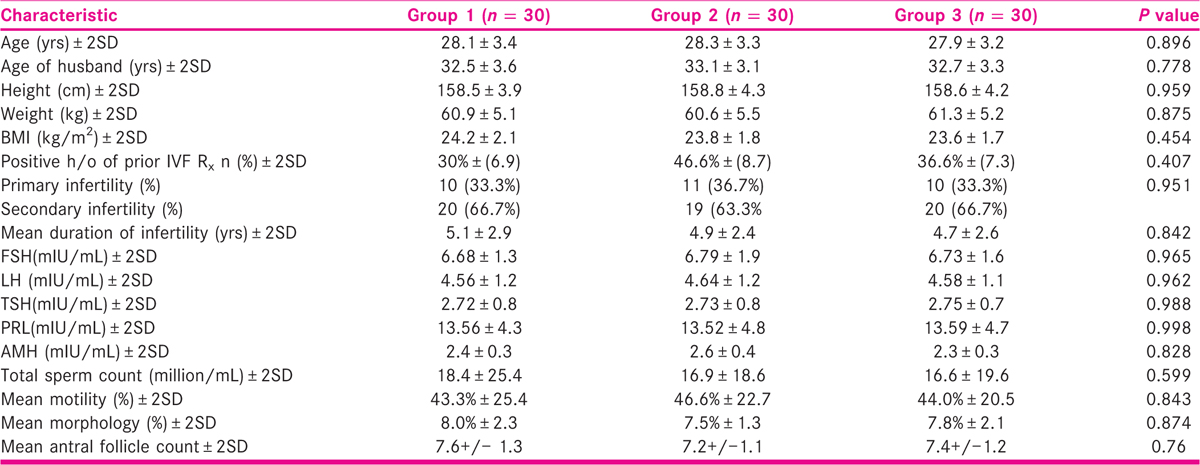
Baseline characteristics of participants of each group are depicted in Table 1. There was no significant difference in any characteristics.
Those patients of group 1 and 2 who had uterine abnormality [Table 2] were further subjected to diagnostic hysteroscopy for confirmation [Table 3].
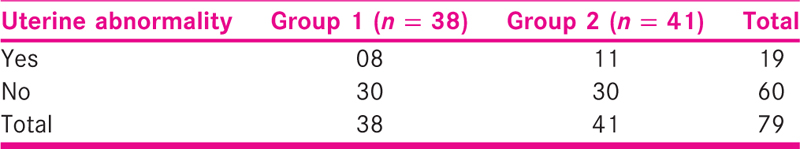
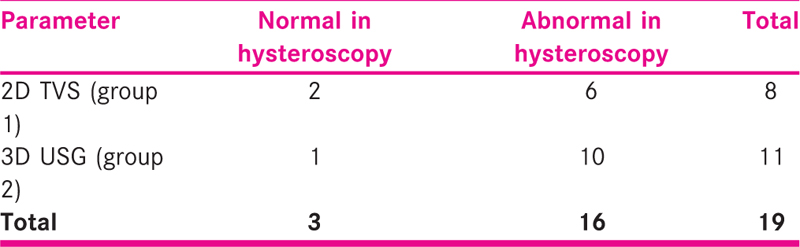
Positive predictive value of 2D TVS and 3D USG PPV
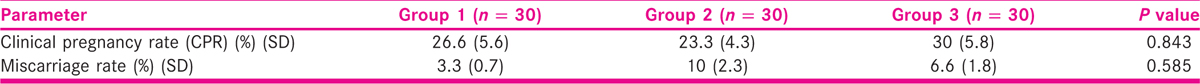
Clinical pregnancy rate and miscarriage rate: Table 4 highlights CPR and miscarriage rate. There was no significant difference in groups in either of the parameters.
Participants who did not undergo any conception, that is, 21 and 20 participants in group 1 and 2, respectively were further subjected to hysteroscopy to confirm normal uterine findings to calculate sensitivity and specificity of the tests as a part of objective of the study [Tables 5-7].

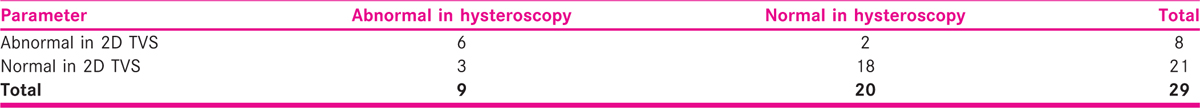

2 × 2 tables were constructed to calculate Sn and Sp of 2D TVS and 3D USG. Sensitivity 2D TVS: 66.6%; Specificity of 2D TVS: 90%; Sensitivity of 3D USG: 90.9%; Specificity of 3D USG: 95%.
DISCUSSION
In our study we found that sensitivity of 2D TVS is 66.6%, specificity as 90%, PPV as 75% and NPV as 90%. In the study conducted by Parsons AK and Kim AH,[6,7] the baseline periovulatory PPV was reported to be 85% to 95%. Similarly, in a study conducted by Ayida G et al.[8] the 2D TVS was found to have Sn = 84.5%, Sp = 98.7%, PPV = 98% and NPV = 89.2%. In general, it can be inferred that 2D TVS has more specificity than sensitivity in diagnosing uterine malformations/abnormalities. Hence, 2D TVS is more useful in ruling out the uterine abnormalities. In the current study, the sensitivity of 2D TVS came out to be 66.6% and specificity as 90%. The low sensitivity as compared to other studies can be attributed to less sample size which leads to increase in error. Also, the study was conducted in settings of a private IVF center where the patient inflow is limited as compared to large tertiary care centers with limited time to recruit patients. But, the specificity of 2D TVS in the current study is comparable to other studies.[6,7,8] Hence, hysteroscopy is almost always advised for patients coming in for infertility treatment owing to limited scope of 2D TVS in diagnosis certain uterine conditions as mentioned above.
Many authors have considered 3D USG as a viable alternative tool for Hysteroscopy in valuation of uterine cavity prior to IVF treatment.[9,10,11]. In the current study, the 3D USG was found to have 90.9% sensitivity, 95% specificity, 90.9% PPV, and 95% NPV, which is comparable to previous studies. As with 2D TVS, 3D USG has lower sensitivity as compared to specificity, which is similar to our study (Sn = 90.9%, Sp = 95%). Hence, 3D USG has more roles as a screening tool rather than as a diagnostic method of choice especially if facilities of hysteroscopy are present and there is no underlying contraindication for hysteroscopy like ongoing clinical pregnancy. 3D USG is also a viable alternative to hysteroscopy in terms of Patient comfort, pain, need to anesthesia and relatively higher cost.
As part of secondary objective of the study, we also determined whether prior hysteroscopy has any effect on clinical pregnancy rate, Overall conception rate and miscarriage rate. It has been conclusively proven that hysteroscopy is the gold standard test for diagnosing uterine anomalies. However, the utility of routine hysteroscopy prior to IVF is an ongoing debate and the current evidence is inconclusive at best. According to NICE guidelines hysteroscopy is not recommended as a part of prior assessment for subfertility unless indicated clinically,[10] while the European Society for Human Reproduction and Embryology recommends hysteroscopy prior to IVF in confirmation and treatment in case any abnormality is detected.[10]
In our study we found that prior hysteroscopic treatment has no statistically significant effect on clinical pregnancy rate (P = 0.842), overall conception rate (P = 0.861), and miscarriage rate (P = 0.585). This objective was tested owing to a recent systemic review to evaluate the current evidence in utility of hysteroscopy in improving pregnancy rates in infertile women with no other gynecological symptoms by Bosteels et al.[12] In the past, several studies have evaluated the question of benefits of hysteroscopy in women with two or more failed IVF attempts. El-Toukhy et al. in 2008 evaluated such benefits of hysteroscopy through systematic review of the available evidence. Accordingly, analysis showed significantly better outcome in terms of pregnancy rate of the hysteroscopy subgroup with normal uterine findings.[13]
It has been reported that introduction of hysteroscopy inside the uterine cavity may itself facilitate future embryo transfers as it allows for direct examination of cavity to detect anomalies such as uterine configuration anomalies like arcuate uterus and measurement of uterocervical length.[13] Such information obtained through direct visualization of the cavity could facilitate decision to where deposit embryo in terms of depth and vascularity within the cavity.[14,15] Finally, it has been hypothesized that introduction of hysteroscope inside the cavity may cause an injury to the endometrial lining which in turn results in release of cytokines and growth factors,[16] which ultimately leads to more likelihood of implantation success.[17,18,19,20]
A recent study published in Cochrane review by Kamath SM et al. concluded that at present, due to lack of high quality evidence, hysteroscopy is not recommended as a screening tool in the normal population of infertile females with a normal USG or HSG in prior to IVF routine fertility work-up for improving IVF success rate. Due to unclear allocation concealment in the studies showing beneficial effects of hysteroscopy, there was uncertainty whether routine hysteroscopy actually increases pregnancy and live birth rates even in those women who had two or more failed IVF attempts.[21] Similar results were reported by Smit GJ et al. in a pragmatic multicenter, randomized controlled trial in seven university hospitals in Netherlands (inSIGHT study).[22] More studies are required to arrive at a meaningful conclusion regarding role hysteroscopy in IVF treatment with a normal uterus with no malformations.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Evaluation of outpatient hysteroscopy, saline infusion hysterosonography, and hysterosalpingography in infertile women: a prospective, randomized study. Fertil Steril. 2000;74:1029-34.
- [Google Scholar]
- Implantation failure: molecular mechanisms and clinical treatment. Hum Reprod Update. 2011;17:242-53.
- [Google Scholar]
- Molecular aspects of implantation failure. Biochim Biophys Acta. 2012;1822:1943-50.
- [Google Scholar]
- Effect of treatment of intrauterine pathologies with office hysteroscopy in patients with recurrent IVF failure. Reprod Biomed Online. 2004;8:590-94.
- [Google Scholar]
- Hysteroscopy in recurrent in-vitro fertilisation failure (TROPHY): a multicentre, randomised controlled trial. Lancet. 2016;387:2614-21.
- [Google Scholar]
- Sonohysterography for endometrial abnormalities: preliminary results. J Clin Ultrasound. 1993;21:87-95. 1993
- [Google Scholar]
- Sonohysterographic screening before in vitro fertilization. Fertil. Steril.. 1998;69(5):841-844.
- [Google Scholar]
- Uterine cavity assessment prior to in vitro fertilization: comparison of transvaginal scanning, saline contrast hysterosonography and hysteroscopy. Ultrasound Obstet Gynecol. 1997;10:59-62.
- [Google Scholar]
- The use of three dimensional hysterosonography in recurrent implantation failure prior to in vitro fertilization. Sch J App Med Sci. 2017;5:730-7.
- [Google Scholar]
- Three-dimensional sonohysterography compared with vaginoscopic hysteroscopy for evaluation of the uterine cavity in patients with recurrent implantation failure in vitro fertilization cycles. J Minim Invasive Gynecol. 2012;19:503-08.
- [Google Scholar]
- Three-dimensional hysterosonography versus hysteroscopy for the detection of intracavitary uterine abnormalities. Int J Gynaecol Obstet. 2007;97:6-9.
- [Google Scholar]
- The effectiveness of hysteroscopy in improving pregnancy rates in subfertile women without other gynaecological symptoms: a systematic review. Hum Reprod Update. 2010;16:1-11.
- [Google Scholar]
- Outpatient hysteroscopy and subsequent IVF cycle outcome: a systematic review and meta-analysis. Reprod Biomed Online. 2008;16:712-19.
- [Google Scholar]
- Is hysteroscopic correction of an incomplete uterine septum justified prior to IVF? Reprod Biomed Online. 2007;14:335-40.
- [Google Scholar]
- Influence of position and length of uterus on implantation and clinical pregnancy rates in IVF and embryo transfer treatment cycles. Hum Reprod. 2000;15:1943-46.
- [Google Scholar]
- Expression of proinflammatory cytokines in mouse blastocysts during implantation: modulation by steroids hormones. Am J Reprod Immunol. 2002;47:2-11.
- [Google Scholar]
- High pregnancy rate after hysteroscopy with irrigation in uterine cavity prior to blastocyst transfer in patients who have failed to conceive after blastocyst transfer. Fertil Steril. 2000;4:S206.
- [Google Scholar]
- Local injury to the endometrium doubles the incidence of successful pregnancies in patients undergoing in-vitro fertilization. Fertil Steril. 2003;79:1317-22.
- [Google Scholar]
- Favourable influence of local injury to the endometrium in intracytoplasmic sperm injection patients with high-order implantation failure. Fertil Steril. 2007;87:198-201.
- [Google Scholar]
- Screening hysteroscopy in subfertile women and women undergoing assisted reproduction. Cochrane Database Syst Rev. 2019;4:CD012856.
- [Google Scholar]
- Hysteroscopy before in-vitro fertilisation (inSIGHT): a multicentre, randomised controlled trial. Lancet. 2016;387:2622-29. doi: 10.1016/S0140-6736(16)00231-2
- [Google Scholar]