Translate this page into:
Variation of post trigger LH, progesterone and HCG levels with BMI and its impact on recovery rates of oocytes during IVF/ICSI cycles
Address for correspondence: Dr. Mohita Gupta, G-28, Tej Bagh Colony, Patiala, Punjab, India. E-mail: mohitasingal@gmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Aims and Objectives:
To assess the variation in post trigger LH, progesterone and HCG levels with BMI after agonist/HCG trigger during ART cycles and its impact on recovery rate of oocytes.
Material and Methods:
A prospective study was conducted at Max Multispeciality Hospital Panchsheel Park, New Delhi from May 2018 – Feb 2019. A total of 101 patients (51 in agonist trigger and 50 in HCG trigger group) met the inclusion and exclusion criteria, were enrolled after taking written consent. Agonist trigger patients received either decapepty l0.3 mg or lupride 3 mg trigger. HCG trigger group received ovitrelle 500 mcg. Trigger day and 10–12 hours post trigger LH, progesterone and HCG was done and its correlation to BMI and recovery rates was analyzed. P value <0.05 was considered significant.
Results:
BMI showed significant negative correlation with post trigger LH levels (P=0.047), LH rise (P=0.036) in group 1 and post trigger HCG levels in group 2 (P=0.026) levels. When BMI was categorized into 4 groups, in group 1, post trigger progesterone showed decreasing trend with increasing BMI (P=0.05) with comparable recovery rates but in group 2, post trigger HCG, progesterone levels and recovery rates were found to drop as BMI increased >30 kg/m2.
Conclusion:
BMI should be considered while deciding dose of the trigger keeping in mind the variation of Post trigger LH, progesterone and HCG levels with BMI. Further large randomized controlled trails are required to validate the results found in this study.
Keywords
BMI
HCG
IVF
INTRODUCTION
Obesity is a leading cause of various medical and reproductive disorders and is being labelled as an epidemic. Abnormal body mass index (BMI) affects in vitro fertilization (IVF) outcomes[1,2,3] but the underlying mechanisms are not well elucidated. To the best of our knowledge, limited literature is available on the effect of BMI on post trigger hormone levels which impact the recovery rate of the oocytes. This study is thus put forth to assess the same.
AIMS AND OBJECTIVES
To assess the variation in post trigger luteinizing hormone (LH), progesterone (P4) and human chorionic gonadotropin (HCG) levels with BMI after agonist/HCG trigger during IVF/ICSI cycles.
To assess the impact on recovery rates (RR) of oocytes of these values
MATERIAL AND METHODS
This prospective observational study was conducted from May 2018 to Feb 2019. Scientific and Ethical committee approval was taken. Written informed consents were taken from all patients before starting the stimulation. All patients undergoing agonist/antagonist/autologous/donor IVF/ICSI cycles were included. Patients who were not willing to give consent, who were unable to get investigations done as per protocol and who required cycle cancellation like a poor responder patient with no follicular recruitment were excluded from the study. Total 101 patients, 51 patients in agonist trigger (group 1) and 50 patients in HCG trigger (group 2) were enrolled in the study. In antagonist cycles, patients were started on gonadotropins injections (Injection FSH/HMG) from day2/3 with dose of 150-300 IU according to BMI, age of patient, initial history, cause of infertility, ovarian reserve and day 2/3 parameters (AFC, FSH, LH, E2). The number of developing follicles was monitored periodically by ultrasound examination during ovarian stimulation and titration of doses was done accordingly. Antagonist (Inj Cetrolix 0.25mg subcutaneous) was started when at least one follicle reached 14 mm or estradiol levels were >500pg/ml (usually done on day 5/6 of cycle). When at least three follicles reached 17–18 mm size, patients with estradiol levels >3500pg/ml, showing tendency to hyperstimulate were given agonist trigger (Inj lupride 3mg/triptorelin 0.3mg subcutaneous, rest were given recombinant HCG trigger (Inj ovitrelle 500mcg subcutaneous). Last dose of antagonist was given 12 hours prior to trigger time. In agonist cycles, agonist lupride 0.4ml s/c started from day 21 of previous cycle followed by stimulation from day2/3. HCG trigger was given in a similar manner as above followed by egg retrieval transvaginally, 34–36 h after trigger administration. Serum LH, Estradiol (E2), Progesterone (P4) levels in both groups were measured in samples drawn in the morning of trigger day and 10-12 hours after the trigger. HCG levels were additionally measured 10–12 hours after HCG trigger in group 2. Variations in LH, P4 and HCG levels were studied in relation to BMI. Patients were categorized into four subgroups according to BMI: <18, 18–25, 26–30, >30 kg/m2 and labelled as 1a,1b,1c,1d in group 1 and 2a,2b,2c,2d in group 2 and correlation with LH, P4 and HCG levels were calculated. In group 1(GnRHa trigger group), patients were also divided into five sub-groups according to post trigger LH levels: <15IU/L, 15–30 IU/L, 30–45 IU/L, 45–60 IU/L and >60 IU/L and labelled as subgroup 1A,1B,1C,1D,1E and correlation with BMI and recovery rates were calculated. Another sub-group analysis was done by categorizing patients into two subgroups according to post trigger progesterone levels − <9ng/ml and >9ng/ml in group 1[4] (labelled as1i and 1ii) and <3ng/ml and >3ng/ml in group 2[5] (labelled as 2i and 2ii) and correlated with BMI and recovery rates. Studies have been done evaluating post trigger progesterone cut off 2.3 ng/ml[5] and 9 ng/ml[4] with HCG trigger but we didn’t encounter very high post trigger progesterone levels with HCG trigger, so 3 ng/ml was taken as cut off with HCG trigger group. On the other hand, we didn’t happen to encounter any studies with agonist trigger evaluating post trigger progesterone at various cut off but patients with agonist trigger tend to have higher post trigger progesterone levels than HCG trigger, so 9 ng/ml was taken as cut off. LH and P4 rise were calculated by subtracting post trigger levels from trigger day levels and correlated with BMI. Recovery rates were calculated as number of oocytes retrieved divided by total number of follicles punctured multiplied by 100 with fluid aspirate of 1.5–8 ml (approximately 14–24 mm follicular size). Conventional IVF or ICSI was performed as indicated.
Data analysis
Categorical variables were presented in number and percentage (%) and continuous variables were presented as mean ± SD. Quantitative variables measured by Paired t-test. Qualitative variables were compared using Chi-Square test /Fisher’s exact test whenever the cell frequencies were less than 5. A P value of < 0.05 was considered statistically significant. The data was entered in MS EXCEL spreadsheet and analysis was done using Statistical Package for Social Sciences (SPSS) version 21.0.
RESULTS
Mean age of patients in group1 and group 2 was 33.39 and 34.18years, mean BMI was 25.23 and 25.50 kg/m2 which were statistically not significant [Table 1].

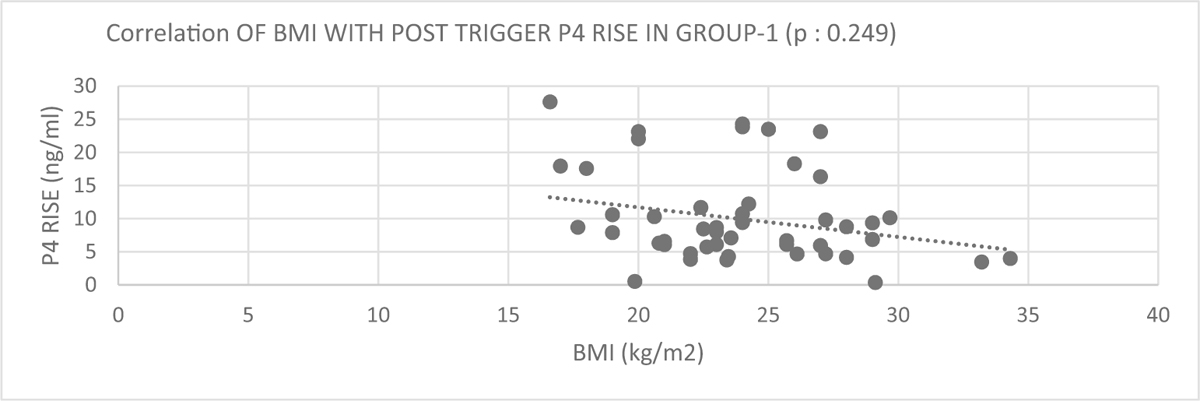
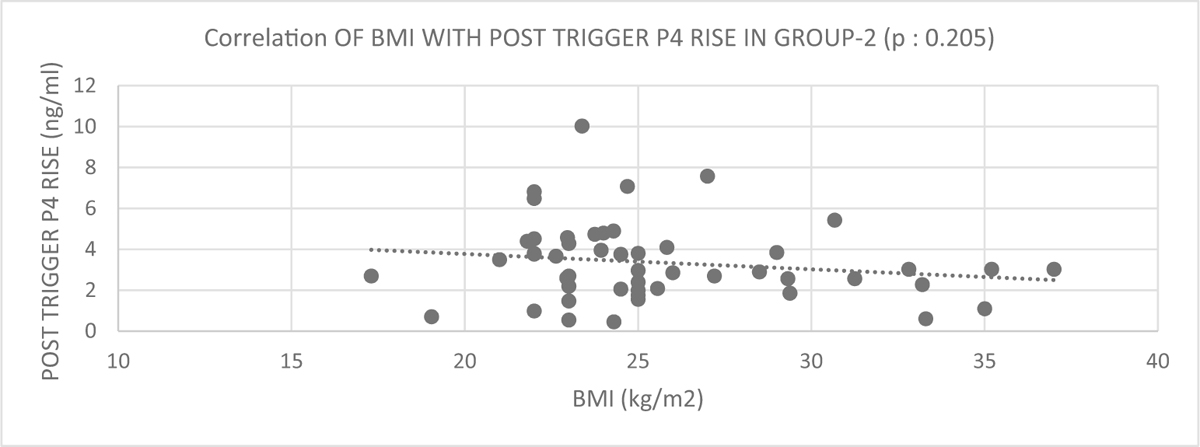
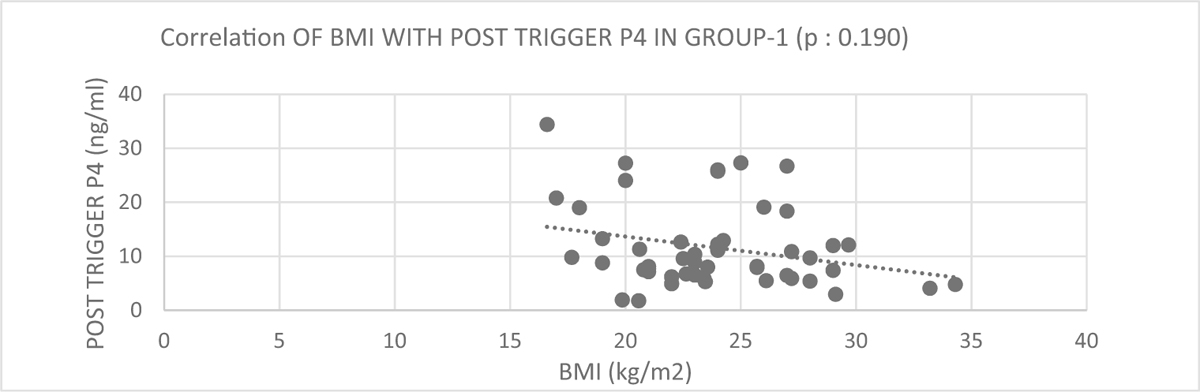
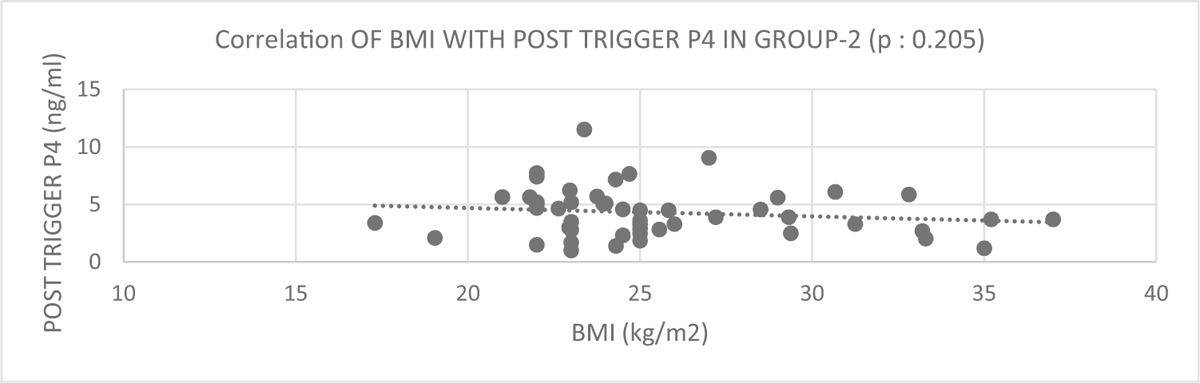
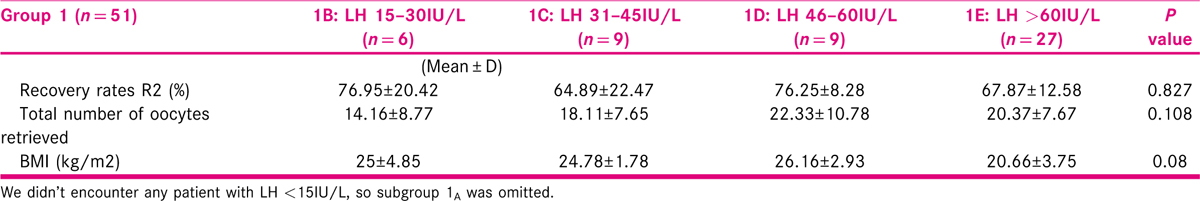
BMI showed significant negative correlation with post trigger LH (P = 0.047) and LH rise (P = 0.036) in group1 and post trigger HCG (P = 0.026) levels in group 2 [Figures 1,2,6]. Post trigger progesterone and progesterone rise didn’t show any significant difference in either group as shown in Figures 3-5,7.

- Correlation of BMI with post trigger in Group 1 (P = 0.047).
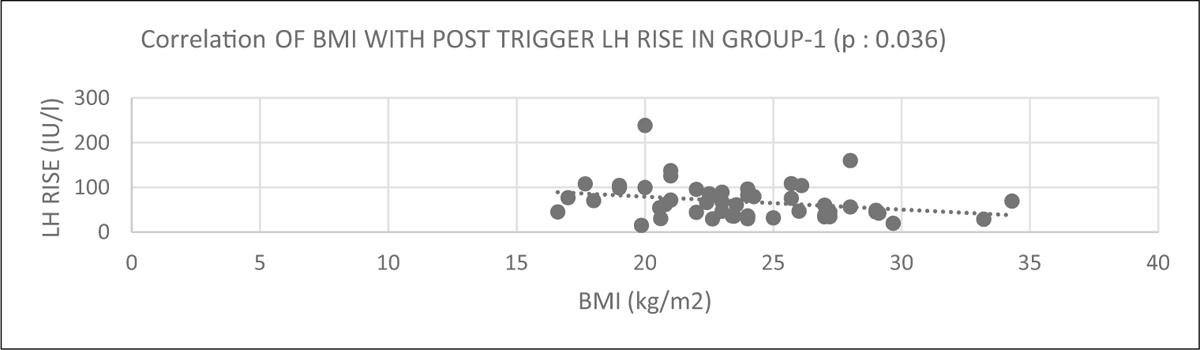
- Correlation of BMI with post trigger LH rise in Group 1 (P = 0.036)
- Correlation of BMI with post trigger P4 in Group 1 (P = 0.190)
- Correlation of BMI with post trigger P4 rise in Group 1 (P = 0.249)

- Correlation of BMI with post trigger P4 rise in Group 2 (P = 0.205)
- Correlation of BMI with beta HCG in Group 2 (P = 0.026)
- Correlation of BMI with post trigger P4 in Group 2 (P = 0.205)
When BMI was categorized into 4 groups, in group 1, post trigger progesterone showed decreasing trend with increasing BMI. As BMI increased from <18 to >30kg/m2, post trigger P4 levels decreased from 21.67 to 4.43 ng/ml (P = 0.05). Post trigger LH levels also demonstrated decreasing trend (LH fell from 77.6 to 51.6IU/L) but with non-significant difference. Recovery rates were comparable in all groups (Table 2). This was probably because the lowest level of LH was also above the required threshold ie 15IU/L.[6,7]

HCG levels also followed a similar trend. When BMI was categorized into 4 groups, in group 2, post trigger HCG levels were found to fall as BMI increased to >30kg/m2 (P = 0.076). Recovery rates were found to be significantly high in patients with BMI 26–30 kg/m2 than 18–25 kg/m2 (81.7 vs 65.4%, P = 0.034) but fell after BMI >30kg/m2 to 70.4% (along with HCG levels). Similarly, post trigger P4 levels also showed falling trend as BMI increased to >30kg/m2 (P = 0.589) [Table 2].
In subgroup analysis, after categorizing LH into 4 subgroups in group 1, patients with higher post trigger LH levels tend to have lower BMI (P = 0.08). There was no significant difference in recovery rates among groups [Table 3].
In another subgroup analysis, according to post trigger progesterone levels <9 and >9ng/ml in group 1 and <3 and >3ng/ml in group 2, we didn’t find any significant difference in BMI [Tables 4 and 5].


DISCUSSION
In our study, in agonist trigger cycles, we found post trigger LH and its rise was significantly inversely proportional to BMI (P = 0.047 and 0.036 respectively). When BMI was sub-grouped in four groups, post trigger progesterone levels showed significant downward trend as BMI increases. These findings were similar to Chang et al.,[6] who in his retrospective study of 1840 IVF cycles demonstrated statistically significant negative relationship between BMI and post trigger LH and Progesterone (P > 0.001) with lupride trigger. He concluded that obesity is an important parameter to consider before evaluating post trigger hormone levels. In contrast Meyer et al.,[7] in 535 fresh transfer cycles (375 autologous and 160 donor cycles) with agonist and dual trigger found that suboptimal responders (defined as LH<15IU/dl) demonstrated trend towards low BMI (21.75 vs 23.01 kg/m2 respectively) but this was statistically not significant (P = 0.766). Lowest LH found in our study was 21IU/L with BMI of 29kg/m2 and lowest BMI was 16.6kg/m2 with post trigger LH 45IU/L. Since there was no case of empty follicle syndrome, the value of BMI where a failed trigger being a cause for empty follicle syndrome happens could not be identified in our study.
In present study with HCG trigger, we found significant negative correlation of BMI with post trigger HCG levels (P = 0.029) similar to Elkind-Hirsch et al.,[8] Salha et al.,[9] Mizrachi et al.,[10] Carell et al.[11] and Bustillo et al.[12] Busillo et al.[12] in a retrospective analysis of 84 HCG trigger cycles demonstrated that HCG levels fell from 135 IU/L to 70 IU/L as BMI increased from <20kg/m2 to >29kg/m2 (P = 0.05) and patients with BMI >29 kg/m2 required higher dose of trigger to achieve same levels. Carell et al.[11] studied 247 autologous and 58 donor oocytes cycles and found mean intrafollicular HCG concentrations significantly decreased (P < 0.001) in patients with a BMI >30 kg/m2 compared with patients with a BMI of <30kg/m2, similar to our study.
Rodriguez et al5 in a retrospective study on HCG trigger in 16087 cycles demonstrated significant negative correlation of BMI with post trigger progesterone levels (P = 0.001). As BMI decreased from 25.9 to 23.8kg/m2, progesterone levels increase from <1ng/ml to >2.3ng/ml. We also found fall in post trigger progesterone levels after BMI >30kg/m2, but this was statistically insignificant.
Busillo et al.[12] didn’t find any significant correlation of BMI with number of oocytes retrieved but women with low BMI had higher number of MII oocytes in HCG trigger cycles. Salha et al.[9] in a prospective study on 50 women demonstrated that women with high BMI have less recovery rates, fertilization rates and pregnancy rates. Similar findings were seen by Carell et al.[11] In contrast, Mizrachi et al.[10] in prospective observational study on 326 women found no effect on mature oocytes, fertilization and pregnancy rates with BMI. We found significantly high recovery rates in patients with BMI 26-30kg/m2 than 18–25kg/m2 (81.7 vs 65.4%, P = 0.034) but fell after BMI >30kg/m2 to 70.4% i.e. in morbidly obese women.
Since we used higher than normal dose of HCG and agonist as trigger, we did not have LH and HCG levels in the range suggested where there were empty follicles. However, it may be kept in mind that with a higher BMI both HCG and LH levels after trigger were lower and if a lower dose is being used, they could have suboptimal levels leading to failed retrieval of oocytes.
SUMMARY AND CONCLUSION
In agonist trigger cycles, BMI is negatively correlated with post trigger LH and LH rise significantly. In HCG trigger cycles, BMI is negatively correlated with post trigger HCG levels significantly. When BMI was categorized into 4 groups in agonist trigger cycles, post trigger progesterone decreases with increasing BMI. When BMI was categorized into four groups, in HCG trigger cycles, post trigger HCG levels, post trigger progesterone levels and recovery rates falls after BMI >30kg/m2 i.e. in morbid obese women.
BMI should be considered while deciding dose of the trigger keeping in mind the variation of post trigger LH, progesterone and HCG levels with BMI. Further large randomized controlled trails are required to validate the results found in this study. We also recommend that further studies are done to evaluate the trigger dose based on BMI and its effect on post trigger hormone levels, recovery rates, fertilization rates and pregnancy outcomes.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Effect of body mass index on the outcome of in-vitro fertilization/intracytoplasmic sperm injection in women. J Hum Reprod Sci. 2017;10:37-43.
- [Google Scholar]
- The effect of female body mass index on in vitro fertilization cycle outcomes: a multi-center analysis. J Assist Reprod Genet. 2018;35:2013-23.
- [Google Scholar]
- Comparison of progesterone measurement on day of, and day after, HCG administration in IVF-embryo transfer cycles. Reprod Biomed Online. 2015;30:157-65.
- [Google Scholar]
- Lack of progesterone rise post-trigger correlates with sub-optimal clinical outcomes despite normal fertilization rate. Fertil Steril. 2016;106:174.
- [Google Scholar]
- Assessing the adequacy of gonadotropin-releasing hormone agonist leuprolide to trigger oocyte maturation and management of inadequate response. Fertil Steril. 2016;106:1093-100.
- [Google Scholar]
- Risk factors for a suboptimal response to gonadotropin-releasing hormone agonist trigger during in vitro fertilization cycles. Fertil Steril. 2015;104:637-42.
- [Google Scholar]
- Serum human chorionic gonadotropin levels are correlated with body mass index rather than route of administration in women undergoing in vitro fertilization − embryo transfer using human menopausal gonadotropin and intracytoplasmic sperm injection. Fertil Steril. 2001;75:700-4.
- [Google Scholar]
- Influence of body mass index and self-administration of hCG on the outcome of IVF cycles: a prospective cohort study. Hum Fertil (Camb). 2001;4:37-42.
- [Google Scholar]
- Human chorionic gonadotropin serum levels following ovulation triggering and IVF cycle outcome. J Assist Reprod Genet. 2018;35:891-8974.
- [Google Scholar]
- Body mass index is inversely related to intrafollicular HCG concentrations, embryo quality and IVF outcome. Reprod Biomed Online. 2001;3:109-11.
- [Google Scholar]
- Correlation between Body Mass Index and Serum Beta HCG levels post HCG with ART cycle outcomes. Fertil Steril. 2008;90:328-9.
- [Google Scholar]







