Translate this page into:
Impact of BMI on IVF outcome
Address for correspondence: Dr. Pinkee Saxena, 534 Mandakini Enclave, Alaknanda, New Delhi, India. E-mail: drpinkee@hotmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Nowadays increasing number of obese women are seen attending infertility clinics. The objective of this study was to find out relationship of body mass index (BMI) on IVF cycles and to note of increased BMI.
Materials and Methods:
This was a retrospective study. All the patients undergoing IVF during the study period were divided in to three groups based on BMI − Group 1: <25 kg/m2; Group 2: 25 to 29.9 kg/m2; Group 3: ≥30 kg/m2. Records were analysed such as patient’s age, BMI, duration and cause of infertility, antral follicle count and hormonal profile. The total gonadotropins dose used, duration of stimulation, number of retrieved oocytes and pregnancy rate were noted.
Results:
A total of 151 women with non-donor IVF cycles were analysed. There were 58 patients in Group 1, 68 patients in Group 2 and 25 patients in Group 3. Laboratory parameters such as serum FSH, serum LH, serum AMH and serum E2 were compared. Serum AMH were found to be slightly higher in the obese group but was not statistically significant. Other hormones levels were comparable in the three groups. The total gonadotropin dose required for stimulation of follicles was found to be significantly higher in Group 3. The number of oocytes retrieved was similar in the three groups and so was the pregnancy rate.
Conclusion:
The present study suggests that BMI does not have significant impact on IVF cycles.
Keywords
BMI
IVF
pregnancy
INTRODUCTION
Changing lifestyle has led to increase in the incidence of obesity. In addition, many women are delaying childbearing. So, nowadays we see many obese women seeking infertility treatment. Obesity has several health implications such as diabetes mellitus, cardiovascular disease, impaired lipid profile, uterine cancer and breast cancer.[1] Moreover, obesity is found to decrease successful pregnancy rates in both natural and assisted conception cycles.[2] Studies on effect of a raised body mass index (BMI) on the outcome of artificial reproductive techniques (ART) have conflicting evidences. Although some studies have found no effects of an increased BMI on in vitro fertilizations (IVF) cycles,[3,4] others have reported effects such as requirement of a higher dose of gonadotropins, longer stimulation period, lower oocyte retrieval.[5,6] The objective of this study was to find out relationship of BMI on IVF cycles and to note any adverse effect of increased BMI.
MATERIALS AND METHODS
This was a retrospective study performed at tertiary-based fertility centre − Max Multi Speciality Hospital, Panchsheel Park, New Delhi, from May 2016 to October 2017. All patients who underwent IVF at the centre were included in this. Records of patients undergoing IVF were analysed. Because this was a retrospective cohort study, no written informed consent for participation was obtained from the participants. All patients undergoing IVF/Intra cytoplasmic sperm injection (ICSI) cycle either with agonist or antagonist protocol were included in the study. Patients undergoing donor IVF cycles or gestational surrogacy cycles were excluded. Detailed history was taken and their weight and height measured. BMI was determined by the ratio of weight divided by the height squared in metric units.
Patients were given either agonist or antagonist protocol, based on initial history and evaluation, followed by follicular monitoring and titration of doses accordingly. They received trigger with Gonadotropins- releasing hormone agonist (GnRHa) or Human Chorionic Gonadotropins (hCG) when at least three follicles reach 17 to 18-mm size. Oocytes were retrieved transvaginally, 34 to 36 h after trigger administration. Standard laboratory protocols for IVF or ICSI were performed as indicated. Ultrasound-guided transfer of embryos was performed on Day 2/3/5 after oocyte pick-up. The luteal phase was supported with progesterone and estradiol (E2) as per standard protocol used in the institute and continued until 12 weeks of gestation in presence of a positive hCG test.
Serum hCG levels were measured 15 days after retrieval. A clinical pregnancy was defined as the presence of a gestational sac on ultrasound. Spontaneous abortion was defined as the loss of a clinical pregnancy before 20 weeks. In addition, ongoing pregnancy was defined as progression beyond 12 weeks of gestation. Fertilisation rate is defined as the ratio of number of fertilised oocytes to the number of oocytes retrieved in conventional IVF cycles. In ICSI, fertilisation rate is calculated by dividing number of fertilised oocytes by number of M2 oocytes.
Patient’s demographic factors such as age, BMI, duration of infertility, aetiology of infertility, antral follicle count (AFC), baseline follicle-stimulating hormone (FSH), luteinizing hormone (LH) and estradiol levels were reviewed. The total gonadotropins dose used, duration of stimulation, number of retrieved oocytes were noted. Based on the BMI calculated, the patients were grouped into three groups − Group 1 (normal weight): <25 kg/m2; Group 2 (overweight): 25 to 29.9 kg/m2; Group 3 (obese): ≥30 kg/m2. Their records were analysed.
Preliminary statistical comparisons were made by analysis of variance (ANOVA) and Chi-square tests using data grouped according to these BMI categories. The data presented in represent group means (±SD) and frequencies from the preliminary analyses (ANOVA and Chi-square). A simple Pearson correlation coefficient was calculated to determine whether BMI and age were independent or interrelated variables.
RESULTS
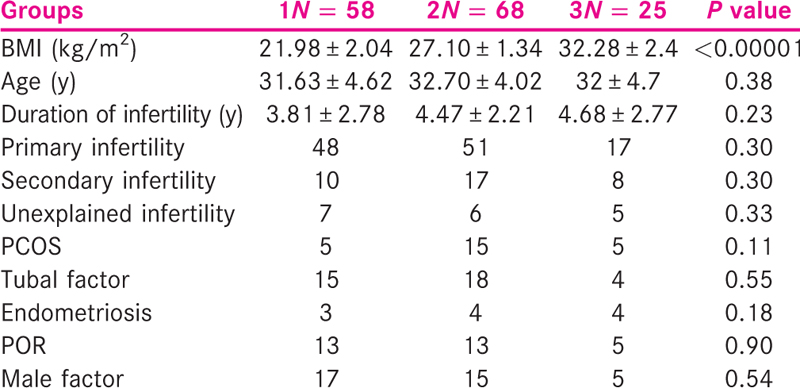
A total of 151 women with non-donor IVF cycles were analysed. There were 58 patients in Group 1, 68 patients in Group 2 and 25 patients in Group 3. The age of the patients studied ranged from 21 to 46 years with the mean age 32 years. The age of patient was similar in all the three BMI groups and so was the duration of infertility. Other demographic details such as type of infertility and cause of infertility were almost similar in the three groups as shown in Table 1.
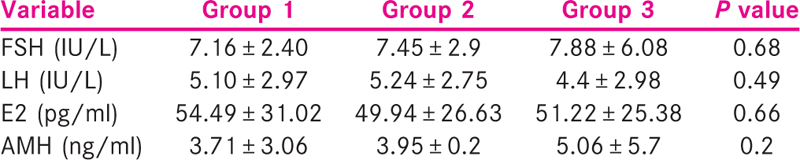
Laboratory parameters such as serum FSH, serum LH, serum anti-mullerian hormone (AMH) and serum E2 were compared. Serum AMH were found to be slightly higher in the obese group but was not statistically significant. Serum FSH, LH and E2 were comparable in the three groups [Table 2].
Ultrasound was performed to assess the AFC and endometrial thickness. There was no significant difference in the total number of antral follicles obtained in the three groups. The endometrial thickness achieved was slightly less in Group 3, though it was not statistically significant. On analysing the total gonadotropin dose required for stimulation of follicles, it was seen that the total gonadotropin dose required was found to be significantly higher in Group 3 (P = 0.023). The duration of stimulation was slightly longer in the obese group though not statistically significant (P = 0.058) [Table 3].
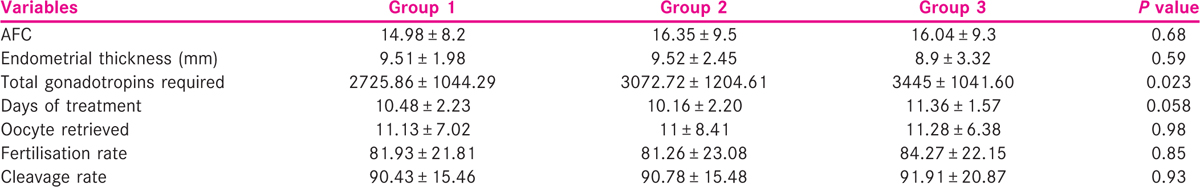
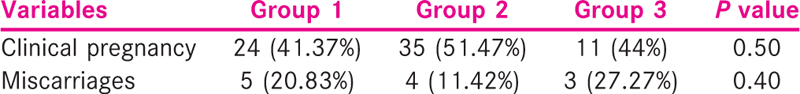
The number of oocytes retrieved was similar in the three groups and so were the fertilisation rate and the cleavage rate. The pregnancy outcome was similar in the three BMI groups. The miscarriage rate was higher in Group 3 as compared to the other two groups though not statistically significant [Table 4].
The correlation coefficient for BMI and age was calculated, and the value of R was 0.0557. Although technically a positive correlation, the relationship between the variables was weak.
DISCUSSION
There is inconsistent evidence regarding the effect of raised BMI on the outcome of assisted reproductive technology.
The study showed that there is a positive relationship between age and BMI though weak. Megan et al.[7] also showed relationship between age and BMI. They observed that at younger ages, a higher BMI has a pronounced negative influence on fertility, but the effect diminished as the patient’s age increases. The clinical pregnancy rates decreased with increasing BMI and increasing age. BMI has a much less profound effect on fertility as patients reach the age of 36 and higher.
AFC count performed was similar in all the three groups. We had a slightly decreased endometrial thickness in obese group which was not significant. Friedler et al.[8] in their study had observed that endometrial thickness was significantly lower in morbid obese group.
In our study, the total gonadotropin dose requirement was found to be significantly higher in Group 3. However, the duration of stimulation though slightly longer in the obese group was not statistically significant. Many studies have observed that the total gonadotropin dose and duration of stimulation were significantly higher in the obese group when compared to the normal BMI group.[9,10,11,12,13] However, length of treatment was significantly shorter in normal weight women as compared to other groups in study performed by Friedler et al. In a study performed by Hill et al.,[14] they stated that increased BMI may be associated with the need for fewer days of stimulation, fewer ampules of medication and a greater number of follicles produced without affecting pregnancy outcome rates.
Studies performed have shown that there are no significant differences in the number of retrieved oocytes in all groups.[8,9,11,13] We also had similar results. Other investigators have also found a decrease in the number of retrieved oocytes.[12,15,16,17] Singh et al.,[11] in their study, noted no difference in the number of oocyte retrieved but had decreased fertilisation and cleavage rate in patient with increasing BMI. They concluded that obesity impairs IVF outcome potentially by impairing oocyte quality but does not affect ovarian response to stimulation.
Ozekinci et al.[9] observed that the clinical pregnancy, spontaneous abortion and the ongoing pregnancy rates per transfer were comparable among the normal weight, overweight and obese women. Similar findings were observed by Koning et al.[18] In our study, also the pregnancy rate was similar in all the three groups. However, Singh et al.[11] observed a negative co-relation with increasing BMI for clinical pregnancy rate (P value = 0.040). Pinborg et al. also stated that the number of patients with positive serum human chorionic gonadotrophin decreased significantly with increasing BMI. Similar finding was observed by Rittenberg et al.[19] Kalem et al.[20] evaluated obesity and clinical pregnancy rates in IVF cycles in polycystic ovarian syndrome (PCOS) patients according to age groups. They observed that the clinical pregnancy rates were lower in the obese group, particularly in the age group ≥35 years than in the other BMI groups. However, this difference was found to be statistically insignificant. Higher rate of miscarriage has been observed with increased BMI in various studies.[18,21,22] A recent meta-analysis of the available evidence suggested that there was a significant increase in the odds of miscarriage in women with a BMI of ≥25 kg/m2 following spontaneously conceived pregnancies as well as following ovulation induction but not in women who underwent IVF/ICSI. This may be due to differences in the nature of the included studies and the type of denominator used to calculate the prevalence of miscarriage.[23] In our study, we found that miscarriage rate was higher in Group 3. This was not statistically significant. This may be due to the small sample size.
CONCLUSION
The present study indicates that BMI does not have a significant effect on IVF cycles. An increased requirement of gonadotropins for ovarian stimulation and an increased risk of miscarriage were however observed in patients with increased BMI. Hence, BMI alone should not be a factor for denying IVF to obese infertile patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Metabolic syndrome, chronic kidney, and cardiovascular diseases: Role of adipokines. Cardiol Res Pract. 2011;2011:653182.
- [Google Scholar]
- The adverse effects of obesity on conception and implantation. Reproduction. 2010;140:347-64.
- [Google Scholar]
- Obesity and poor reproductive outcome: The potential role of the endometrium. Fertil Steril. 2007;88:446-51. 10.
- [Google Scholar]
- Impact of body mass index on IVF and ICSI outcome: A retrospective study. Reprod Biomed Online. 2008;16:778-83.
- [Google Scholar]
- Evidence that obesity alters the quality of oocytes and embryos. Pathophysiology. 2008;15:115-21.
- [Google Scholar]
- High and low BMI increase the risk of miscarriage after IVF/ICSI and FET. Hum Reprod. 2008;23:878-84.
- [Google Scholar]
- Body mass index: Impact on IVF success appears age-related. Hum Reprod. 2008;23:1835-9.
- [Google Scholar]
- Should high BMI be a reason for IVF treatment denial? Gynecol Endocrinol. 2017;33:853-6.
- [Google Scholar]
- Does obesity have detrimental effects on IVF treatment outcomes? BMC Womens Health. 2015;15:61.
- [Google Scholar]
- Influence of female bodyweight on IVF outcome: A longitudinal multicentre cohort study of 487 infertile couples. Reprod Biomed Online. 2011;23:490-9.
- [Google Scholar]
- Correlation of body mass index with outcome of in vitro fertilization in a developing country. Arch Gynecol Obstet. 2012;285:259-63.
- [Google Scholar]
- Does obesity really matter? The impact of BMI on embryo quality and pregnancy outcomes after IVF in women aged ≤38 years. Aust N Z J Obstet Gynaecol. 2012;52:270-6.
- [Google Scholar]
- Effect of female body mass index on oocyte quantity in fertility treatments (IVF): Treatment cycle number is a possible effect modifier. A register-based cohort study. PLoS One. 2016;11:e0163393.
- [Google Scholar]
- Body mass index impacts in vitro fertilization stimulation. ISRN Obstet Gynecol. 2011;2011:929251.
- [Google Scholar]
- Overweight and obesity negatively affect the outcomes of ovarian stimulation and in vitro fertilisation: A cohort study of 2628 Chinese women. Gynecol Endocrinol. 2010;26:325-32.
- [Google Scholar]
- Impact of overweight and underweight on assisted reproduction treatment. Hum Reprod. 2004;19:2523-8.
- [Google Scholar]
- Does body mass index of infertile women have an impact on IVF procedure and outcome? J Assist Reprod Genet. 2000;10:547-52.
- [Google Scholar]
- Complications and outcome of assisted reproduction technologies in overweight and obese women. Hum Reprod. 2012;27:457-67.
- [Google Scholar]
- Effect of body mass index on IVF treatment outcome: An updated systematic review and meta-analysis. Reprod Biomed Online. 2011;23:421-39.
- [Google Scholar]
- Effect of body mass index and age on in vitro fertilization in polycystic ovary syndrome. J Turk Ger Gynecol Assoc. 2016;17:83-90.
- [Google Scholar]
- Obesity is associated with increased risk of first trimester and recurrent miscarriage: Matched case-control study. Hum Reprod. 2004;19:1644-6.
- [Google Scholar]
- High and low BMI increase the risk of miscarriage after IVF/ICSI and FET. Hum Reprod. 2008;23:878-84.
- [Google Scholar]
- Does high body mass index increase the risk of miscarriage after spontaneous and assisted conception. A meta-analysis of the evidence? Fertil Steril. 2008;90:714-26.
- [Google Scholar]







