Translate this page into:
Comparative study of intrauterine infusion of autologous platelet rich plasma in unresponsive thin endometrium in frozen ET cycle
Address for correspondence: Dr Zeepee Godha, MS (OBS and GYNAE), Fellow in clinical ART, A 75, Mahesh Nagar, Jaipur-302015, Rajasthan, India. E-mail: zeepee_dr@yahoo.co.in
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Aims:
Study of intrauterine infusion of autologous platelet rich plasma in unresponsive thin endometrium in frozen ET cycle. Thin endometrium still remains a big challenge for clinicians, creating so much burden in the form of cycle cancellation, unplanned freezing of embryo and even need for surrogacy. Intrauterine infusion of platelet-rich plasma (PRP) is newer modality of treatment in thin endometrium, in various studies showing promising results.
Material and methods:
Our study was prospective randomised controlled trial done from 1 August 2018 to 31 May 2019 at a tertiary infertility centre, New Delhi, India. 30 patients undergoing frozen embryo transfer with history of thin endometriun (less than 7 mm) with normal hysteroscopic examination were enrolled. Patients with platelet count less than 1.50000/dl, uncorrected asherman syndrome, submucosal polyp, fibroid or congenital uterine anomaly and with history of systemic diseases were excluded from study. From day 2 of menses tab estradiol valerate was started in dose of 6–8 mg/day. It was increased up to 12 mg/day gradually after reviewing endometrial thickness serially. Patients with thin endometrium on day 10/11 received PRP on day 11 and repeat dose after 48 hours if endometrial thickness was less than 7 mm. Frozen embryo transfer was done in patients who achieved endometrial thickness 7 mm or more.
Results:
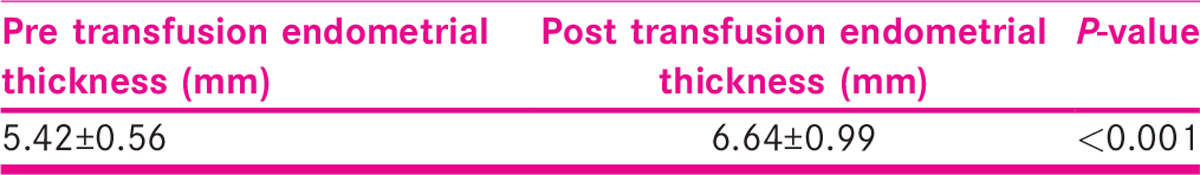
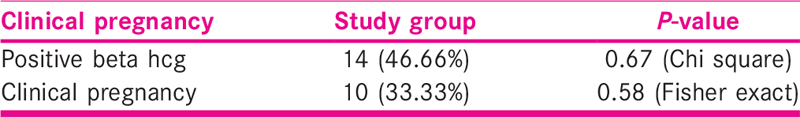
The mean pre-treatment endometrial thickness was 5.42 mm, which significantly increased to 6.64 mm, post treatment (P < 0.001). 8 patients out of 30 in our study could not achieve an optimal pattern of endometrium after treatment and embryo transfer was postponed. The positive beta human chorionic gonadotropin rate was 46.66%, and clinical pregnancy rate was 33.33% which is not statistically significant.
Conclusion:
In this study, we found PRP has effective role in thin endometrial cases.
Keywords
Implantation
platelet-rich plasma
thin endometrium
INTRODUCTION
In humans, implantation is one of the most delicate and synchronised process of attachment and invasion of embryo to the endometrium. It starts with the apposition of maternal and embryonic epithelium, followed by adhesion, penetration and invasion of placental cells deep into the endometrium.[1] For this maternal endometrium undergoes cyclical changes at molecular, biological and morphological levels under the effect of estrogen and progesterone hormone.[2,3,4,5] Endometrium should be in secretory phase for implantation.[6] In frozen embryo transfer cycles, implantation mainly depends on endometrium receptivity and embryo quality and technique of transfer. There is no absolute method to judge the endometrium receptivity. On ultrasonography we can see for endometrium thickness, blood flow and its pattern. Adequate endometrial thickness is essential to achieve clinical pregnancy. It should be more than 7 mm at the time of embryo transfer.[7] There are around 0.6–0.8% cycles of IVF in which embryo transfer is cancelled because of thin endometrium that is less than 7 mm.[8]
Angiogenesis is very important parameter for endometrial growth. Vascular epidermal growth factor (VEGF) is one of the most important mediators for hormonal-dependent endometrium growth.+ It increases the blood flow to uterine endometrium. Increased resistance in uterine redial arteries causes decrease expression of VEGF receptor, resulting poor endometrium growth.[9]
There are various treatments which have been used in patients of thin endometrium as extended estrogen administration, pentoxifylline, vaginal sildenafil, vitamin E, aspirin, human chorionic gonadotropin, gonadotropin-releasing hormone agonist, infusion of granulocyte colony stimulating factor.[10,11,12,13,14,15,16,17] But still thin endometrium remains a challenge for clinicians as it creates so much burden in form of cycle cancellation, unplanned freezing of embryo, even need for surrogacy.
The aim of our study is to evaluate the effect of intrauterine infusion of platelet-rich plasma (PRP) in case of thin endometrium and its impact on endometrial thickness and clinical pregnancy rate
PRP infusion is newer modality of treatment in thin endometrium. PRP is prepared from autologous blood plasma that is concentrated with platelets. It has a unique ability of haemostasis, wound healing and tissue growth.[18,19,20,21,22] It has various clinical applications as in neurosurgeries, oro maxillary surgeries, ortho laryngio head and neck surgeries, cosmetic surgeries, periodontal surgeries, orthopaedic and spinal surgeries, cardiothoracic surgeries and general surgeries.[23] Recently it is also being used in case of thin endometrium with better results and minimal side effects. PRP exerts its effect by degranulation of its granules which contain various growth factors as vascular endothelial growth factor, platelet-derived growth factor, transforming growth factor.[21] PRP also activates other cytokines which promote tissue growth.
MATERIAL AND METHODS
Our study is prospective clinical intervention study, was undertaken at Akanksha IVF centre at Mata Channan Devi Hospital, New Delhi from perio 1 August 2018 to 31 May 2019.
Inclusion criteria
Women aged above 22 years.
Previously cancelled at least one cycle because of thin unresponsive endometrium (<7 mm) during IVF programmes.
Absence of systemic disease as sickle cell disease, chronic neutropenia, known past or present malignancy, renal insufficiency, upper respiratory infection, pneumonia, congenital fructose intolerance, liver dysfunction.
Exclusion criteria
Platelet count less than 150,000/dl.
Use of NSAIDS in last 7–10 days.
Patient on any anticoagulant therapy.
Patients with uncorrected Asherman syndrome, submucosal polyp or fibroid and congenital uterine anomaly.
Patient with recent history of fever or viral illness.
Patient with history of systemic use of corticosteroid in last 2 weeks.
Patient with poor quality of embryos.
All baseline investigations as CBC, blood group, coagulation profile, renal function test, thyroid profile, serum prolactin, HIV, HbsAg, anti HCVAb, VDRL, AMH and husband semen analysis were done when patient enrolled in the study.
Baseline transvaginal ultrasound was done on day 1/2 of menses to check endometrial thickness (ET) and ovarian cyst. Oral contraceptive pills were given for 21 days to the patients who had ovarian cyst of size more than 10 mm and again reviewed on day 2 of next cycle.
From day 1/2 of menses Tab estradiol valerate was started in dose of 6–8 mg/day. It was gradually increased up to 12 mg/day in divided doses after reviewing endometrial thickness serially.
ET is measured in the median longitudinal plane of the uterus, as the maximum distance from one basal endometrial interface across the endometrial canal to the opposite endometrial–myometrial interface with same machine and same operator to minimise subjective error. Using Power Doppler with machine presets for endometrium, vascular pattern was noted. When blood flow was present in the hypoechoic endometrio–myometrial junction, it was graded as zone 1 vascularity. When it was up to the outer hyperechoic line of the endometrium, it was zone 2 vascularity. When it was in the intervening hypoechoic area, it was known as zone 3 vascularity and when blood flow reached the central echogenic line, it was known as zone 4 vascularity.[22] Excellent vascularity was called when patients have at least five signals in zones 3 and 4; patients with up to four signals reaching zone 3 and 4 were termed as modest vascularity and less than one signal in zones 3 and 4 as poor vascularity.
After informed consent patients who have endometrial thickness less than 7 mm on day 10/11 were subjected to intrauterine infusion of autologous PRP on day 10/11. Second dose of PRP was given to those patients who have endometrial thickness less than 7 mm after 48 hrs of first dose.
Frozen embryo transfer was done to the women who achieve endometrial thickness of at least 7 mm with moderate to excellent vascularity after 48 h of last dose of PRP and intravaginal progesterone support was also given to all women who underwent embryo transfer. After 15 days of embryo transfer, we checked for serum beta hcg.
Method of PRP preparation
We take whole blood of 8 ml by venipuncture in acid citrate dextrose tubes (ACD). We centrifuged the blood using a “soft” spin at 300 g for 10 min and then transferred the supernatant plasma containing platelets into another sterile tube (without anticoagulant). We centrifuged the tube again at 300 g for 10 min to obtain a platelet concentrate. The lower 1/3rd is PRP and upper 2/3rd is platelet-poor plasma (PPP). At the bottom of the tube, platelet pellets are formed.
Remove PPP and suspend the platelet pellets in a minimum quantity of plasma (2–4 mL) by gently shaking the tube. Intrauterine infusion is done with the help of IUI catheter under aseptic precaution.
Statistical methods
Statistical testing was conducted with the statistical package for the social science system version SPSS 17.0. The comparison of continuous variables between the groups was performed using Student’s t test. Nominal categorical data between the groups were compared using Chi-squared test. For all statistical tests, a P-value less than 0.05 will be taken to indicate a significant difference.
RESULTS
Intrauterine infusion of PRP is newer modality of treatment in cases of thin endometrium. It is prepared from peripheral vein of autologous blood.
We have enrolled 30 patients in our study after considering inclusion and exclusion criteria.
Table 1 shows clinical characteristics of patients.
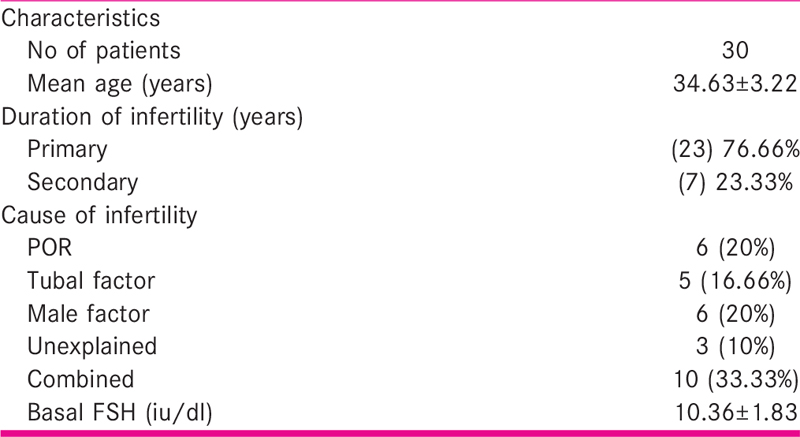
Table 2 shows effect on endometrial thickness pre and post treatment. Increment in endometrial thickness was statistically significant after treatment with PRP in thin endometrium. The mean pre treatment endometrial thickness was 5.42 ± 0.56 mm which was increased significantly to 6.64 ± 0.99 mm, post treatment (P < 0.001). Vascular pattern was also improved.
In 12 (40%) patients it was improved to excellent vascularity from modest vascularity and in 8 (26.66%) patients it was increased to moderate from sparse vascularity [Table 3].
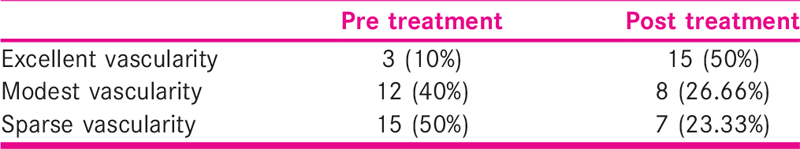
Table 4 shows that 8 patients out of 30 in our study could not achieve an optimal pattern of endometrium after treatment and embryo transfer was postponed.

Table 5 shows that the positive beta human chorionic gonadotropin rate was 46.66% improvement in mean endometrial thickness (1.22 mm) and clinical pregnancy rate was 33.33%, which is not statistically significant. In our study we found that PRP has effective role in thin endometrial cases.
DISCUSSION
PRP has role in improving implantation rate and clinical pregnancy rate with thin endometrium patients. It decreases the cycle cancellation and psychological and financial stress of infertile women. Autologous PRP is very safe, with no side effects, cheap, easily accessible treatment of refractory endometrium.
Zadehmodarres et al.[22] studied the effect of PRP in thin endometrium cases. They found significant increase in endometrial thickness (above 7 mm) in all 10 patients enrolled in their study. Mean pre PRP ET was 4.8 mm which was increased to 7.25 mm after PRP instillation. Chang et al.[11] found that autologous PRP promotes endometrial growth and improve pregnancy outcome in invitro fertilisation patients. They studied the effect of PRP in 5 patients of resistant thin endometrium; they found after 48–72 h of PRP, endometrial thickness was significantly increased and it was above 7 mm in all 5 patients at the day of progesterone administration. Tandulwadkar et al.[23] did a study of autologous intrauterine PRP instillation for suboptimal endometrium in frozen embryo transfer cycles. Total 68 women included in the study, in which 49 women required single sitting of PRP, whereas 19 women required two sittings of intrauterine PRP infusion. The mean pre-PRP ET was 5 mm and the post-PRP ET was 7.22 mm (P < 0.00001).
These results are similar to our study. Our pre PRP ET was 5.38 ± 0.57 mm which was increased significantly to 6.62 ± 0.98 mm. PRP is also effective in corrected Asherman syndrome. In study of Chang et al.[11] one patient had partial Asherman syndrome, hysteroscopically adhesiolysis was done and again hysteroscopy was done before starting the cycle, which was normal. Pre PRP ET was 5.9 mm which was increased to 7 mm after PRP.
PRP prepared from autologous plasma is 4–5 times more in concentration in platelets. Release of granular content of platelet causes large amount of cytokines, growth factor as VEGF, TGF, PDGF, EGF, FGF, IGF 1 and 2, CTGF, interleukin 8 in endometrium and help in endometrium proliferation, remodelling and angiogenesis. Endometrium has important role in implantation and clinical pregnancy. Intrauterine infusion of autologous PRP is also associated with improvement in clinical pregnancy rate. In our study we found clinical pregnancy rate 33.33% after PRP infusion. In study of Tendulwadkar et. al.[23] they found positive beta hcg rate was 60.93% and clinical pregnancy rate was 45.31% after intrauterine infusion of PRP in suboptimal endometrium in frozen embryo transfer cycle. Frozen embryo transfer was done in 64 patients out of 68. Among them 13 were in second trimester, 13 were in first trimester, one had ectopic pregnancy, 3 had blighted ovum, 2 had missed abortion and two had biochemical pregnancy (23).
In the study of Chang et al.[11] platelet rich plasma administration has benefit for infertile women with thin endometrium in frozen blastocyst-stage embryo transfer programme implantation rate was 27.94%, clinical pregnancy rate was 44.12% while in control it was 11.67% and 20% respectively. Both these results were statistically significant (P<0.05). In study of Zadehmodarres et al.[23] intrauterine infusion of PRP in thin endometrium patients found chemical pregnancy in 50% cases and clinical pregnancy rate was 40%. These results are slightly higher than our study. In our study PRP was associated with significant improvement in endometrial thickness in cases of thin endometrium. It is effective within 48–72 h after infusion. While in other treatment option as vitamin E, pentoxyphylline, extended estrogen therapy, the duration of treatment is very long so drop out rate is more. In other treatment option as sildenafil, low dose aspirin mainly increase the vascularity while GCSF and PRP have proliferative action along with increasing angiogenesis. Role of stem cell therapy in thin endometrium and in recurrent implantation failure is in research stage, practical utility has not established yet.
CONCLUSION
Thin endometrium still remains one of the challenging situation for clinicians to treat. In most of the patients, no etiological factor is present for its cause and resistance to traditional treatment. PRP has promising results in cases of thin endometrium. It has direct effect on endometrial growth and increases its vascularity also. It is easily available and free of any side effects. They also have role in implantation, although results are not significant. Large studies at multiple centres needed to find out and establish the effect of PRP and G-CSF in thin endometrium and in implantation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Principles and practice of assisted reproductive technology (second). The Health Science Publisher; 2018. p. :103.
- Early pregnancy losses in in vitro fertilization and oocyte donation. Fertil Steril. 1999;72:106.
- [Google Scholar]
- In vitro fertilization plus preimplantation genetic diagnosis in patients with recurrent miscarriage: an analysis of chromosome abnormalities in human preimplantation embryos. Fertil Steril. 1999;71:1033-9.
- [Google Scholar]
- Human implantation: the last barrier in assisted reproduction technologies? Reprod Biomed Online. 2007;14:5-22.
- [Google Scholar]
- Thin endometrium in assisted reproductive technology. Curr Opin Obstet Gynecol. 2008;20:221-8.
- [Google Scholar]
- The relationship between endometrial thickness and outcome of medicated frozen embryo replacement cycles. Fertil Steril. 2008;89:832-9.
- [Google Scholar]
- The correlation between endometrial thickness and outcome of in vitro fertilization and embryo transfer (IVF-ET) outcome. Reprod Biol Endocrinol. 2008;6:37.
- [Google Scholar]
- A randomized clinical trial of endometrial perfusion with granulocyte colony-stimulating factor in in vitro fertilization cycles: impact on endometrial thickness and clinical pregnancy rates. Fertil Steril. 2014;101:710-5.
- [Google Scholar]
- Autologous platelet-rich plasma promotes endometrial growth and improves pregnancy outcome during in vitro fertilization. Int J Clin Exp Med. 2015;8:1286-90.
- [Google Scholar]
- Transvaginal perfusion of G-CSF for infertile women with thin endometrium in frozen ET program: a non-randomized clinical trial. Iran J Reprod Med. 2014;12:661-6.
- [Google Scholar]
- Successful treatment of unresponsive thin endometrium. Fertil Steril. 2011;95:e13-7.
- [Google Scholar]
- A pilot cohort study of granulocyte colony-stimulating factor in the treatment of unresponsive thin endometrium resistant to standard therapies. Hum Reprod. 2013;28:172-7.
- [Google Scholar]
- What is the optimal means of preparing the endometrium in frozen-thawed embryo transfer cycles?A systematic review and meta-analysis. Hum Reprod Update. 2013;19:458-70.
- [Google Scholar]
- Treating patients with "thin" endometrium—an ongoing challenge. Gynecol Endocrinol. 2014;30:409-14.
- [Google Scholar]
- Two protocols to treat thin endometrium with granulocyte colony-stimulating factor during frozen embryo transfer cycles. Reprod Biomed Online. 2015;30:349-58.
- [Google Scholar]
- Bone growth factors in maxillofacial skeletal reconstruction. Int J Oral Maxillofac Surg. 2002;31:469-84.
- [Google Scholar]
- Platelet-rich fibrin: Evolution of a second-generation platelet concentrate. Indian J Dent Res. 2008;19:42-6.
- [Google Scholar]
- Platelet-rich plasma: where are we now and where are we going? Sports Health. 2010;2:203-10.
- [Google Scholar]
- Comparison of methods for point of care preparation of autologous platelet gel. J Extra Corpor Technol. 2004;36:28-35.
- [Google Scholar]
- Treatment of thin endometrium with autologous platelet-rich plasma: a pilot study. JBRA Assis Reprod. 2017;21:54-6.
- [Google Scholar]
- Autologous intrauterine platelet-rich plasma instillation for suboptimal endometrium in frozen embryo transfer cycles: a pilot study. J of Hum Reprod Science. 2017;10:208-12.
- [Google Scholar]







