Translate this page into:
Comparison of a “freeze-all” strategy versus a “fresh transfer” strategy among poor responders in Assisted Reproductive Technology (ART)—An observational study
Address for correspondence: Dr Manvi Tyagi, MBBS, MS (Obst and Gynaec), Fellow (Diploma in Clinical ART), B-226, Sector 71, Noida, Uttar Pradesh. E-mail: manvityagi226@gmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
In recent years, frozen embryo transfer has been used by many and it may be a viable alternative to frozen embryo transfer (FET). So far, most of the studies were done to prove effectiveness of “freeze all” strategy in normal responder, very few had focused this policy on poor responder.
Aims:
To find clinical pregnancy rate (CPR) in frozen cycle versus fresh cycle embryo transfer (ET) in poor responder.
Settings and design:
Prospective observational study performed at our private fertility clinic.
Methods and materials:
From August 2018 to April 2019, a total of 102 poor responder patients who met POSEIDON criteria were included in the study out of which 50 were in FET group and 52 were in frozen thaw group. Controlled ovarian stimulation (COS) with gonadotropin releasing hormones (GnRH) antagonist protocol was done. Measured primary outcome was CPR in both groups.
Statistical analysis used:
Paired t test, chi square test, Z test, and Student t test were used.
Results:
Statistical analysis showed that the CPR in the frozen embryo group was 46.15%, while in the FET group it was 24.0%. The proportional comparison among the two groups was found to be statistically significant (P = 0.016), showing a higher CPR in the FET group.
Conclusion:
Success of IVF treatment can be improved in poor responder by implementing “freeze all” policy. RCT with large number of patients should be carried out to confirm this finding.
Keywords
Freeze-all policy
fresh embryo transfer
frozen-thaw embryo transfer
in vitro fertilization
Key message: With the recent advancements in Assisted Reproductive Technology (ART), we understand that we are not far from good culture and blastocyst vitrification in poor ovarian responders to gain better result.
INTRODUCTION
The use of Assisted Reproductive Technique (ART) for treatment of infertility is increasing all over the world, recently.[1] The standard procedure in ART is the use of frozen embryo transfer (FET) which has stood the test of time. But in recent years, frozen embryo transfer (eFET) has also been used by many quite successfully and it may be a viable alternative to FET. With the advent of better vitrification technique and endometrial receptivity concept, there is significant rise in IVF outcome (in terms of implantation rate (IR), clinical pregnancy rate (CPR), and ongoing pregnancy rate (OPR)) with “Freeze all” policy. Ovarian Hyper Stimulation Syndrome (OHSS) can be prevented as an added benefit of this policy.[2] Keeping in mind such advantages, objective of this study is to compare the “freeze-all” strategy with same cycle transfer strategy among poor responders in ART.
SUBJECTS AND METHODS
Inclusion criteria
All the patients who were presented to our IVF center for fertility treatment meeting the POSEIDON criteria for POR were included in this study.
Day 5 embryo transfer in gonadotropin releasing hormones (GnRH) antagonist cycles.
Fresh and frozen thawed ET done with good quality embryos according to Gardner blastocyst grading system, that is, blastocyst cavity expansion larger than the embryo, along with thinning of the shell (4AA, 4AB).
Exclusion criteria
Endometriosis stage 3 to 4
Ovarian cysts with a diameter more than 30 mm found on the starting day of stimulation
Congenital/ acquired defect of uterus
Fibroids (submucosal)
Presence of severe co-morbidity (uncontrolled diabetes, cardiovascular, pulmonary, or any major system illness)
Uncontrolled thyroid disease
Contraindications or allergies to gonadotropins or GnRH antagonists
Ovum donor cycle
Primarily male factor infertility (for e.g. severe oligozoospermia < 1million/mL, or azoospermia; asthenozoospermia etc.)
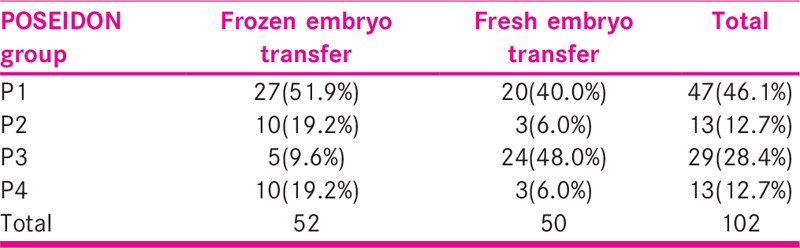
We have enrolled 102 poor responder patients (POSEIDON groups 1 to 4) between the ages 22 and 40 year [Table 1]. All participants attended our fertility clinic between August 2018 and April 2019. Ovarian stimulation with GnRH antagonist protocol was used in both the groups. Stimulation was performed using combination of Inj. rFSH (Gonal F, folligraft) and Inj.HMG (Gynogen), maintaining the physiological synergy of follicle stimulating hormone (FSH) and leuteinizing hormone (LH) ratio of 2:1, which was started on day 2 or 3 of menses. Follicular monitoring, human chorionic gonadotropin (HCG) trigger, and ovum pick up was done as per protocol. After 3–4 hr of ovum pick up, intra cytoplasmic sperm injection (ICSI) was performed and further embryo growth was monitored with time lapse technique. Grading of embryo was done with “Gardner” blastocyst grading system. In the fresh transfer group (n = 50), transfer of embryo was performed only when progesterone levels were ≤1.5 ng/mL and the endometrium was 7 mm or more on the day of trigger. Those patients were included in the freeze-all group (n = 52) who had all the embryos cryo-preserved in the fresh cycle and the first embryo transfer was performed after priming the endometrial and embryo thawing. The freeze-all strategy was applied when the E2 levels were > 3000 picogram/ml or more than twenty follicles were seen in both the ovaries, serum level of progesterone was more than 1.5 ng/mL, and the endometrium was less than 7 mm in thickness on the day of trigger. After ET, luteal phase support was given as per protocol. Primary outcome was measured in form of clinical pregnancy which is defined as confirmation of pregnancy by both, high level of serum beta HCG that is more than 10 IU and gestational sac’s presence along with cardiac activity of fetus 30 days after the embryo transfer, seen by USG. Ongoing pregnancy was the secondary outcome; which is defined as viable intrauterine pregnancy of at least 12 weeks duration confirmed on an ultrasonography scan.
RESULTS
Statistical analysis was done with the Statistical Package for Social Sciences (SPSS version 24.0). Statistical software was used for calculating the P values. Comparison of mean between the two groups was done using Unpaired ‘t’ test and comparison of proportions between the two groups was done using Z test for two sample proportion. A P-value of less than 0.05 was considered as statistically significant. The final data were presented in the form of tables and graphs.
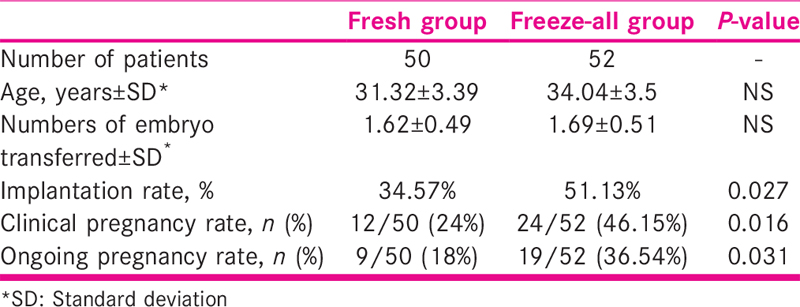
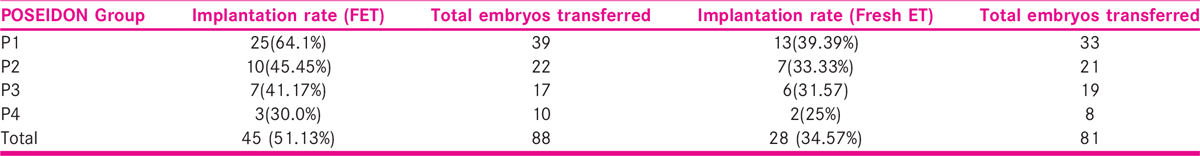
Implantation, clinical pregnancy, and ongoing pregnancy rates were higher in frozen ET group (51.1%, 46.1%, 36.5%, respectively) compared to fresh ET group (34.5%, 24%, 18% respectively), this difference was statistically significant (P = 0.02) [Table 2, Figures 1 and 2].
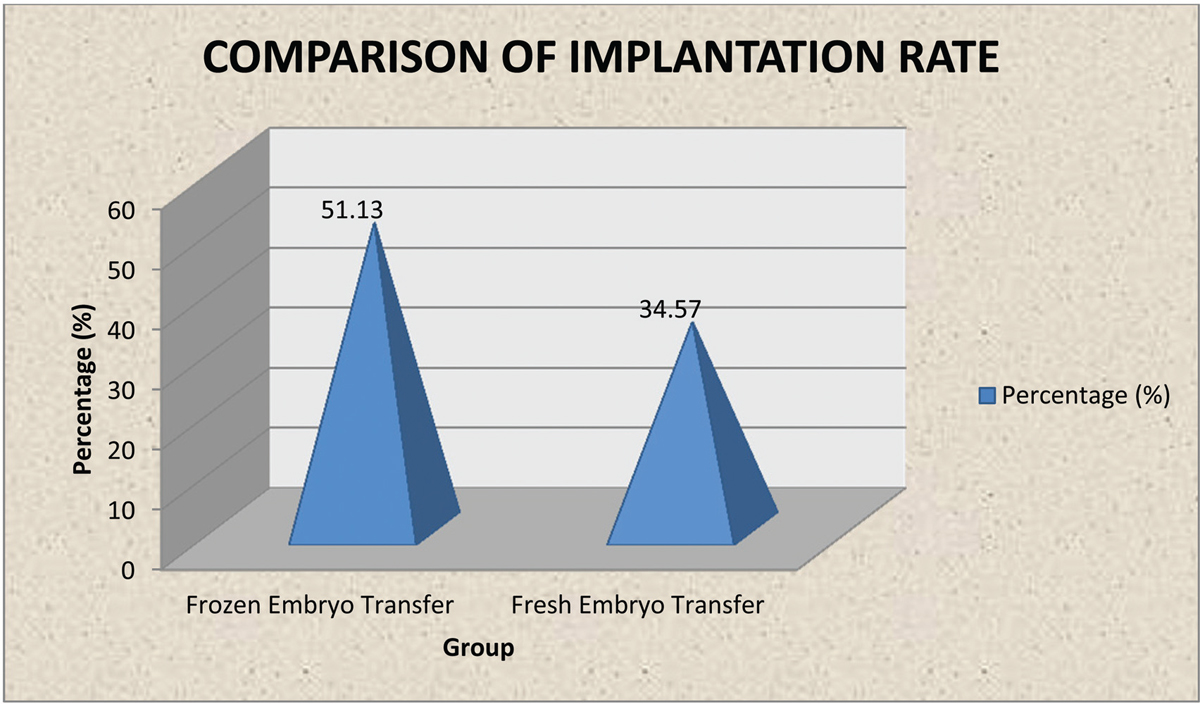
- Graph comparing implantation rate.
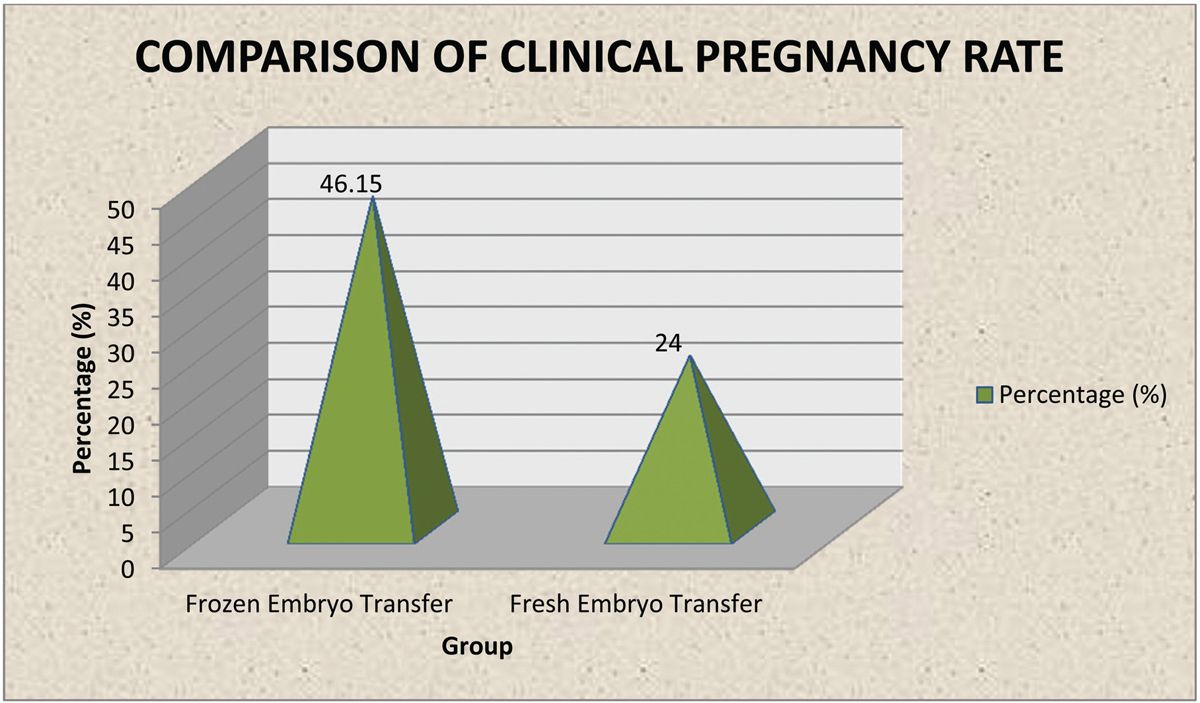
- Graph comparing clinical pregnancy rate.
In POSEIDON group 1, the implantation rate was 64.1% in the FET group and 39.39% in fresh ET group. The results of other POSEIDON groups were also better among the FET group as compared to fresh ET [Table 3].
DISCUSSION
In our study we have found that there is a significant difference in IR, CPR, and OPR between fresh and frozen thaw embryo transfer (FET) groups. It has been noted that implantation failure in early pregnancy is due to increased levels of PG released due to oocyte retrieval procedure in fresh embryo transfer cycle.[3,4] It is also postulated that PG rise is responsible for early onset OHSS.[5,6] Because of these reasons it has been theorized that FET cycles are similar to natural cycles and therefore gives better result. In present study the mean age of patients in FET group and fresh embryo transfer group was 34.04 ± 3 and 31.3 ± 3 years respectively. In patients with advanced age, we have chosen frozen cycle transfer as it mimics natural physiology of implantation resulting in reduced abortion rate.[5,6] Poor responder patients belonging to higher maternal age group that is >35 years can be benefited from pre implantation genetic screening test, as aneuploidy rate significantly increases in advanced maternal age.[7] The supra-physiological effects of the exogenous hormone administration in fresh ET cycle may adversely affect the implantation resulting in higher rates of miscarriage. As higher serum levels of estradiol (>2500 pg/ml) may affect endometrial maturation and implantation; there are lower chances of pregnancy rates in these cycles.[8,9,10]
In our study we noted higher implantation rate in FET cycle as compared to fresh embryo transfer group (51.13% vs 34.5%) which is statistically significant. Celik et al.[11] reported no obvious difference in respect to IR in same cycle and frozen transfer cycle. However, in this study cleavage stage ET was done in fresh cycle whereas blastocyst stage transfer was done in FET cycle. Higher implantation rates were found by Zhu et al.[12] in FET cycles as compared to fresh embryo transfer cycles. Clinical pregnancy rates and implantation rates were 36.4% and 25.2% respectively in fresh cycle whereas, 55.1% and 37.5% in frozen group which is statistically significant. Murat Berkanoglu et al.[13] had studied optimal embryo transfer strategy in poor responders including freeze all. The study showed IR of 24.1% in freeze cycle transfer and 47% in frozen ET cycle which was statistically significant and supports our study. In our study clinical pregnancy rates and ongoing pregnancy rates were 46.1% and 36.1% respectively in FET cycle while 24% and 18% in fresh cycle, which is statistically significant and supported by aforementioned study done by Murat et al. With the recent advancements in ART like vitrification technique and cryopreservation technique we understand that we are not far from good culture and blastocyst vitrification in poor ovarian responders to gain better result. It is believed that future controlled ovarian stimulation (COS) strategy will enhance the chances of more competent oocyte in patients with poor ovarian reserve which can result in clinical pregnancy rates comparable with that of normal responder patients.
We have concluded from our study that in poor responder group of patients IVF outcomes can be improved by implementing freeze all policy, as significantly higher rate of implantation, clinical pregnancy, and ongoing pregnancy was observed in this group. This may be due to the negative effect of exogenous gonadotropins in ART cycle over the endometrium which gets prevented following freeze all policy. Major concern in poor responder patients is reduced oocyte competence due to availability of lesser oocyte. Therefore better outcomes could be achieved with the help of pre implantation genetic screening synchronized with latest endometrium receptivity markers which is only possible with freeze all policy.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Assisted reproductive technology in Europe, 2012: results generated from European registers by ESHRE. Hum Reprod. 2016;31:1638-52.
- [Google Scholar]
- Cryopreservation of human embryos by vitrification or slow freezing: a systematic review and meta-analysis. Fertil Steril. 2008;90:186-93.
- [Google Scholar]
- Increased decidual prostaglandin E concentration in human abortion. Br J ObstetGynaecol. 1983;90:958-60.
- [Google Scholar]
- Suppression of concentration of endometrial prostaglandin in early intra-uterine and ectopic pregnancy in women. J Endocrinol. 1980;85:379-86.
- [Google Scholar]
- Early and late ovarian hyperstimulation syndrome: early pregnancy outcome and profile. Hum Reprod. 2005;20:636-41.
- [Google Scholar]
- Pregnancies conceived using assisted reproductive technologies (ART) have low levels of pregnancy-associated plasma protein-A (PAPP-A) leading to a high rate of false-positive results in first trimester screening for Down syndrome. Hum Reprod. 2009;24:1330-8.
- [Google Scholar]
- Obstetric and perinatal outcomes in singleton pregnancies resulting from the transfer of frozen-thawed versus fresh embryos generated through in vitro fertilization treatment: a systematic review and meta-analysis. Fertil Steril. 2012;98:368-77.
- [Google Scholar]
- Clinical evidence for a detrimental effect on uterine receptivity of high serum oestradiol concentrations in high and normal responder patients. Hum Reprod. 1995;10:2432-7.
- [Google Scholar]
- Increasing uterine receptivity by decreasing estradiol levels during the preimplantation period in high responders with the use of a follicle-stimulating hormone step-down regimen. FertilSteril. 1998;70:234-9.
- [Google Scholar]
- Increasing levels of estradiol are deleterious to embryonic implantation because they directly affect the embryo. Fertil Steril. 2001;76:962-8.
- [Google Scholar]
- The effects of fresh embryo transfers and elective frozen/thawed embryo transfers on pregnancy outcomes in poor ovarian responders as defined by the Bologna criteria. Turk J Obstet Gynecol. 2015;12:132-8.
- [Google Scholar]
- Vitrified-warmed blastocyst transfer cycles yield higher pregnancy and implantation rates compared with fresh blastocyst transfer cycles–time for a new embryo transfer strategy? Fertil Steril. 2011;95:1691-5.
- [Google Scholar]
- Optimal embryo transfer strategy in poor response may include freeze-all. J Assist Reprod Genet. 2017;34:79-87.
- [Google Scholar]







