Translate this page into:
Knowledge, attitude, and practice regarding fertility preservation among specialists involved in the care of cancer patients
Address for correspondence: Shefali Wadhwani, House no. 1048, Sector 37 - B, Chandigarh 160036, India. E-mail: drshefaliwadhwani.sharma@gmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Aim:
To evaluate knowledge, attitude, and practices (KAP) regarding fertility preservation among various doctors involved in treatment and care of cancer patients and identify the potential barriers for the discussion of fertility preservation with patients.
Settings and design:
A survey-based cross-sectional study conducted in a tertiary ART centre in Northern India (Jindal IVF & Sant memorial nursing home, Chandigarh).
Materials and methods:
The study involved Gynecologists, Infertility specialists, Radiotherapists, General Surgeons and Oncologists from multiple institutions. The survey included a questionnaire consisting of 20 items. The study was closed after receipt of the first 201 responses. The responses to questions were analysed by the standard statistical method using SPSS- 22.
Results:
The knowledge among respondents from all specialties regarding impact of cancer treatment on fertility was very high. The rates of knowledge regarding various fertility preservation (FP) options were variable, least knowledge regarding the transposition of ovaries/gonads, testicular tissue cryopreservation, fertility-sparing chemotherapy. There were variations in clinician’s attitude and practice regarding various fertility issues of the patient and fertility preservation based on the specialty of clinicians. Nearly three-fourth discuss various FP options but only one-third provide written information on the same. The referral practice for FP was variable and was influenced by many factors. The factors considered most important for barriers to fertility preservation are Socioeconomic status/cost and affordability issues, 75.1% (patient factor), prognosis, type of cancer and type of treatment 60.2%, (clinician’s consideration).
Conclusion:
To improvise utilization of fertility preservation services, the deficit in clinician’s knowledge should be circumvented by providing them with basic, advanced, and up to date information particularly among primary contact clinicians of cancer patients. The referral pathways should be defined and made clear.
Keywords
Barriers to fertility preservation
fertility preservation
KAP studies regarding fertility preservation
oncofertility
INTRODUCTION
Fertility is one of the key aspects of quality of life for young cancer patients and survivors and hence it should be protected and preserved.[1] Fertility preservation (FP) is receiving increasing attention as an evolving area of reproductive medicine and it aims to protect, preserve, and store gametes and/or reproductive tissue for future use.[2] There is still a huge lacuna in fertility preservation services and so there is an urgent need for priming, spreading awareness, and educating specialist doctors involved in the treatment of cancer about fertility preservation and its advantages. Currently, not many studies exist in India that question the knowledge and attitude of professionals towards the discussion of fertility preservation with the patients.
Aims of the Study
To evaluate knowledge of, attitude to, and practice behavior regarding fertility preservation among various doctors involved in the treatment and care of cancer patients.
To identify the potential barriers to the discussion of fertility preservation with patients.
To create awareness regarding fertility preservation.
MATERIALS AND METHODS
It is a survey-based cross-sectional study conducted over a period of 7 months from August 1, 2019 to March 31, 2020 at a North Indian tertiary care infertility clinic, Jindal IVF Centre, Chandigarh. The consent and completed survey consisting of a structured questionnaire was obtained online through a link by a mobile application (Google forms) or on paper. The sample size by formula had not been calculated since it was a time-bound survey-based study conducted over a period of 7 months. All gynecologists, infertility specialists, radiotherapists, general surgeons, and oncologists were sent questionnaires of which 201 responded.
Inclusion Criteria
All gynecologists, infertility specialists, radiotherapists, general surgeons, and oncologists that gave consent to participate in the study.
The minimum qualification was post-graduation (completed or pursuing). The designation of the respondents was categorized into junior resident (those who were pursuing post-graduation), senior resident (pursuing residency after completion of post-graduation for 3 years), junior consultant (designation after completing 3 years of senior residency for 7 years or assistant professor in a medical college), senior consultant (associate professor, professor in a medical college or 7 years post junior consultancy in a private hospital), and head of the institute/unit (head of the department or unit in a medical college or private hospital).
Study Questionnaire
The survey included a questionnaire evaluating awareness, attitude, knowledge of, and practice behavior toward fertility preservation among these specialists. After requesting participation in the survey, the questionnaire was circulated to more than 200 specialists.
In this study, 20 point questions were selected to fit the following three domains other than participant’s demographics: Knowledge and Awareness, Attitude and Practice behavior, and Barriers of Fertility preservation. A questionnaire was developed based on items from various sources. Selected items were adapted to fit in the setting of the current study. Two senior gynecologist and infertility specialists reviewed the questionnaire to evaluate its validity leading to some additional modifications.
Knowledge and awareness were assessed by six items that measure knowledge about the risk of infertility because of cancer treatment, need for fertility preservation in male and female cancer patients, various fertility preservation methods, and awareness regarding the American Society of Clinical Oncology (ASCO) guidelines on Fertility preservation. Response alternatives were categorized into “Not at all Knowledgeable,” “Aware but do not know well,” “Slightly knowledgeable,” “Knowledgeable,” and “Very knowledgeable.”
Practice behavior of the clinicians was evaluated using eight items. Physicians indicated the level of agreement with the statements based on their clinical practice. The items evaluate how frequent and the extent to which physicians explained to their patients the gonadotoxic impact of cancer treatment and risk of infertility; to what extent they discussed various fertility preservation options available and if they provided any written information on the same. It enquired participants to what extent they considered fertility as an important quality of life issue and; how considerate were they of patient’s desire for future fertility while planning cancer treatment regimen. It tends to assess that to what extent is fertility preservation a high priority for their cancer patients. It interrogated how frequently they consulted specialists from other fields with queries about fertility issues of their cancer patients and how frequently they referred patients who have queries regarding fertility or want fertility preservation to a fertility specialist. Responses were given on a 5-point Likert scale ranging from “Never” to “Always” with the additional alternative “Not applicable”. Responses were categorised into “Never,” “Rarely,” “Sometimes,” “Usually,” and “Always” in order to facilitate the analysis and interpretation of the results.
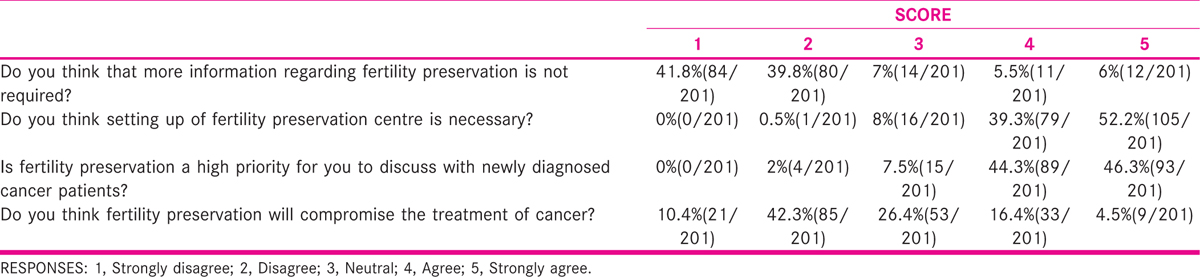
Attitudes were measured by asking physicians to indicate their level of agreement with four questions that enquire if they think that more information regarding fertility preservation is not required; whether they think that setting up of fertility preservation center is necessary; is fertility preservation a high priority for them to discuss with newly diagnosed cancer patients and whether they think that fertility preservation will compromise cancer treatment. Responses ranged from 1 (“Strongly disagree”) to 5 (“Strongly agree”), and were categorized into “Disagree,” “Neutral,” and “Agree.”
Barriers of not initiating a discussion on fertility preservation (Patient Factors and clinician’s perspective) were measured by asking them to mark one or more options they considered to be a barrier under each category, patient factors and clinician considerations. Multiple selections were allowed. They could cite reasons other than those mentioned in the options provided.
Data about the participants’ demographics and clinical background included name, age, sex, marital status, having children or not, specialization, years of experience, designation, type of hospital, and level of care.
Statistical Analysis
The data were collected using Google Spreadsheets for all participants and was described in terms of range frequencies (number of cases) and relative frequencies (percentages) as appropriate after the division of the participants into various categories depending upon age, sex, marital status, having children, specialty, designation, type and level of care at hospital, and duration of the experience. As the responses of participants were nonmetric category, these were compared using a Cross-tab method with Pearson chi-square test. All P values are two-sided, with a statistical level of significance set at P < 0.05. All statistical calculations were done using SPSS 22.0 (Statistical Package for the Social Science) for Microsoft Windows.
OBSERVATION AND RESULTS
The total number of respondents in our study were 201. The demographic profile of the respondents is depicted in Figure 1.
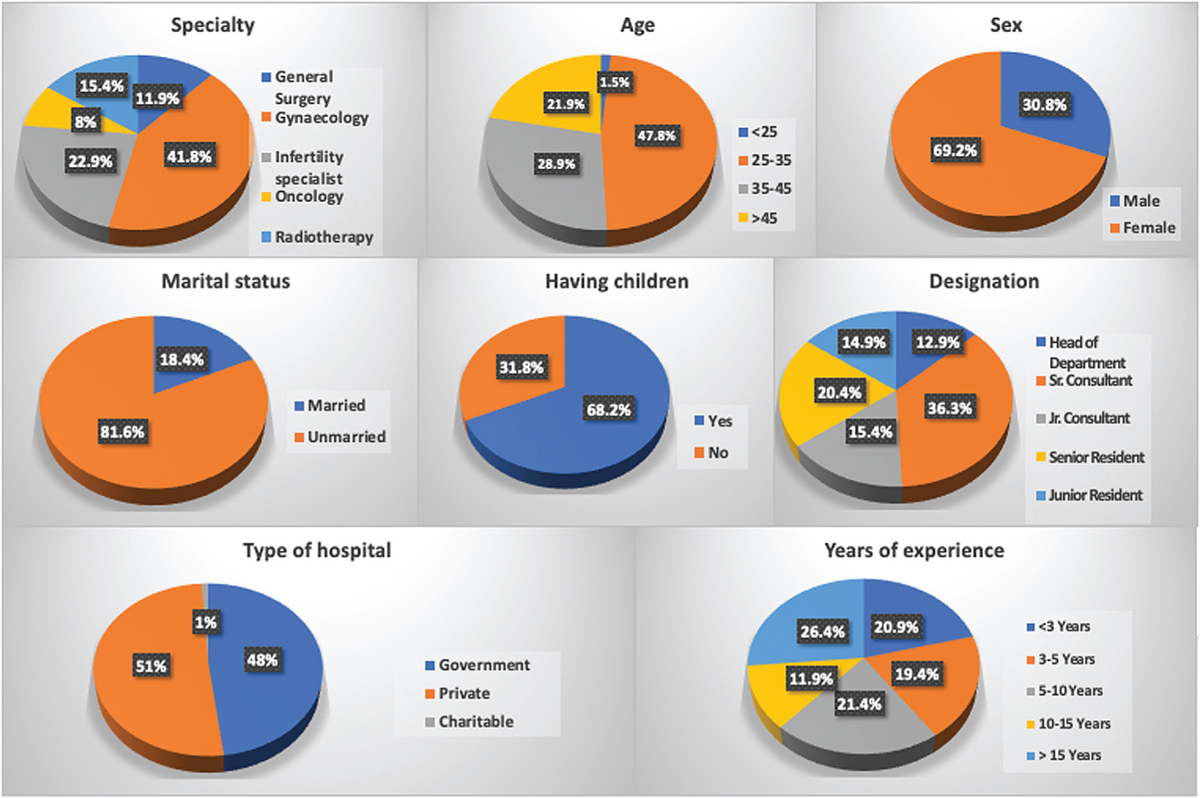
- Demographics of respondents.
Knowledge and Awareness about Fertility Preservation
The knowledge among respondents regarding the impact of radiotherapy and chemotherapy on a patient’s fertility was very high. The responses by respondents to questions evaluating knowledge and awareness regarding FP are depicted in Table 1 and Figure 2. Of the respondents, 87.5% of oncologists, 65% of infertility specialists, 33% of gynecologists, and 45.1% of radiotherapists reported that they were ‘very knowledgeable, whereas only 29.1% of general surgeons reported being “very knowledgeable” and the difference was significant (P = 0.004).
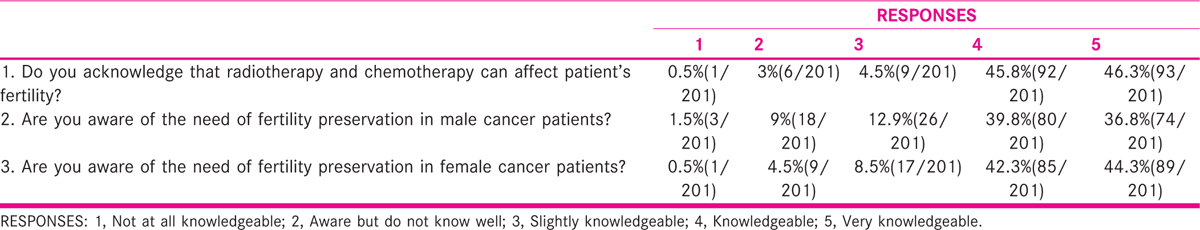
- Are you aware of the following fertility preservation options.
The respondents were “very knowledgeable” or “knowledgeable” about fertility preservation in male cancer patients (76.6%) and in female cancer patients (86.6%). The fertility of respondents had a significant bearing on awareness (P = 0.001).
Nearly 90% of infertility specialists, oncologists, and radiotherapists reported that they were “knowledgeable” or “very knowledgeable” about male and female fertility preservation but only 62.5% of General surgeons and 64.2% of Gynecologists reported so. There was a statistically significant difference in knowledge regarding male FP among respondents based on their marital status (P = 0.01), designation (P = 0.021), and experience (P = 0.042).
There was a statistically significant difference in knowledge (P = 0.002) about female fertility preservation based on the designation of the respondents. Consultants were more knowledgeable than junior residents and senior residents. About 56.6% of junior residents and 60.9% of senior residents responded being “knowledgeable” or “very knowledgeable” while 76.4% of head of the departments, 90.4% of senior consultants, and 83.8% junior consultants responded being “knowledgeable” or “very knowledgeable.” There was a statistically significant difference in knowledge regarding female FP based on age (P = 0.009), marital status (P = 0.019), specialty (P = 0.000), and experience (P = 0.032).
The level of awareness among respondents regarding various fertility preservation options was variable and is shown in Figure 2. The transposition of ovaries/gonads, testicular tissue cryopreservation, and fertility-sparing chemotherapy were the least known.
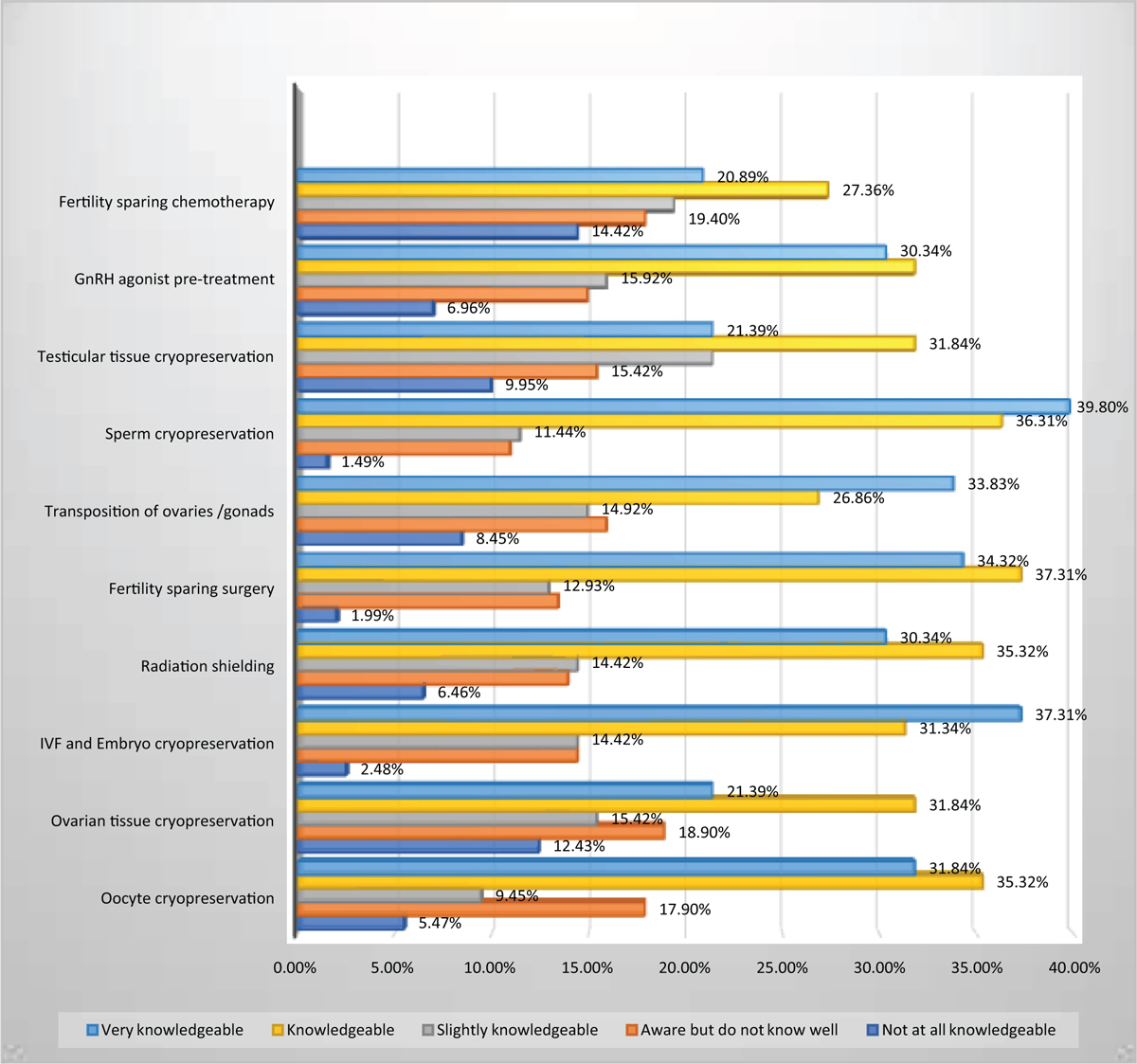
The awareness regarding the ASCO guidelines on FP is shown in Figure 3. The level of awareness was the highest among oncologists (68.75%) and infertility specialists (67.3%) followed by gynecologists (51.1%) and radiotherapists (48.3%), and least among general surgeons (12.5%). There was a statistically significant difference in the level of awareness between males (35.5%) and females (58.3%; P = 0.003).
- Awareness regarding ASCO guidelines on FP. ASCO, American Society of Clinical Oncology; FP, fertility preservation.
Practice Behavior
There were eight items in the questionnaire that evaluated respondents’ practice behavior toward fertility preservation and responses are shown in Table 2. Of 75% respondents that “always” or “usually” discuss fertility preservation options, 93.4% were infertility specialists, 87.5% were oncologists, 74.1% were radiotherapists, 62% were gynecologists, and 37.5% were general surgeons, and this difference was statistically significant (P = 0.002). Age of the clinician had an influence on attitude or practice of consulting clinicians from other specialty, being highest in the age group of more than 45 years (72.7%) and 35 to 45 years (72.4%), followed by age group of 25 to 35 years (47.9%), and least in the age group of less than 25 years (33.3%; P < 0.003). Females (71.2%) were twice more likely to consult than males (35.2%). Married clinicians (66.4%) are almost twice more likely to consult with specialists from other specialty than clinicians who are single (32.4%). This difference was statistically significant (P = 0.001). The respondents that were having children tend to consult more often than those who did not have children (70.8% and 37.5%, respectively). Out of all the clinicians, 52.1% of infertility specialists, 38.1% of gynecologists, 31.2% of oncologists, 12.9% of radiotherapists, and 4.1% of general surgeons “always” consult.
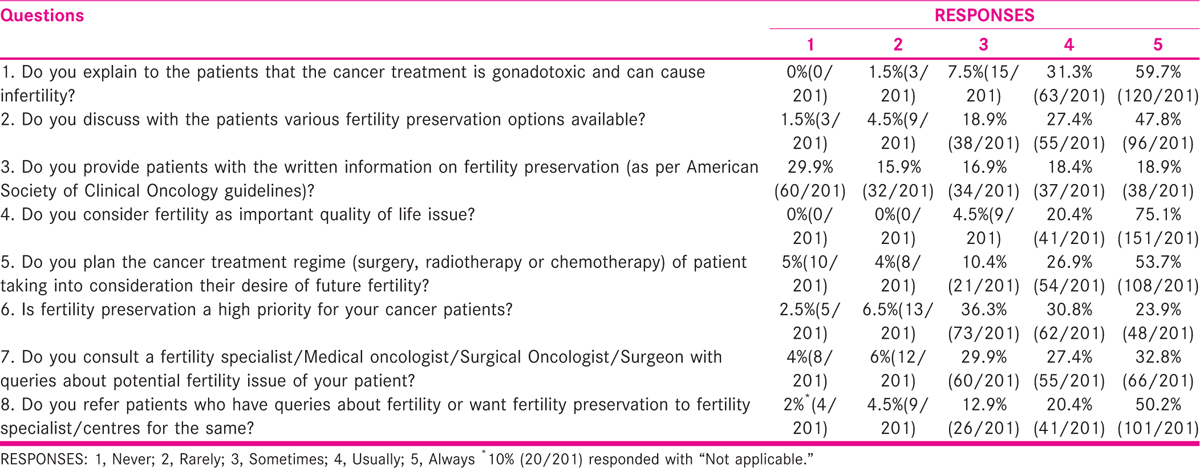
Out of 70.6% respondents who “always” or “usually” referred patients for FP, 93.7% were oncologists, 75% were gynecologists, 70.9% were radiotherapists, 60.8% were infertility specialists, and 58.3% were general Surgeons. There was a statistically significant difference (P = 0.003) in referral practice among clinicians who were married or single. Married clinicians (73.7%) tend to refer more frequently (those who responded with “always” or “usually”) than single clinicians (56.7%).
Attitude Toward Fertility Preservation
The attitude of the respondents regarding fertility preservation was evaluated by four items and is shown in Table 3. Out of 91.5% who “strongly agree” or “agree” regarding the necessity of setting up an FP center, 68.75% were oncologists, 67.3% were infertility specialists, 61.2% were radiotherapists, 47.6% were gynecologists, and 16.6% were general surgeon (P = 0.003).
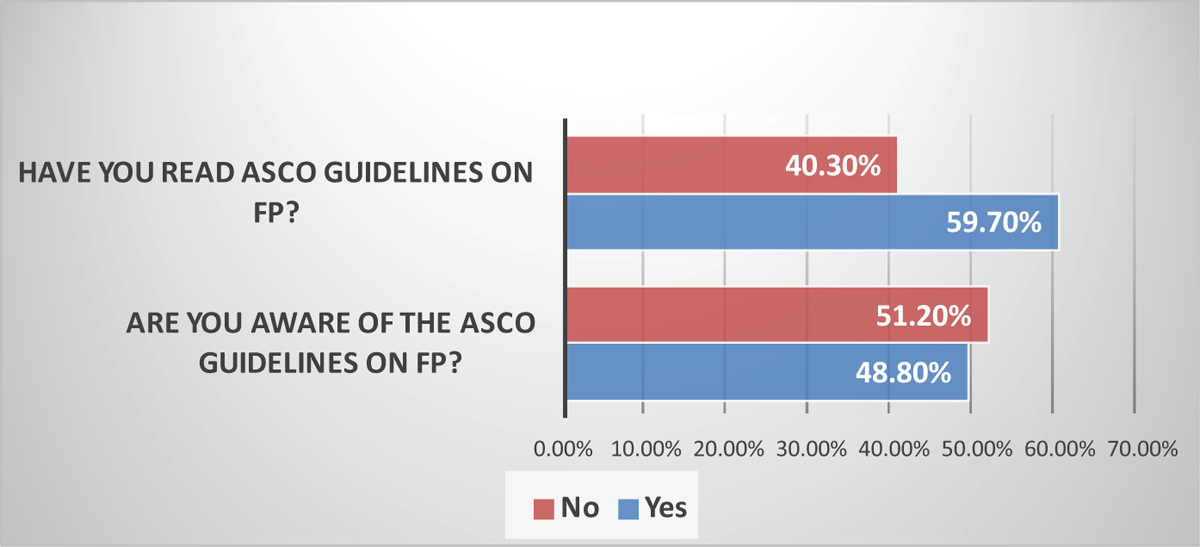
Barriers of Fertility Preservation
The clinicians were asked what “patient factors” and “clinician’s considerations” according to their belief are the barriers to initiating a discussion on FP and for not referring the patients to a specialist for undergoing FP. The results are as shown in Figures 4 and 5.
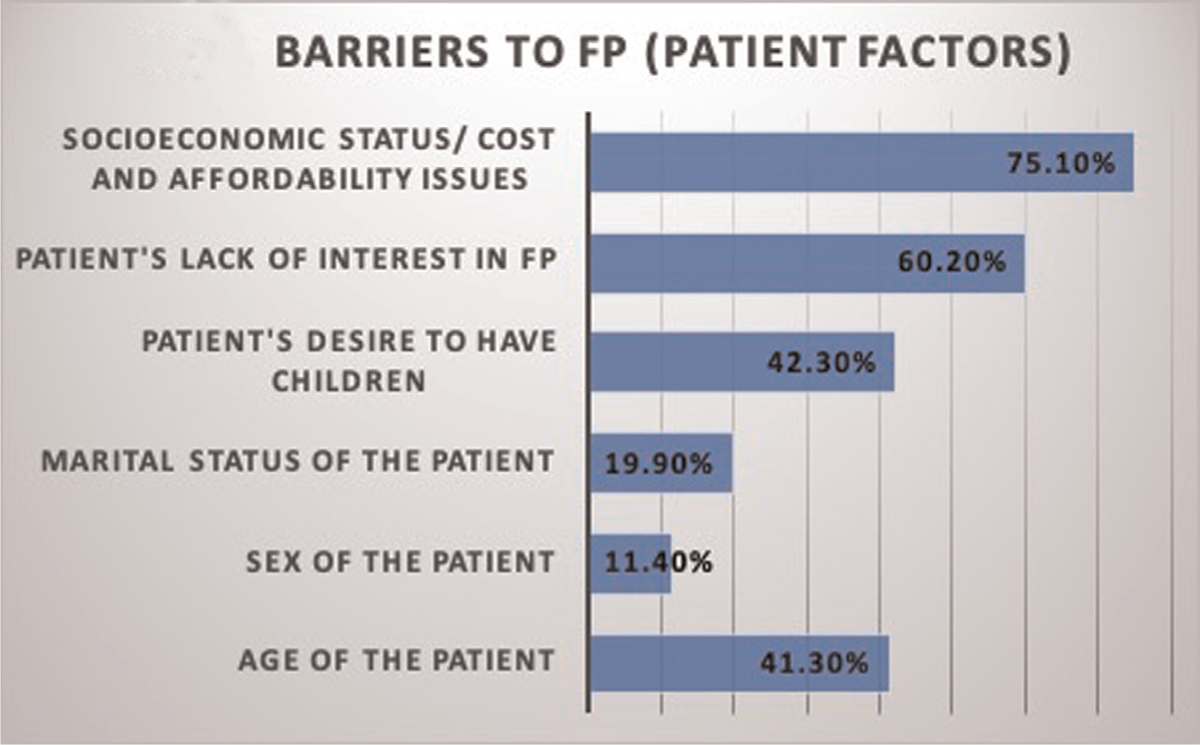
- Barriers to FP (patient factors). FP, fertility preservation.
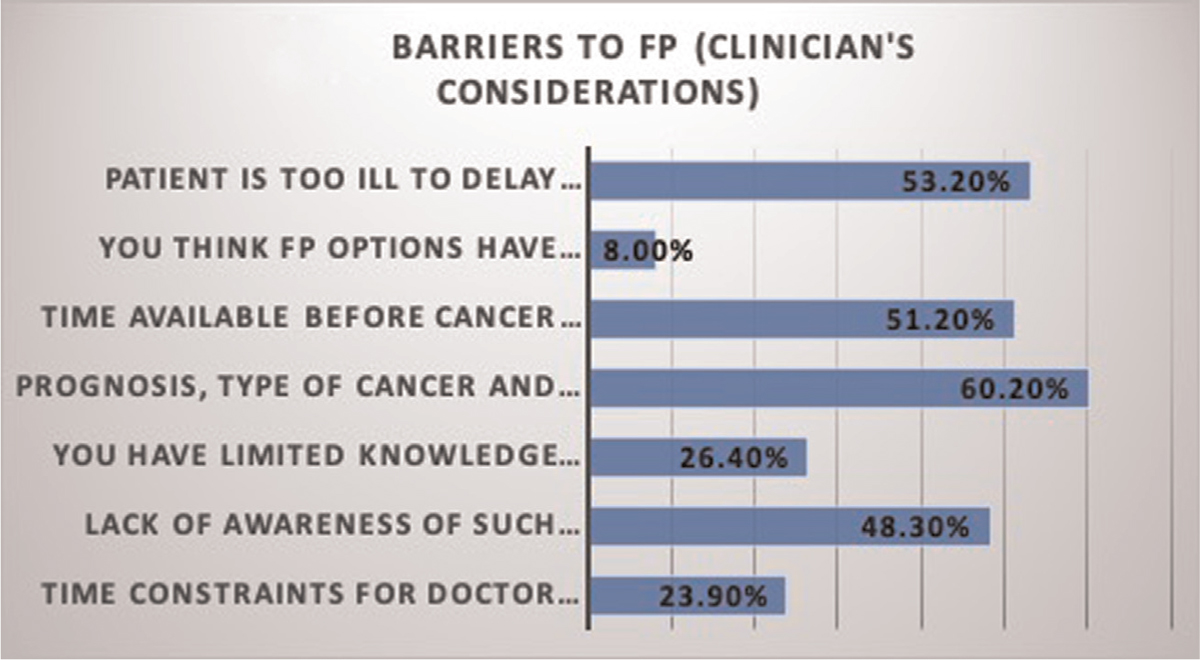
- Barriers to FP (clinicians’ considerations). FP, fertility preservation.
DISCUSSION
This report represents the first quantitative survey in India, to our knowledge, of clinicians from various specialties (gynecology, infertility, oncology, radiotherapy, and general surgery) involved in the care of cancer patients from multiple institutions.
Knowledge and Awareness Regarding Fertility Preservation
The results in our study indicated that the knowledge of participants regarding the impact of radiotherapy and chemotherapy on fertility was very high that was similar to the survey conducted in China, which reported that nearly 95% of physicians acknowledged that cancer treatment can affect patient’s fertility.[3] However, another study[4] reported that nearly 50% and 70% of the physicians acknowledge the damage caused by radiotherapy and chemotherapy, respectively, which indicated that the knowledge score of Chinese oncologists that participated in this survey was lower as compared to participants in our study.
Our findings suggest that 76.6% had a high level of knowledge regarding FP in male cancer patients and 86.6% for FP in female cancer patients. This was in contrast to a study that implied that nearly 40% of the oncologists were familiar with FP.[4] Another study reported that less than 50% of the respondents were knowledgeable about fertility preservation.[5]
A study indicated that 62% of oncologists were aware of male fertility preservation, and 40.1% of them were aware of female fertility preservation methods.[3]
The high level of knowledge regarding the impact of cancer treatment on fertility and awareness regarding fertility preservation in males and females in our study can be attributed to the fact that the majority of the respondents were from medical colleges, government hospital, urban area, and tertiary level corporate hospitals offering advanced care to the patients. Also, it is possible that clinicians who have a special interest in fertility preservation or those with good knowledge are more likely to respond to the survey. Remarkably, the level of knowledge among specialists that are the first or primary contact to cancer patients such as general surgeons and gynecologists is less as compared to oncologists and infertility specialists highlighting the need to prime and increase the level of awareness and knowledge regarding FP among these first-contact clinicians so that no cancer patient that is eligible is devoid of information regarding FP and there is no delay in referral services for same.
Again the awareness regarding various fertility preservation methods was moderate to high in our study, contrary to a study that indicated a low level of knowledge for various FP methods; 22.5% for IVF (In vitro fertilisation), 24.4% for oocyte cryopreservation, and 18.2% for ovarian tissue cryopreservation.[6]
Awareness Regarding ASCO Guidelines
Our study indicates that awareness regarding ASCO guidelines on FP was moderate, in contrast to another study that reported that nearly 60% of oncologists were aware of ASCO guidelines for fertility preservation.[7] Another survey that was done on awareness regarding ASCO guidelines on FP indicated that only 38% of the oncologists that participated in the survey were aware of ASCO guidelines.[8]
This discrepancy in awareness can be explained in part by the time period of the survey done. Our study was conducted in 2019, whereas the abovementioned studies were done in 2009 and we believe that over these years awareness regarding FP has increased.
Practice Behavior
It was heartening to note that majority of the respondents explain to the patients that cancer treatment is gonadotoxic and the adverse effect it can have on fertility similar to a study that showed that nearly 77% of the participants discuss with patients their fertility issues that may arise out of cancer treatment and felt that it was their responsibility to discuss fertility issues.[6] Similarly, another study indicated that nearly 80% of the physicians usually or always inform the possibility of infertility with the gonadotoxic cancer treatment.[9] In contrast, the findings of a French study show that less than half (47%) of the respondents discuss risks of infertility resulting from cancer treatment with their patients.[10]
The knowledge translated to a discussion in nearly 65% of the respondents. The finding was in contrast to this study where the survey reported that the majority of the participants believe that FP should be recommended to the patients but only 35% actually initiate discussion on FP.[3] Similarly, the French study shows that approximately one third (35%) of their respondents reported discussing the possibility of FP before beginning cancer treatment and 26% seldom discussed if at all.[10] Another study showed that nearly 60% of the oncologists discuss FP with their patients.[6] However, another study suggested that nearly 3-4th of the physicians often inform the patients about the FP option before the commencement of treatment.[9]
The index study showed that nearly 60% of our participants, seldom or rarely provide patients with written information on FP and only 18.9% always provide written information. Similar results were obtained from this study that showed that only 13.5% provide the patient with educational material regarding cancer and FP from various sources available in the United States.[11] There is not much discrepancy in the results with our study but there still could be biased results as the study by Quinn et al.[11] included more than 500 oncologists and our study had 201 participants from various specialties that included 16 oncologists. In contrast to our findings, one study from the United States reported that 51% of physicians always use education materials while discussing FP. Also, these educational materials were used by 54% of advanced practice nurses and 39% of nurses.[12] In a survey of Iranian oncologists, only 11% of male oncologists and 16.3% of female oncologists reported that they provided their patients with written information about FP that was much low as compared to our study.[13]
This indicates that FP counseling is done not only by physicians but also by advanced practice nurses and nurses in this country that is a rarity in our country where the onus of discussing FP with the patients lies only on the physicians. If we could include counselors and nurses to actively participate in creating awareness and promoting FP in cancer patients in our institutes or hospitals, our FP practice would improve and would be beneficial to the vast majority of cancer patients and having said that, time constraints in the doctor’s clinic would never be a barrier for FP.
Nearly three-fourths of respondents in our study considered fertility as an important quality of life issue. This study indicated that 59% of the physicians considered fertility as an important quality of life issue and 93% considered quality of life in general after gonadotoxic treatment to be important.[14]
The respondents in our study reported that 53.7% would always plan cancer treatment regimens taking into consideration the patient’s desire for future fertility and 26.9% would usually do that. Attending an educational session on FP appears to influence the clinician’s considerations of the patient’s desire for fertility while planning the cancer treatment (45% vs 33%). Approximately 55% of attendees willingly considered a less aggressive treatment regimen compared to those who did not attend (29%).[15] Contrarily, another study showed that instead of choosing a lower infertility-damage regimen, 68.9% of physicians altered the treatment with a higher survival rate.[4]
Our study shows that the practice of consulting a specialist from another field regarding fertility issues of the patient and referring the patients for FP was moderate to high. The study among Iranian oncologists showed that the majority, 73.3% male oncologists, and 71.4% female oncologists, referred cancer patients to reproductive specialists.[13] Similarly, another study remarkably reported 72% of the physicians had referred patients to an oncofertility consultation in 2015 compared with 46% in 2012, showing a dramatic increasing trend.[9]
On the contrary, the survey of oncologists at Duke University suggested that nearly 45% never referred patients for FP, whereas our study reported that only 6.5% never or rarely referred patients for FP.[15]
One study showed that 47% of respondents routinely refer cancer patients of childbearing age to a reproductive endocrinologist and referrals were more likely among female physicians.[7]
Our results for referral practices showed variations with respect to the specialty and marital status of the respondents. On the contrary, one study showed that General surgeons made the largest contribution to FP referrals for breast cancer patients (36.5%), followed by medical oncologists (27.0%) and family physicians (20.8%). No differences in referral rates were observed according to physician’s sex and age.[16] Another study showed that female and younger oncologists (age less than 50 years) had a significantly higher probability of referring patients to reproductive specialists.[17] One study reported that 34.6% of providers consulted with specialists regarding fertility issues.[18] In a Chinese study, only 31.1% of physicians ever consulted a fertility specialist about fertility issues or referred patients to specialists.[4] Another study reported that nearly two-thirds of the respondents had never referred a patient for FP and among the one-third of those who had, the majority had referred less than five patients in a year.[5]
Physician’s Attitude Toward Fertility Preservation
Current study indicates that the majority (81.6%) of physicians agree or strongly agree that more information regarding FP is required and there was widespread agreement on the fact that setting up an FP center is necessary. Similarly, a study in China indicated that oncology physicians had an optimistic attitude toward FP but knowledge regarding the same was insufficient and they would appreciate and welcome training programs.[4] Similar was the opinion of Turkish hematologists in a survey that reported and opined on publishing a guidebook on FP and holding regular sessions in the congress to create awareness and acquire more knowledge that would be helpful in their clinical practice.[19] Various other studies also concluded that lack of efficacy and knowledge among clinicians is a deterrent for offering FP to their patients and the majority of clinicians, Health care providers, advanced practice nurses would benefit from educational information about fertility preservation options and methods.[12,20]There was widespread agreement among participants in our study that discussing FP with a newly diagnosed cancer patient is a high priority for them. Similarly, the clinicians in this study reported a high sense of responsibility toward patients for discussing fertility issues and FP.[6] However, according to another survey, many oncologists acknowledged the importance of fertility but attributed the responsibility for FP to others.[21]
The majority of Chinese clinicians in Hong Kong (94%), in a survey, agreed to set up a dedicated referral center with government funding and 73.4% believed that FP should be available as a government-funded service for medical indications.[22] Similarly, in another study, up to 76.5% (117/153) of the respondents agree that fertility preservation should be available as a public service.[5]
Barriers of Fertility Preservation
The results of the study showed that poor prognosis (66.9%) was cited as a major barrier among clinicians in one center in China that is very similar to our study.[4] Another study reported the factors that acted as a deterrent to initiating FP discussion or referral was the poor prognosis, cited by 54% of the respondents while approximately half of the respondents reported cancer requiring urgent treatment as the reason. About 51% of the respondents mentioned the age of the patient more than 40 years and 45% reported that the patient did not ask for information on fertility as the reason why they might not initiate discussion on FP.10] Limited knowledge of physicians about FP was cited by 43.6% which is a high number as compared to our study (26.4%).[4] The economic status was cited by 15.4% while our study showed cost and affordability/ socioeconomic status to be the major hindrance (75.1%).[4] This role of financial constraints is very understandable considering the self-funding of all oncological treatments.
In a Hong Kong study, the hindrances faced by clinicians in discussing FP was analyzed which are as follows in decreasing order of occurrence /importance: non-availability of time before initiating treatment (60.6%), poor prognosis, or high risk for cancer recurrence(53%), economical constraints (47%), cancer treatment is the top priority (38%), and being unaware of centers where referral can be made (35%). Similar results are reported in other studies also.[5,23]
Patient’s lack of interest in FP (39% versus 60.2%) and time constraints because of the urgent need to start therapy (13% versus 53.2%) were other commonly reported reasons.[15]
The reasons for declining FP in this latest study were the following: prioritizing cancer treatment (56.6%), having children (40.3%), age (20.8%), financial burden (10.1%), and being afraid of the possible influence of genetic factors on future progeny (6.1%).[24]
It is surprising to note that nearly 50% (48.3%) of the clinicians in our study, which is a significant number, are not aware of such centers where referral for FP can be made. Hence, referral pathways should be made clear. The process and protocol for referral should be identified. The clinicians and hospitals should be provided with a list of centers where facilities for fertility preservation are delivered. Making such arrangements will make the referral pathways easy.
Limitations and Strengths
The majority of the clinicians that participated in our study were from medical colleges, government hospitals, and tertiary level corporate hospitals that offered advanced care to patients. The results obtained may not reflect the views of clinicians from different practice set up (for example, rural and remote areas where medical facilities are not advanced or in a resource-poor setting) and regions of the country. It is possible that clinicians who have a keen interest in FP or have a good level of knowledge have been more likely to respond to the survey. The knowledge, attitude, and practice behavior that the clinician cites are self-reported and hence in part may be biased as there are many factors that cannot be measured. The sample size is too small to reflect the survey results that can be extrapolated to a diverse country like India. The strength of our study is inclusion of clinicians that are involved in the treatment of cancer patients from various specialties and institutions. One aim was to identify potential barriers but it has also thrown light on how these potential barriers to FP can be overcome.
CONCLUSIONS
The concept of fertility preservation is relatively novel but rapidly emerging and awareness regarding the same has increased over the years. The knowledge and attitude among surveyed clinicians were very positive. However, there was a significant lack of knowledge among first-contact physicians. The attitude of physicians varies according to age, gender, their own fertility status, experience, and specialty. The major barriers identified were the cost, poor prognosis, lack of referral system, and time constraints. To improvise the utilization of fertility preservation services, the deficit in clinician’s knowledge should be circumvented by providing them with basic, advanced, and up-to-date information. This can be achieved by (i) introducing formal training in the study curriculum of specialty, super-specialty courses, and fellowships programs; (ii) providing more information on the subject by holding CMEs, seminars, separate sessions in various national, and international conferences. To ensure that majority of cancer patients receive fertility preservation counseling and services, it is imperative that allied health care providers, nurses, and social workers be trained so that time constraints in the doctor’s clinic are not a deterrent in offering FP. To make patients understand the FP process and also for making it easy for health care professionals, written material in the form of printed handouts, information booklets, website, and online portals for the same should be established. The referral pathways should be defined and a list of such centers should be made available so that not knowing of a center where referrals can be made should not come in the path of doctor’s willingness to refer. The sensitization of health care professionals and spreading awareness regarding fertility preservation is most solicited. Strengthening fertility preservation counseling and referral patterns, better collaboration between the clinicians from different specialty to offer a multidisciplinary approach to cancer treatment is need of the hour.
Ethical approval
Ethical approval was taken from Independent Ethical committee of Indian Fertility Society [F.1/IEC/IFS/2020No.44]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Sexual health problems in French cancer survivors 2 years after diagnosis-the national VICAN survey. J Cancer Surviv. 2016;10:600-9.
- [Google Scholar]
- Knowledge, attitudes, and intentions toward fertility preservation awareness among oncologists in China. J Clin Oncol. 2018;36:e18537.
- [Google Scholar]
- The knowledge attitude and self-reproductive behaviours of oncology physicians regarding fertility preservation in adult cancer patients. J Cancer Educ. 2019;35:1119-27.
- [Google Scholar]
- Evaluation of the awareness of, attitude to, and knowledge about fertility preservation in cancer patients among clinical practitioners in Hong Kong. Hong Kong Med J. 2017;23:556-61.
- [Google Scholar]
- Oncologists’ confidence in knowledge of fertility issues for young women with cancer. J Cancer Educ. 2012;27:369-76.
- [Google Scholar]
- Physician referral for fertility preservation in oncology patients: a national study of practice behaviors. J Clin Oncol. 2009;27:5952-7.
- [Google Scholar]
- Survey: little awareness of ASCO fertility-preservation guidelines by cancer specialists. Oncol Times. 2009;31:26-30.
- [Google Scholar]
- Can we improve referrals for fertility preservation? Evolution of practices after the creation of a fertility network. Future Oncol. 2016;12:2175-7.
- [Google Scholar]
- Fertility preservation in women with cancer: a national study about French oncologists awareness, experience, and feelings. J Assist Reprod Genet. 2018;35:1843-50.
- [Google Scholar]
- Oncologists’ use of patient educational materials about cancer and fertility preservation. Psychooncology. 2012;21:1244-1249.
- [Google Scholar]
- Pediatric oncology providers’ attitudes and practice patterns regarding fertility preservation in adolescent male cancer patients. J Pediatr Hematol Oncol. 2016;38:118-22.
- [Google Scholar]
- Little information about fertility preservation is provided for cancer patients: a survey of oncologists’ knowledge, attitude and current practice. Eur J Cancer Care. 2019;28:12947.
- [Google Scholar]
- Oncologists’ practice and attitudes regarding fertility preservation in female cancer patients: a pilot study in the Netherlands. J Psychosom Obstet Gynaecol. 2013;34:129-32.
- [Google Scholar]
- Pilot survey of oncologists regarding treatment-related infertility and fertility preservation in female cancer patients. J Reprod Med. 2009;54:203-7.
- [Google Scholar]
- Patterns of referral for fertility preservation among female adolescents and young adults with breast cancer: a population-based study. J Adolesc Young Adult Oncol. 2019;8:197-204.
- [Google Scholar]
- Physicians’ knowledge, attitude, and behavior regarding fertility issues for young breast cancer patients: a national survey for breast care specialists. Breast Cancer. 2013;20:230-40.
- [Google Scholar]
- Attitudes and practices of pediatric oncology providers regarding fertility issues. Pediatr Blood Cancer. 2007;48:80-85.
- [Google Scholar]
- Knowledge, attitudes, and practices of hematologists regarding fertility preservation in Turkey. Turk J Haematol. 2013;30:269-74.
- [Google Scholar]
- Talking about fertility in the context of cancer: health care professional perspectives. Eur J Cancer Care. 2016;25:99-111.
- [Google Scholar]
- Clinicians’ perspectives on barriers to discussing infertility and fertility preservation with young women with cancer. JAMA Netw Open. 2019;2:e1914511.
- [Google Scholar]
- Fertility preservation in Hong Kong Chinese society: awareness, knowledge, and acceptance. BMC Womens Health. 2020;20:86.
- [Google Scholar]
- Utilization and knowledge of oncofertility preservation services: a single institution experience. Fertil Steril. 2019;111:39-40.
- [Google Scholar]
- Level of knowledge and needs on fertility preservation in reproductive-aged male patients with cancer. J Cancer Educ. 2020;35:321-26.
- [Google Scholar]







