Translate this page into:
A novel fertility score predictor: a cafeteria approach for fertility treatment option
Address for correspondence: Dr. Snehal Chavan, M.B.B.S, D.G.O, Fellow in reproductive medicine at Ssmile IVF centre, Shree Hospital, Opposite Agakhan Palace, Nagar Road, Pune, Maharashtra, India. E-mail: bdhorepatil@gmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Fertility prediction application is the need to increase the likelihood for early approach at right time in infertility. In this study, we propose to investigate the use of a fertility score predictor (FSP), score system with colour code for easy understanding and calculated by using common easily available variables associated with fertility. We applied this score system retrospectively to our own out patients and analysed our infertility management protocols to those patients with outcome.
Materials and Methods:
A total of 100 patients who attended for the infertility treatment at Ssmile Fertility Center in Pune during the period of October 2018 to February 2020 were retrospectively evaluated. The demographic variables were categorised according to their impact on fertility reported by previous studies and each category was assigned to a value to calculate the Fertility score predictor (FSP) with colour code (green, blue, orange, and red green, blue, orange, red, black) for easy understanding and applicability.
Results:
The association between infertility and colour codes based on FSP was evaluated and the results showed that all analysed variables were significantly associated to the colour code, revealing that a higher number of patients with high FSP presented a healthy lifestyle, regular menstruation, and regular sexual intercourse. Also, it was observed that all patients with high FSP had been diagnosed with unexplained infertility, and the number of patients with other causes of infertility increased as score was lower.
Conclusions:
The association between FSP and fertility related parameter suggests that the score is suitable for detecting the patients with lower fertility at early stage. The treatment option based on FSP was associated with early detection and appropriate intervention.
Keywords
Age
body mass index
fertility predictor score
marriage duration
prediction
sexual intercourse
unexplained infertility
INTRODUCTION
Over the recent years, infertility has become one of the more frequent health issues that couples are facing. Sedentary lifestyle with minimal physical activity, addictions, stress level, and different food habits and irregular sleeping patterns, are few of the reasons that cause infertility.[1] Many studies have shown that parenting is an important part of life for most couple, and that infertility is the most common health issue amongst them.[2] Involuntary childlessness brings psychological and psychosomatic disorders, mainly in women, becoming a real social stigma. Not only they present depression, distress, or high anxiety levels, among others, but also they have less social support.[3,4] In fact, previous studies indicated that childless people present difficulty in keeping social bonds with people who have children and are sometimes excluded from social gatherings.[5] It has been described that infertility and subfertility affect around 15% of couples, but this number would be underestimated and it has showed no improvement in the last decades.[5] The challenges associated to this high burden have been solved at some extent by reproductive medicine and endocrinology using many different methods from fertility awareness methods to more complex techniques.[6] According to the World Health Organization (WHO), global infertility prevalence rates are difficult to estimate.[5] The global prevalence of infertility has remained high as shown by a WHO study that revealed infertility burden levels and tendencies were similar to those calculated 12 years before. This suggested that, although many novel and effective therapies have been developed, solutions in the treatment seems to be “the tip of the iceberg”.[6]
Infertility has been defined as the failure to accomplish a clinical pregnancy after 1 year of regular sexual intercourse without protection. However, in couples were the female with advanced maternal age, over 35 years; the couple assessment begins after 6 months of seeking conception.[7] Strong evidence indicates that many female and male factors can explain infertility such as failure to ovulate, menstrual cycle problems, reproductive system structural problems, infections, egg maturation defects, implantation failure, endometriosis, polycystic ovary syndrome, primary ovary insufficiency, autoimmune disorders, and uterine fibroids.[8] Failure to ovulate is the lead cause of female infertility and aging leading to reduced ovarian reserve and lifestyle and environmental factors have been related to ovulation disorders, oligoospermia and azoospermia.[8,9]
The Practice Committee of the American Society for Reproductive Medicine (ASRM) established standard guidelines to evaluate infertility(9). Couples tests include semen analysis, ovulation evaluation, hysterosalpingogram, and ovarian reserve test. If all tests result normal, the couple is diagnosed with unexplained infertility.[7] Approximately 15–30% of couples are diagnosed with unexplained infertility.[10] One of the issues addressed to treat a couple with unexplained infertility includes counseling and methodical lifestyle changes. Previous studies have shown that women’s smoking, high or low body mass index (BMI), and excessive caffeine or alcohol intake can affect their fertility and physicians advise their patients to optimize BMI, and strict restriction on caffeine and alcohol intake.[11] In these cases, the optimal treatment for patients relies on woman’s age and duration of infertility.
With improved literacy in India and busy lifestyle, fertility awareness methods is the new norm to increase the probability of natural conceiving, and predicting the fertile and infertile days of a woman’s menstrual cycle and take the appropriate steps towards achieving their goal of fertility.[12] It has been suggested that primary care physicians should perform reproductive health promotion to women of advanced age, educating women about their fertility potential.[12] Considering the relevance of age, duration of marriage, lifestyle, and environmental factors on fertility, and the availability of the assisted reproduction treatment (ART), we believe that scoring the contribution of these factors into the couple’s fertility might improve the outcome of fertility treatments and help physicians to make the right choice for the couple’s next step in line. However, there is no simple and user-friendly application like fertility scores systems designed to evaluate fertility potential and treatment road map. In this study, we propose to investigate the use of a fertility score calculated by using the common variables associated with infertility such as age, BMI, lifestyle, marriage, and sexual history and any obvious diagnosis.
Taking into consideration this background, we intend to develop a specific fertility score predictor (FSP) application for knowing the fertility potential with broader social contexts. It is a simple and efficient method to calculate the couple’s score and determine the category of the treatment the couple falls into. Its purpose is to educate the couple, families, practitioners, and family physicians to have a simplified yet effective way for a treatment road map while avoiding delay for the anxious couple. On the other hand, FSP is useful for those couples who can achieve pregnancy without fear of getting into the vicious path of the treatment cycles who scores higher.
The variety of infertility treatments has direct consequences on standard of care among practitioners. The use of FSP could help with the decision-making process for the couple in their infertility treatment. As well, this simple and user-friendly application “FPS” will enable the couple to know their fertility potential, decide the treatment option and the severity of the situation. Thus FPS can (a) provide Road map and awareness about infertility treatment for common people and (b) to improve the decision-making processes among practitioners and gynaecologist.[13,14]
MATERIALS AND METHODS
Patient population and scoring
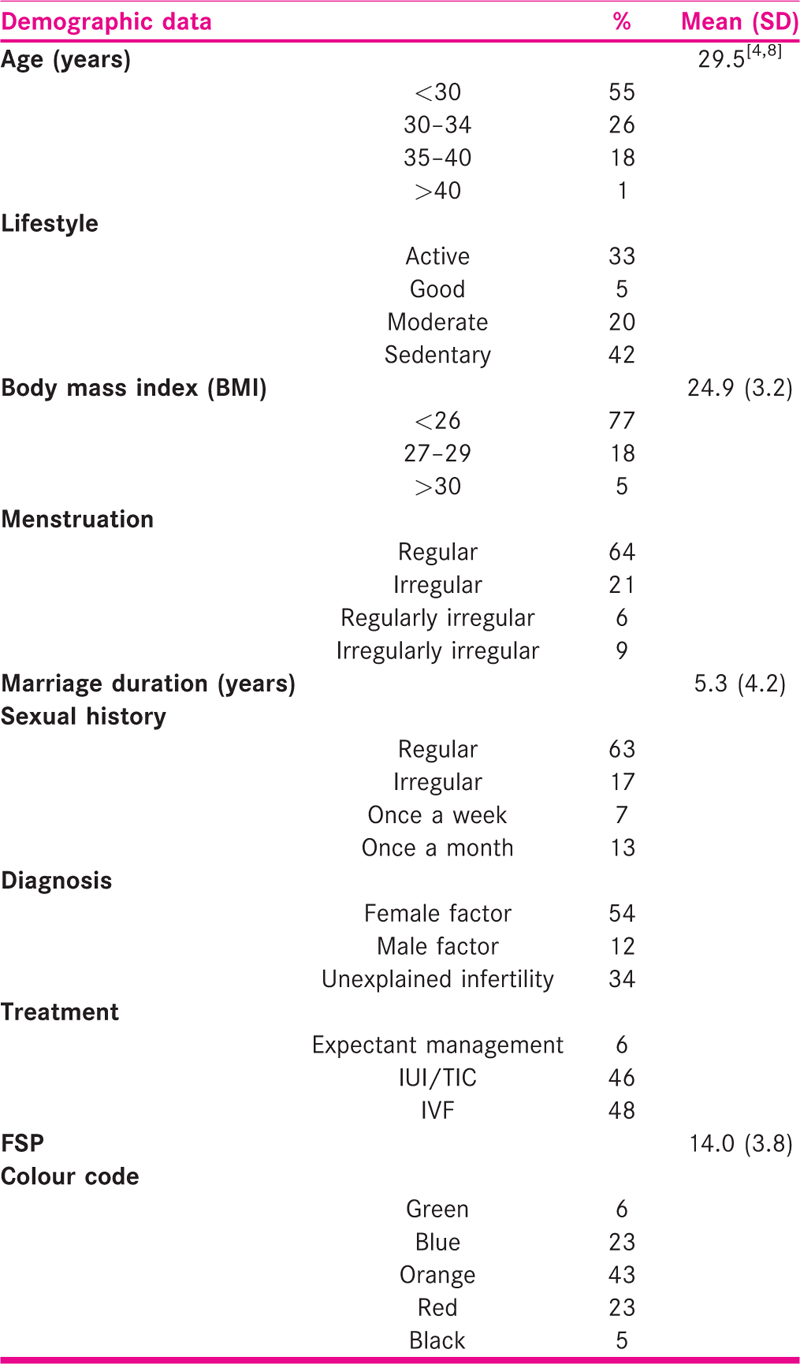
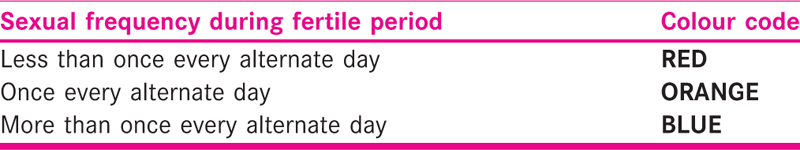
A total of 100 patients who attended Ssmile Fertility Center in Pune and were treated because of fertility issues during October 2018 to February 2020 were retrospectively evaluated. Data was recovered from the clinical charts and age, BMI, marriage duration time, lifestyle (physical activity intensity), infertility cause, sexual intercourse regularity, and menstruation regularity were registered to calculate FPS. Also, the applied fertility treatment was recorded. The demographic variables were categorized according to their impact on fertility and each category was assigned to a value to calculate the FSP with colour codes (Green, Blue, Orange, Red, and Black) to carry understanding and applicability [Table 1]. The analysed variables were chosen in order to allow any couple to apply on its own. FSP was calculated by adding the score resulting from the corresponding category of each variable.

The inclusion criteria were: patients > 21 years, BMI of 16 onwards, marriage duration > 1 year. Patients < 21years and married during <1 year were excluded from this study.
Fertility Score Predictor
Fertility score was classified according to number and colour coding as follows:
Green (>20 score): Expectant management including diet modifications, alleviation of stress with natural try for conception for 6 months to 1 year duration. Lifestyle changes recommended (such as weight loss, quit smoking, reduction of caffeinated drinks) were suggested at least for 6 months. Blue (15–19 score): Active involvement of treatment option including consultation to fertility specialist to perform all basic investigations, timed intercourse (TIC), detection of ovulation by urinary kit, or basal body temperature (BBT), or sonographic assessment. Basic investigations including all routine investigations, female hormonal investigations, male semen analysis.
Orange (10–14 score): Consistent & Active management including ovulation induction with ovulogens and/or gonadotropins along with intrauterine insemination (IUI) for 3–6 cycles and Endoscopy procedure.
Red (5–9 score): Aggressive management including IVF, ICSI, intracytoplasmic morphologically selected sperm injection (IMSI), testicular sperm extraction (TESE), percutaneous epididymal sperm aspiration (PESA), micro-TESE, assisted laser hatching, blastocyst embryo transfer, time-lapse monitoring for 3 to 6 cycles.
Black (<5 score): Alternative option including using gamete donor, surrogate, embryo donor, uterine transplant.
Our previous results indicate that FSP colour code classification was able to predict the applied fertility treatment with a predictive value of 94.2% (non-published data).
Primary and secondary outcomes
The primary outcome measure was the association between the FSP colour code suggested treatment and the applied treatment and pregnancy outcome. The secondary outcome was the mean value of the analyzed variables (age, marriage duration, BMI, lifestyle) compared between the different FSP colour code categories.
Statistical analysis
Data were analyzed using GraphPad Prism version 7.00 software. Descriptive statistics are presented as percent, mean, and standard deviation. Chi-square test and ANOVA comparisons were used in data analysis and a p<0.05 was considered statistically significant.
RESULTS
In this study, we have evaluated 100 patients after the couple was diagnosed with infertility according to WHO definition and treated in Ssmile fertility center, Pune fertility during October 2018 to February 2020. The patient’s demographic data are shown in Table 2.
The association between factors that could affect fertility and colour codes based on FSP [Tables 3 and 4] was evaluated and the results showed that all variables analysed were significantly associated to the colour code, revealing that a higher number of patients with green code presented a healthy lifestyle, regular menstruation, and regular sexual intercourse [Table 5]. Also, it was observed that all green code patients had been diagnosed with unexplained infertility, and the number of patients with other causes of infertility increased as score was lower [Table 5].
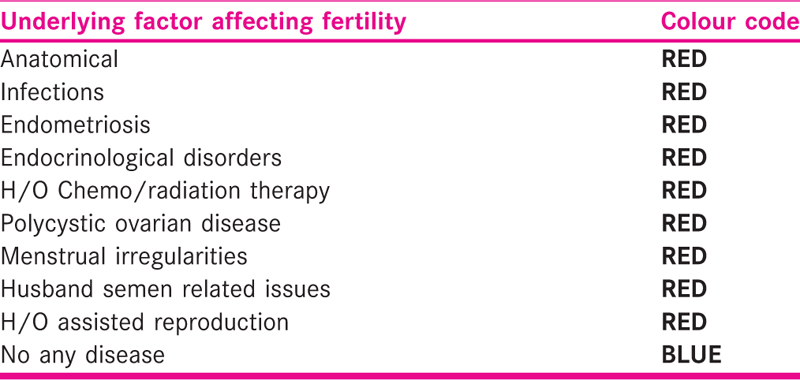
According to FSP, black and red colour patients are advised to receive IVF treatment, orange colour patients should receive IUI, blue colour patients should start Active involvement of treatment option, and green couples should receive expectant management.
A positive association was shown between the treatments applied and the colour code (P < 0.0001). All the patients from the red and black colour groups were, in fact, treated with IVF. Most orange colour patients were treated with COH + IUI as would be suggested but 35% were treated with IVF. Half of the green colour patients were treated with expectant management as suggested, and the rest were indicated with TIC/IUI. It must be noticed that none of the patients form the green group underwent IVF [Table 4]. IVF use increased as FSP decreased revealing a statistical association (P < 0.001). Conversely, expectant management and TIC and IUI increased as FSP increased, indicating a significant association (P < 0.0001 and P < 0.001, respectively).
Regarding pregnancy outcomes, it was observed that half of the green patients became pregnant and that red and black colour groups presented the higher pregnancy rates (P = 0.05).
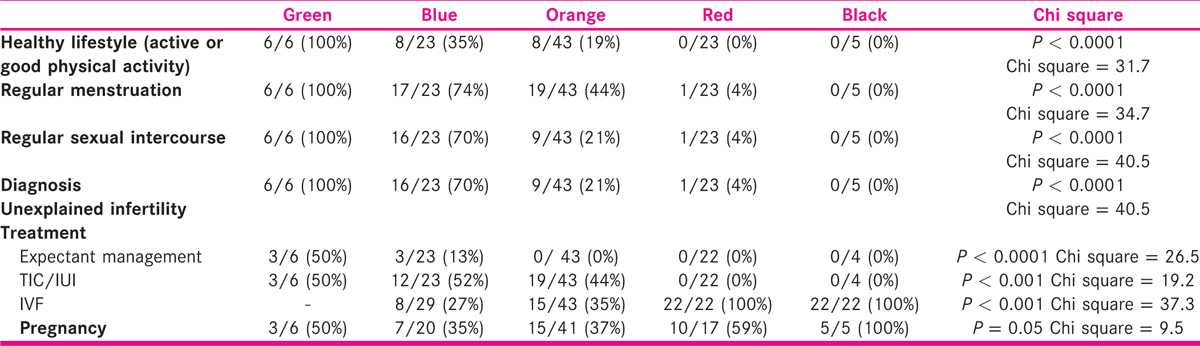
On the other hand, the results showed that the mean BMI comparison revealed no statistically significant difference among patients with different colour codes (P = 0.40, Figure 1a). However, the ANOVA comparisons between age and marriage duration indicated that the group of patients with orange, red, and black colour were increasingly older (P < 0.01, Figure 1b). Additionally, the black group of patients had been married for a significantly higher mean time than the other groups [Figure 1c].
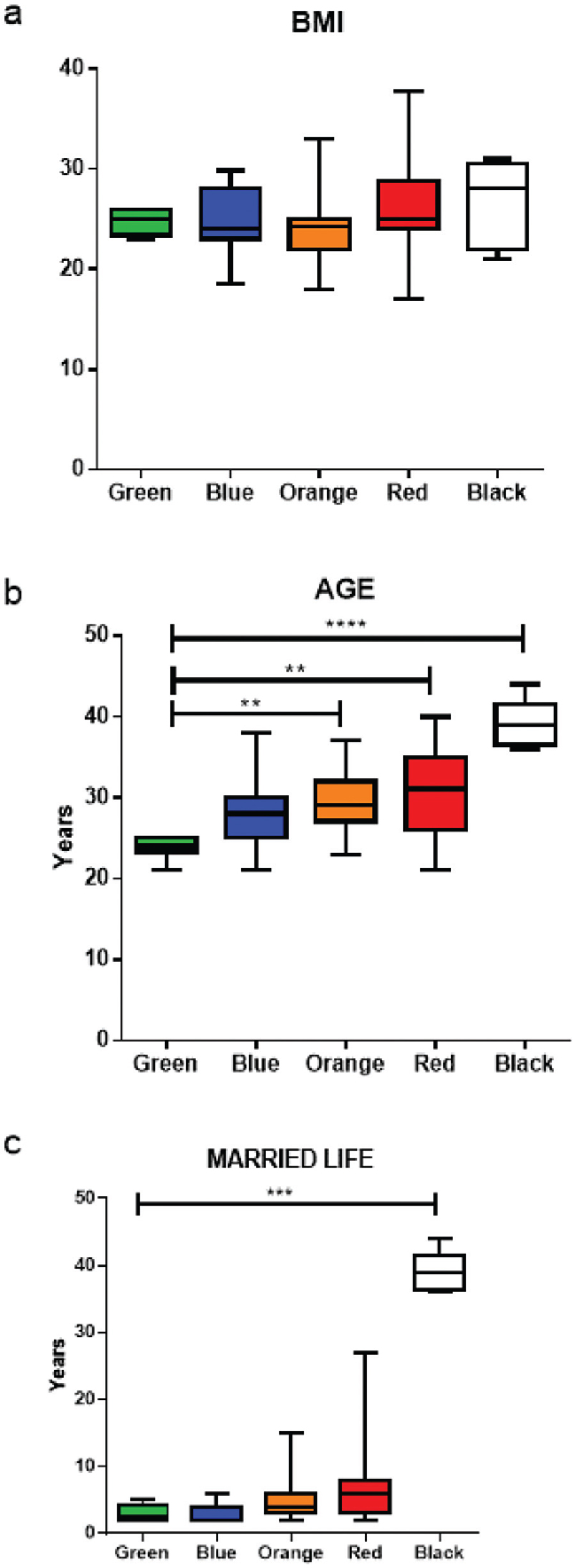
- ANOVA comparisons between the mean values of (a) BMI, (b) age and (c) marriage duration among different colour code groups. ****P < 0.0001, ***P < 0.001, **P < 0.01
DISCUSSION
In this study we have investigated the association between FSP, a score developed in our center and fertility related variables and proposed infertility treatment. The score was associated with the patient’s age, duration of marriage, menstrual cycle, sexual history, and any known obvious diagnosis related to infertility. The association between factors and colour codes based on FSP was evaluated and the results showed that all variables analysed were significantly associated to the colour code, revealing that patients with high FSP presented a healthy lifestyle, regular menstrual cycle pattern, and regular sexual intercourse. Also, it was observed that all patients with high FSP fall into unexplained infertility category and the lower score was seen in patients with known prior obvious factor of infertility. A significant association was found between the treatments proposed and the patients with lower score patients. The ANOVA comparisons between age and marriage duration indicated that the group of patients with lowest scores were older and had been married for a longer period of time than the other groups. The evidence points that the FSP could be suitable to predict the appropriate treatment that the couple should receive to achieve the best outcome, since there was a significant association between the score (colour group) and the treatment given. Moreover, pregnancy rate was higher in green, red, and black groups, suggesting that the treatments given for these score (colour groups) were appropriate.
We propose that green code couples (FSP > 20) should be opted for an expectant management for 6 months. Expectant management includes Diet modifications, stress management with natural methods for conception for 6 months to 1 year duration. Lifestyle changes such as weight loss, quitting smoking, reduction on caffeinated drinks, adequate and regular sleep pattern.
Blue code couples (FSP = 15 to 19) were recommended to be evaluated with fertility expert consultation and Basic investigations with detection of Ovulation by non invasive methods with Timed intercourse aligned with Ovulation time and Orange code couples (FSP = 10–14) recommended first line treatment options like Ovulation Induction using ovulation inducing drugs with IUI for 3–6 cycles and if required fertility enhancing endoscopy procedures. In red code couples (FSP = 5 to 9) we recommend aggressive treatment options like IVF, ICSI, intracytoplasmic morphologically selected sperm injection (IMSI), testicular sperm extraction (TESE), percutaneous epididymal sperm aspiration (PESA), micro-TESE, assisted laser hatching, blastocyst embryo transfer, time-lapse monitoring for 3 to 6 cycles.
Black code couples (FSP < 5) were recommended to receive alternative therapies like gamete donor or surrogacy.
The association between advanced age and decline in fertility has been well documented. It has been observed that women prioritise their job careers and personal issues to their fertility and that leads to, eventually, to seek advanced treatment options[14]. From thousands of primordial follicles that women has since birth, only few hundreds remain at the age of menopause, as monthly fecundity rate falls from 25% at age 20–30 years to <10% in women over 35 years.[15,16] The number of oocytes, however, is not the only cause of reduced fertility among older women. As women ages, her fertility potential drastically deteriorates.[17] Accordingly, our results showed that the patients classified as orange, red, and black colour groups, exhibited an increasingly higher mean age than the other groups and required aggressive management or even alternative options. The younger patients with Green and blue code who showed less duration of marriage, an active lifestyle and regular menstrual pattern with regular coital history, presented a higher FSP and good pregnancy outcome.
There was no statistically significant difference between the mean BMI of the colour groups and pregnancy outcome. It has been reported that an altered BMI would relate to Anovulation, irregular menstruation, and hormonal disorders, among others.[18] Our observations indicated that most of the patients that presented BMI>29.9 showed irregular menses, were mostly in the black or in the red group, and received IVF treatment. It should be noticed that almost half the patients presented BMI<25, related to a normal weight, while only 5% of the patients presented obesity, which could explain why we could not observe a statistically significant difference.
Our observations showed a significant association between healthy lifestyle (physically active) and the colour code groups. Green and blue groups showed the highest percentages of women with non-sedentary habits, and this number decreased along with the score groups. These results are in agreement with previous publications that states that physical inactivity has been associated to a decrease in fertility. A study by Foucaut et al.[19] revealed that sedentary behaviour was significantly associated with infertility in women. These observations highlight the fact that lifestyle factors should be emphasized during the counselling and treatment
In addition, there was a significant association between regular sexual relations and colour code. The results showed that most women from green and blue group presented regular sexual intercourse, while the percentage decreased as the score decreased between groups. Black and red colour groups presented the lower percentage of women with history of frequent coitus. Lifestyle habits like diet, physical activity, and sexual intercourse frequency can be interrelated. A clinical trial showed that the intervention during 6 months in women’s lifestyle (diet and physical activity behaviour) was able to improve sexual function at least for 5 years, supporting again the importance of addressing these issues before resourcing the further treatment options.[20]
Interestingly, all green code patients fall into unexplained infertility category because of their basic investigations showed no abnormality and the duration of married life was more than one year according to WHO definition, and the number of patients with other causes of infertility increased as score was lower. The treatment of unexplained infertility is empiric and it usually includes expectant management with TIC and lifestyle modifications, controlled ovarian stimulation with IUI, and IVF according to the female patient’s age and duration of infertility.[7] Couples with unexplained infertility present a lower chance of pregnancy than normal couples due to low fecundity.[7] Expectant management is the lowest cost ART, but also brings the lower cycle fecundity rate that leads to a tendency to use other therapeutic resources. It has been recommended that expectant management would be appropriate in unexplained infertility where the female partner is young and duration of married life is less than 3 years.[7] These factors might explain why practitioners tend to choose more complex treatments or very basic treatment or declare patient as normal. In addition, expecting couples tend to be vulnerable to frustration, anxiety, and emotional stress. In this regard, 50% of the green colour patients were treated with expectant management and the rest were indicated with TIC and IUI and IVF treatment. Nevertheless, it should be considered that in this study no green group patients underwent IVF treatment. Additionally, the mean age of the green group was the lowest of all patients, suggesting that there was consistency between the practioner’s decisions, the patient status, and our FSP. A positive association was shown between the treatments given and the colour code and most of the patients from the red colour group were, in fact, treated with IVF.
In the last years, some prediction models have risen to help predict infertility treatment success. A systematic review showed that the most common predictors were age, duration of infertility, and ovarian/tubal causes and that prediction models can be applied to estimate the success of an infertility treatment.[21] However, it has been highlighted that a good statistical analysis with a good predictor validation are necessary to assure the predictor’s quality. Some studies have proposed to use biochemical markers such as anti-Müllerian hormone as predictors, while other studies used multivariate analysis to develop a prediction model using variables such as age, duration of subfertility, previous pregnancy, among others.[22,23] While the existing models are mainly thought to be used by healthcare professionals, our FSP, an easy-to-calculate score designed for couples to calculate on their own, would provide a valuable tool for couples seeking parenthood to know if they need to resource a fertility specialist. Our results suggest that FSP colour classification would be most useful to detect the patients with the lowest scores that should be enlisted for advanced and aggressive IVF treatment, contributing to an earlier treatment direction and satisfactory outcome.
CONCLUSION
The association between FSP-based colour codes and fertility treatment options suggests that the score is suitable for detecting the patients with good fertility potential or lower fertility potential at early stage, since good fertility potential would be related with a higher score while low fertility potential would be related with a lower fertility score. The treatment option based on FSP was associated with early detection and appropriate intervention. This explains why patients with high FSP score have been diagnosed with unexplained infertility because of timely basic investigation and consultation with fertility specialist. The evidence points that the FSP could be suitable to predict the appropriate treatment that the couple should receive to achieve the best outcome without losing their precious optimum fertile period. A limitation of this study is the small sample size and larger further prospective studies with a higher number of patients should be performed to validate the FSP score for its clinical use in the general population as user-friendly mobile App. As well it will give a road map for treating practioners to deliver standard of care without repeating the same steps in the management of infertility.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Infertility is rising in India’s populace [Internet] Deccan Herald 2019 Available from: https://www.deccanherald.com/opinion/panorama/infertility-is-rising-in-india-s-populace-788978.html
- [Google Scholar]
- The social and cultural consequences of being childless in poor-resource areas. Facts, views. Vis ObGyn. 2009;1:106-21.
- [Google Scholar]
- Psychological distress and infertility: forty years of research. J Psychosom Obstet Gynaecol. 1998;19:218-28.
- [Google Scholar]
- Infertility and psychological distress: a critical review of the literature. Soc Sci Med. 1997;45:1679-704.
- [Google Scholar]
- Infertility is a global public health issue. Available from: https://www.who.int/reproductivehealth/topics/infertility/perspective/en/
- Global prevalence of infertility, infecundity and childlessness.
- Diagnosis and treatment of unexplained infertility. Rev Obstet Gynecol. 2008;1:69-76.
- [Google Scholar]
- 2017. What are some possible causes of female infertility?. Available from: www.nichd.nih.gov/health/topics/infertility/conditioninfo/causes/causes-female
- Effectiveness and treatment for unexplained infertility. Fertil Steril. 2006;86:S111-4.
- [Google Scholar]
- The initial fertility consultation: recommendations concerning cigarette smoking, body mass index, and alcohol and caffeine consumption. Am J Obstet Gynecol. 2001;185:1168-73.
- [Google Scholar]
- Fertility awareness-based methods: another option for family planning. J Am Board Fam Med. 2009;22:147-57.
- [Google Scholar]
- Responding to infertility: lessons from a growing body of research and suggested guidelines for practice. Fam Relat. 2017;66(4):644-58.
- [Google Scholar]
- Effect of parental age on fertilization and pregnancy characteristics in couples treated by intracytoplasmic sperm injection. Hum Reprod. 1998;13:334-8.
- [Google Scholar]
- Accelerated disappearance of ovarian follicles in mid-life: implications for forecasting menopause. Hum Reprod. 1992;7:1342-6.
- [Google Scholar]
- Elevated risks of pregnancy complications and adverse outcomes with increasing maternal age. Hum Reprod. 2007;22:1264-72.
- [Google Scholar]
- Impact of Body Mass Index on female fertility and ART outcomes. Panminerva Med. 2019;61:58-67.
- [Google Scholar]
- Sedentary behavior, physical inactivity and body composition in relation to idiopathic infertility among men and women. PLoS One. 2019;14:e 0210770.
- [Google Scholar]
- A lifestyle intervention improves sexual function of women with obesity and infertility: A 5 year follow-up of a RCT. PLoS One. 2018;13:e0205934.
- [Google Scholar]
- Models Predicting success of infertility treatment: a systematic review. J Reprod Infertil. 2016;17:68-81.
- [Google Scholar]
- Anti-Müllerian hormone-based prediction model for a live birth in assisted reproduction. Reprod Biomed Online. 2011;22:341-9.
- [Google Scholar]
- Individualized decision-making in IVF: calculating the chances of pregnancy. Hum Reprod. 2013;28:2972-80.
- [Google Scholar]







