Translate this page into:
A simple non-invasive method of spermatozoa retrieval from the bladder (SPERB) in patients with retrograde ejaculation
Address for correspondence: S. Sowbarnika, Department of Andrology and Reproductive Medicine, Chettinad Super Speciality Hospital, Chettinad Academy of Research & Education, Kelambakkam, Rajiv Gandhi Salai, Chennai – 603103, India. E-mail: sowbee01@gmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Retrograde ejaculation is very commonly seen in men presenting with aspermia. Despite having normal spermatogenesis, these men present with infertility as the ejaculate is retrograded into the urinary bladder, due to various causes. Diagnosing this condition involves thorough history taking followed by examination of post-masturbatory/coital urine. Retrieval of spermatozoa from the bladder maintaining its vitality is crucial in providing fertility treatment. Various methods employed in retrieving motile spermatozoa from the bladder in literature is either invasive or cumbersome causing inconvenience to the couple. Here, a simple and non-invasive spermatozoa retrieval from the bladder (SPERB) technique is described in detail. Case report of the couple who conceived using spermatozoa retrieved by this method is discussed.
Keywords
Anejaculation
aspermia
dry orgasm
non-invasive sperm retrieval
retrograde ejaculation
sperm retrieval
sperm retrieval from bladder
sperm recovery
INTRODUCTION
Retrograde ejaculation (RGE) is the commonest cause of Aspermia.[1] It is a type of ejaculatory dysfunction where semen is pushed retrograde into the urinary bladder instead of the normal antegrade flow into the urethra during ejaculation. The absence of antegrade ejaculation causes male infertility. It is a disheartening condition in men and distress to the couple as there is no antegrade ejaculation despite normal and sustained erection followed by the perception of ejaculation. Parnham and Serefoglu[2] quoted the incidence of RGE as 0.3% to 2% of male infertile population. Many cumbersome and invasive methods were used in managing infertility in these men. We use a simple and non-invasive method for spermatozoa retrieval in these men from urinary bladder. Herein, we describe the detailed methodology and the case reports of spermatozoa retrieval from the bladder in patients diagnosed with retrograde ejaculation.
PHYSIOLOGY OF MALE SEXUAL FUNCTION
Male sexual function is a series of complex events that takes place involving psychological, neurogenic, vascular, and hormonal factors.[3] With good libido and sexual stimuli in men, arousal and penile erection is achieved. This is followed by the two phases of events known as emission and ejaculation.
The process of emission takes places with the involvement of distal epididymis, vas deferens, seminal vesicles, prostate gland, prostatic urethra, and bladder neck. Stimuli mediated by the innervations form sympathetic nervous system initiates emission by the closure of bladder neck. Contents from the epididymis, vas deferens, seminal vesicles, prostate, and bulbourethral glands are then deposited into the prostatic urethra.[4]
Ejaculation, also known as seminal emission is initiated by the presence of semen in the prostatic urethra. It is controlled by the coordinated neurological stimuli from T10-L2 (sympathetic fibres) to S2-S4 (somatic fibres).[5] Highly coordinated neurological and muscular events aid in the process of ejaculation. The pelvic floor muscles around the urethra upon rhythmic contractions propels the ejaculate via the penile urethra and external meatus.[6]
PATHOPHYSIOLOGY IN RETROGRADE EJACULATION
The events of sexual function like libido, arousal, and erection are normal in patients with retrograde ejaculation. The process of emission take place but due to inadequate closure of bladder neck, semen flows into the urinary bladder.[7]
The semen deposited into the bladder is exposed directly to the acidic urine, which makes the spermatozoa either immotile or non-vital. In order to treat infertility, it is essential to isolate the spermatozoa from urine and retain spermatozoa motility and viability.
Etiology of retrograde ejaculation is given in Table 1.

DIAGNOSIS
High index of suspicion of retrograde ejaculation is raised when a male partner has good erection and achieves the sense of orgasm and ejaculation but there is aspermia/no antegrade ejaculation − dry orgasm. Eliciting the patient’s medical [Table 1] and surgical history is very essential in confirming the diagnosis with further investigations. History should also include the details of surgeries in bladder neck, spinal cord, urethra, neoplastic excision with irradiation in the pelvic floor.[4] The chances of RGE is ruled out in men with painful antegrade ejaculation, as it could be due to pathologies in the ejaculatory duct.[12]
The spermatogenesis is intact despite which the male remains infertile as there is only defective spermatozoa transportation.[13,14] Final diagnosis of retrograde ejaculation can be elicited in men by detailed history taking and examination of post coital or post masturbatory urine for the presence of spermatozoa. The voided urine, upon macroscopic examination will appear cloudy,[2] and plenty of immotile spermatozoa[15] can be seen when viewed under the microscope.
Though spermatogenesis is usually unaffected in these men, exposure to the acidic pH of the urine in the bladder makes the spermatozoa immotile/non-vital.[16] Hence, if the time of exposure of spermatozoa to urine is minimized, motile spermatozoa can be obtained and can be used for fertility treatment procedures which has evolved over a period of time. Cloudy urine has to be differentiated from milky urine (chyluria), which occurs in filariasis or trauma to the lymphatics of the genital tract.
Many methods have evolved in an attempt to recover motile spermatozoa in patients with retrograde ejaculation and one such method is spermatozoa retrieval from bladder (SPERB), which is described below. A detailed literature review pertaining to fertility management in these men is mentioned in Table 3.
SPERMATOZOA RETRIEVAL FROM THE BLADDER (SPERB) - A SIMPLE NON-INVASIVE TECHNIQUE
This novel technique involves a simple method of spermatozoa retrieval from the bladder in patients diagnosed with retrograde ejaculation. We coined the term “SPERB − Spermatozoa Retrieval from the Bladder.” SPERB is a simple, non-invasive and effective method of spermatozoa retrieval in men with retrograde ejaculation which we routinely perform in Department of Andrology & Reproductive Medicine, Chettinad Super Specialty Hospital, Chennai since 2009. The main principle of this technique is to reduce the time of contact of the spermatozoa with urine in the bladder, thereby retaining spermatozoa motility.
Methodology
Step 1: In a sterile non-toxic wide mouth semen collection container, sperm wash medium of around 30 to 40 ml is incubated at 37°C for 45 minutes.
Step 2: The patient is initially advised to void urine to empty the bladder. This is done to reduce the volume of residual urine in the bladder and in turn minimize the exposure of spermatozoa to the acidic pH of urine.
He is instructed to either masturbate (preferable) or have coitus until he achieves orgasm.
The patient is then instructed to void the post masturbatory/post coital urine into a sterile semen collection container which contains preincubated sperm wash medium. The sperm wash medium acts as a buffer and thereby the acidic pH of urine containing spermatozoa is immediately neutralized.
A mixture of pre-incubated sperm wash medium, semen, and the residual urine from the bladder is now obtained in the semen collection container.
Step 3: To isolate spermatozoa, the sample is then aliquoted by transferring to test tubes and subjected to centrifugation at 1500 rpm for 10 minutes.
Step 4: As a result, pellet will be obtained in each aliquot. Pellet is resuspended in 0.5 ml of sperm wash medium and is examined for spermatozoa concentration, motility, and morphology.
Step 5: Based on the sperm parameters thus obtained, the choice of treatment of the female partner is made. Informed consent was obtained from the patients.
CASE REPORT
A 32-year-old gentleman and his wife, a 27-year-old lady, married for around 3 years visited us with history of primary infertility. The female partner had regular menstrual cycles. Upon eliciting detailed sexual history, male partner revealed that he has no antegrade ejaculation and no night emission despite having orgasm. Uro-genital examination was found to be normal.
Considering the history, provisional diagnosis was made as retrograde ejaculation. Our method of SPERB was performed to confirm the diagnosis. Examination of post masturbatory urine revealed the presence of occasional motile and immotile spermatozoa. The test was repeated and the later showed similar spermatozoa parameters.
Since the spermatozoa numbers were very less, ICSI (Intra Cytoplasmic Sperm Injection) was the treatment of choice for this couple. Controlled ovarian hyperstimulation was done and oocyte retrieval was performed. Spermatozoa were recovered by the above-described method on the day of oocyte retrieval, and the motile spermatozoa obtained was used for ICSI. Details of the ART cycle are mentioned in Table 2.
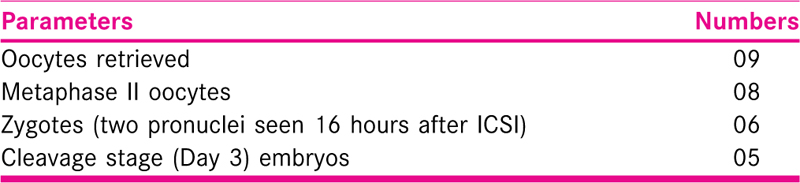
On the third day after ICSI, 05 cleavage stage embryos (03–8 cell grade 1 and 02–6 cell grade 1) were obtained. The rate of fertilization and cleavage was normal. Considering the age of the female partner, type of infertility and quality of embryos, a fresh transfer of 02–8 cell grade 1 embryos was performed. The remaining embryos are cryopreserved. Two weeks from the embryo transfer, serum β hCG levels was assessed and was found to be 579.2 mIU/ml. A healthy live baby boy was born at term by elective Caesarean section.
LITERATURE REVIEW OF MANAGEMENT OF RGE
Upon reviewing the literature in detail (Table 3), it is clear that many methods have evolved over a period of time in managing patients with retrograde ejaculation. But, most of these methods are invasive, cumbersome, and have lot of drawbacks and a majority of them have been withdrawn from current practice.

DISCUSSION
The percentage of men with retrograde ejaculation among the infertile men ranges from 0.3% to 2%.[2] The incidence of azoospermia and aspermia in our center is 10% and 0.3% respectively.
History taking plays a significant role in suspecting and diagnosing this condition. A detailed medical, surgical, and sexual history is important to identify the cause of an ejaculation. Patient’s inability to have an antegrade ejaculation despite having orgasm[3] and passing cloudy urine[2] after the sense of ejaculation due to mixing of semen and urine in the bladder are the key points to diagnose and to suspect retrograde ejaculation.
The final diagnosis of retrograde ejaculation is made by identifying spermatozoa in the post coital/masturbatory urine. In these patients with normal spermatogenesis, plenty of immotile spermatozoa can be seen. As there is mixture of semen with urine in the bladder, the acidic pH of urine renders the spermatozoa immotile/non-viable.[16]
Isolation of motile spermatozoa is essential in these patients to treat infertility. Many methods have been employed for isolation of motile spermatozoa from patients diagnosed with retrograde ejaculation.
The treatment options vary largely from non-invasive to invasive methods, based on the etiology.[17] Most of the methods used were either invasive or unpleasant to the couple seeking treatment. A detailed description of methodology used with their pros and cons are tabulated in Table 3.
SPERB, is a simple yet novel technique and is non-invasive. Spermatozoa retrieval from the bladder is done at ease just by instructing the patients to follow simple instructions. Emptying the bladder and voiding the post coital/masturbatory urine into the media acts as a buffer and reduces the acidic pH of residual urine thereby maintaining spermatozoa motility.
Among men with aspermia, SPERB method is effective in diagnosing retrograde ejaculation. The treatment method for infertility was based on the spermatozoa concentration and motility. ICSI is preferred when the recovered spermatozoa numbers are very few.
Pandiyan et al.[31] introduced SPERB method in another institution and in the year 1998 presented and published the clinical outcome of using spermatozoa retrieved by this method as an abstract. Spermatozoa recovery was done in 06 patients diagnosed with retrograde ejaculation and the spermatozoa concentration and motility was suitable enough for performing intrauterine insemination. Since all the patients reported with primary infertility and had no female factor infertility, intrauterine insemination was offered and 04 pregnancies and live births were obtained.
CONCLUSION
Spermatozoa retrieval in men diagnosed with retrograde ejaculation can be performed by simple and non-invasive methods. Achieving fatherhood by natural conception is not possible in the absence of antegrade ejaculation. SPERB is a simple and easy method to retrieve motile spermatozoa and use it for fertility treatment. The choice of fertility treatment need not be restricted to higher treatment methodologies; a simple IUI should also be considered when the retrieved spermatozoa concentration and motility are favorable.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Commentary
Among the various causes of male infertility, the percentage of men with retrograde ejaculation ranges from 0.3% to 2%. Patient’s inability to have an antegrade ejaculation despite having orgasm and passing cloudy urine after the sense of ejaculation due to mixing of semen and urine in the bladder are thekey points to diagnose and to suspect retrograde ejaculation. But the final diagnosis is made by identifying spermatozoa in the post coital/masturbatory urine. The main objective in these cases would be to obtain viable and motile spermatozoa before the acidic pH of urine renders them immotile/non-viable. In the near past, various treatment options have emerged. But there has been a constant search for a non-invasive, non-cumbersome method for the couple seeking treatment. Spermatozoa retrieval from the bladder (SPERB), described in the article, is a simple yet novel technique and is non-invasive. Emptying the bladder and voiding the post coital/masturbatory urine into the media acts as a buffer and reduces the acidic pH of residual urine, thereby maintaining spermatozoa motility. Although this method was introduced in the year 1998, proper utilisation was limited by a smaller number of studies and the continued use of other methods of sperm retrieval like Hotchkiss method, Glezerman’s methodology, etc. From the comparative analysis of all the invasive and non-invasive methods available, SPERB stands out as a promising option as it does not involve restricting fluid intake, catheterisation of bladder, increased risk of urinary tract infections (UTI) and cumbersome inseminate volume for the female partner. Achieving fatherhood by natural conception is not possible in the absence of antegrade ejaculation. As rightly quoted, the choice of fertility treatment can be a simple intrauterine insemination (IUI) when the retrieved spermatozoa concentration and motility are favourable, before proceeding to higher treatment methodologies and hence reducing the economical and psychological burden.
Dr. Pankaj Talwar, Director, Medical Services, Director, Birla Institute of Fertility Sciences, Gurgaon, Haryana, India
Acknowledgment
The author thanks the faculty and staff of the Department of Andrology and Reproductive Medicine, Chettinad Super Speciality Hospital.
REFERENCES
- Retrograde ejaculation, painful ejaculation and hematospermia. Transl Androl Urol. 2016;5:592-601.
- [Google Scholar]
- Normal male sexual function: emphasis on orgasm and ejaculation. Fertil Steril. 2015;104:1051-60.
- [Google Scholar]
- Ejaculatory physiology and pathophysiology: assessment and treatment in male infertility. Transl Androl Urol. 2014;3:41-9.
- [Google Scholar]
- Male sexual dysfunction and infertility associated with neurological disorders. Asian J Androl. 2012;14:61-8.
- [Google Scholar]
- Neural control and physiology of sexual function: effect of spinal cord injury. Top Spinal Cord Inj Rehabil. 2017;23:1-10.
- [Google Scholar]
- Retrograde ejaculation: pathophysiologic aspects and report of two successfully treated cases. Fertil Steril. 1976;27:796-800.
- [Google Scholar]
- Ejaculatory dysfunction in spinal cord injury men is suggestive of dyssynergic ejaculation. Eur J Phys Rehabil Med. 2011;47:677-81.
- [Google Scholar]
- Retrograde ejaculation following open ureteric reimplantation: a case report. J Med Case Reports. 2009;3:7410.
- [Google Scholar]
- Side effects of alpha-blocker use: retrograde ejaculation. Rev Urol. 2009;11:S14-8.
- [Google Scholar]
- Beyond the clinical classification of azoospermia: opinion. Hum Reprod. 2000;15:2356-9.
- [Google Scholar]
- Approach to male infertility and induction of spermatogenesis. J Clin Endocrinol Metab. 2013;98:3532-42.
- [Google Scholar]
- Development and in vitro testing of a new method of urine preparation for retrograde ejaculation; the Liverpool solution. Fertil Steril. 2008;89:885-91.
- [Google Scholar]
- Infertility in men with retrograde ejaculation: the action of urine on sperm motility, and a simple method for achieving antegrade ejaculation. Fertil Steril. 1978;30:572-6.
- [Google Scholar]
- Management of the dry ejaculate: a systematic review of aspermia and retrograde ejaculation. Fertil Steril. 2015;104:1074-81.
- [Google Scholar]
- Artificial insemination with semen recovered from the bladder. Fertil Steril. 1955;6:37-42.
- [Google Scholar]
- Successful artificial insemination in a diabetic with retrograde ejaculation. Fertil Steril. 1971;22:275-7.
- [Google Scholar]
- Retrograde ejaculation: pathophysiologic aspects and report of two successfully treated cases. Fertil Steril. 1976;27:796-800.
- [Google Scholar]
- Conception following insemination with a freeze-preserved retrograde ejaculate. Fertil Steril. 1978;29:360-3.
- [Google Scholar]
- Retrograde ejaculation: successful pregnancy following combined sympathomimetic medication and insemination. Fertil Steril. 1978;30:96-7.
- [Google Scholar]
- Retrograde ejaculation: a more convenient method for artificial insemination. Eur J Obstet Gynecol Reprod Biol. 1982;14:175-8.
- [Google Scholar]
- Successful pregnancy with sperm retrieved from the bladder after the introduction of a low-electrolyte solution for retrograde ejaculation. Fertil Steril. 1998;69:1149-51.
- [Google Scholar]
- Mini symposium, non-surgical sperm recovery: Part II. Treatment of retrograde ejaculation and anejaculation. Hum Reprod Update. 1999;5:448-74.
- [Google Scholar]
- Successful pregnancies and healthy live births using frozen-thawed sperm retrieved by a new modified Hotchkiss procedure in males with retrograde ejaculation: first case series. Basic Clin Androl. 2015;25:5.
- [Google Scholar]
- Bladder neck collagen injection in the treatment of congenital retrograde ejaculation: a case report. Cureus. 2017;9:e1821.
- [Google Scholar]
- Restoration of antegrade ejaculation after transurethral bladder neck injection of Deflux for retrograde ejaculation: a case report of natural conception. Transl Androl Urol. 2020;9:2270-4.
- [Google Scholar]
- Sperm retrieval from the bladder − a simple non-invasive technique. Fertil Steril. 1998;70:S492.
- [Google Scholar]







