Translate this page into:
Assessing the possible risk factors of male infertility
Address for correspondence: Dr. Trilok Shrivastava, MBBS, Infertility Center, Kathmandu, Nepal. E-mail: trilokshrivastava@hotmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Male infertility encompasses up to 50% of all infertility cases and can be due to a variety of causes. Besides cytogenetic abnormalities, hormonal and environmental factors such as trauma, heat, toxins, radiation and nutritional deficiency have been shown to affect spermatogenesis. This study aims to look for the possible risk factors that impair the normal sperm production, which is reflected in semen analysis.
Materials and Methods:
A total of 601 men underwent semen analysis at Infertility Centre in this prospective case–control study. After undergoing semen analysis, those with azoospermia (AZ), oligozoospermia (OL) and asthenozoospermia (AS) were selected as cases of the study, whereas those with normal semen analysis results were selected as controls. All participants were interviewed with a standardised questionnaire to assess for the known & possible risk factors of infertility & data was analysed.
Results:
Mean & standard deviation (SD) age of the participants was 33.38 ± 5.63 years. History of varicocele was found to be significantly associated with AZ/OL [adjusted odds ratio (ORadj) 5.4] and AS (ORadj 6.9). Similarly, men with a history of mumps orchitis had a significant association with both AS (ORadj 2.13) and OL/AZ (ORadj 2.62). Men who chewed tobacco had about twice more chances of having OL/AZ. Activities related to scrotal heat exposure except hot water bath were not associated with sperm quality [AS (ORadj 0.68) and OL/AZ (ORadj 0.59)]. Motorcycle riders were found to have decreased association with low semen quality AS (ORadj 0.53) and OL/AZ (ORadj 0.50).
Conclusion:
Varicocele, mumps orchitis and tobacco chewing are significant risk factors that have shown to decrease semen quality and can contribute to male infertility.
Keywords
Azoospermia
infertility
male
risk factors
tobacco
varicocele
INTRODUCTION
Infertility is a global burden with a 9% prevalence, and male factor infertility encompasses up to half of these cases.[1] Primary causes of male infertility include congenital, genetic disorders, endocrine disorders, and ageing.[2] The secondary causes are diseases of hypothalamo–pituitary–gonadal axis, drugs such as chemotherapeutic agents, and infiltrating disorders. Risk factors of male infertility include tobacco use, alcohol consumption, obesity, history of varicocele, orchitis, scrotal trauma, increased caffeine intake and others.[3,4,5,6,7,8,9,10]
Semen analysis is one of the initial steps in investigating infertility. According to the WHO, for a semen analysis to be reported as normal, it must have a volume of at least 1.5 mL, sperm concentration of at least 15 million/mL, total sperm of at least 39 million sperm per ejaculate with at least 4% normal forms and 58% live forms, progressive motility of at least 32% and a total motility of at least 40%.[11] Although normal semen analysis does not implicate fertility, abnormal semen analysis is strongly associated with male infertility.[12] This study aims to explore the risk factors of abnormal semen analysis.
MATERIALS AND METHODS
After obtaining ethical approval from the Nepal Health Research Council, we evaluated 601 men with an informed written consent in this prospective case–control study from May 9, 2017, to March 18, 2018, at the Infertility Centre, Nepal. All these men underwent semen analysis after 5 days of abstinence, under the guidelines of ‘WHO laboratory manual for the examination and processing of human semen 2010. Those with abnormalities in semen analysis were identified as the cases, whereas those with normal semen analysis were categorised as the controls in the study. Randomly selected individuals from the general population were also included in the control group.
Those who did not maintain abstinence for at least 5 days and those who were already treated for infertility in the past were excluded from the study.
All participants underwent clinical interviewing by using a standardised questionnaire to assess for following variables, namely BMI, alcohol consumption, cigarette smoking, tobacco chewing, use of tight-fitting underwear, history of varicocele, mumps orchitis, thyroid disorders, diabetes mellitus, hypertension, tuberculosis, recent radiation exposure, history of use of drugs, motorcycle riding, occupational heat exposure (>35°C), regular bathing with hot water, drinking more than two cups of coffee per day and bodily use of laptop. Of the 601 men recruited into the study, only 587 had complete data. Any patient data with incomplete records were excluded from the study. The collected data were entered in SPSS (IBM statistical package for social sciences) and then data checking, cleaning, data re-coding and analysis were performed. Correlation coefficient was calculated to observe the correlation of sperm count and total motility with continuous variables such as age and BMI. Binary logistic regression with 95% confidence interval (CI) and adjusted odds ratio were applied to assess the risk factors independently associated with semen quality and sperm quantity. Normozoospermia was considered as a referent group and was compared with asthenozoospermia (AS) and oligozoospermia (OL)/azoospermia (AZ).
RESULTS
Mean & standard deviation (SD) age of the participants was 33.38 ± 5.63 years, whereas the mean BMI was 25.52 ± 3.64 kg/m2. Only 1.4% of the participants had lower BMI, whereas 46% were overweight and 10% were obese [Table 1].

The mean total sperm count was 45.68 (±29.64) × 106/mL. A total of 77.85% of the participants had sperm count more than 15 million or above, whereas 16.18% had AZ and 5.96% had OL. Similarly, mean sperm motility was 42.61 (±27.16)% with 19.76% participants having less than 40% motility excluding 95 azoospermic participants. There were only 35 participants having both OL and AS. One participant had sperm count less than 15 million but sperm motility was more than 40%. In the final analysis, OL and AZ were counted in the same category for sperm quality, whereas the quality of sperm motility was categorised as normozoospermia and AS.
From the descriptive analysis of risk factors, we found that 35.1% were smokers, 18.1% consumed alcohol regularly and 20.1% had regularly consumed chewable tobacco. Almost 40% and 76% of participants had never consumed alcohol and chewable tobacco, respectively. Similarly, 14.5% used laptop while placing it on lap, and 36.8% of the participants said that they have been exposed to occupational heat. More than 20% said that they wore tight underwear, whereas nearly 60% drank tea/coffee more than twice a day. Similarly, 9.8% were obese, 11.6% and 3.1% had a history of mumps orchitis and varicocele, respectively, 3.9% had undergone scroto-perineal surgery, whereas 7.2% of the participants had a history of chronic diseases. The proportion of participants who rode a motorcycle for 5 years or more was 58.1%, whereas 37.6% had never ridden a motorcycle. Nearly 34% said that they have been doing exercise regularly, whereas 52.8% said they had a frequent hot water bath [Table 2].
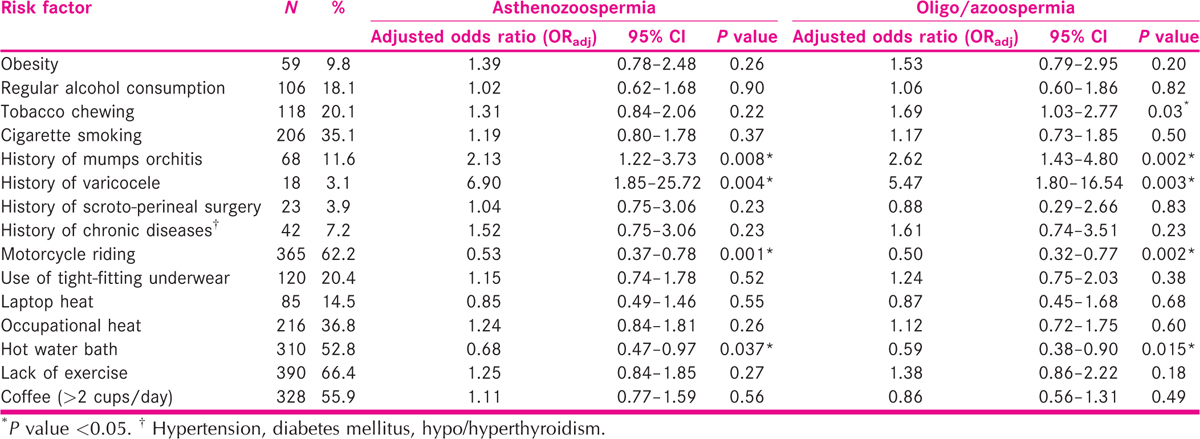
We found that there was a significant positive correlation between sperm motility and sperm concentration with a correlation coefficient (r) of 0.92 (P < 0.01) among analysed semen. No significant correlation of age or BMI was found with sperm concentration or motility. In binary logistic regression, motorcycle riding, hot water bath, history of mumps orchitis and history of varicocele were found to be statistically associated with AS, whereas tobacco chewing, motorcycle riding, hot water bath and history of mumps orchitis, as well as varicocele, were found to be statistically associated with OL/AZ. The odds of men with a history of varicocele were about seven times higher to have AS and about 5.5 times higher to have OL/AZ than the odds of men with a negative history of varicocele (95% CI 1.85–25.72 and 1.80–16.54, respectively). Similarly, the odds of men with a history of mumps orchitis were 2.13 times higher to have AS and 2.62 times higher to have OL/AZ (95% CI 1.22–3.73 and 1.43–4.8, respectively). OL/AZ was 1.7 times more likely to be found in men who consumed chewable tobacco than those who did not (P = 0.03). However, men who ride motorcycle or take hot water bath regularly were less likely to have AZ as well as AS than those who do not. Cigarette smoking, regular alcohol consumption, use of tight-fitting underwear, obesity, history of chronic diseases, past scroto-perineal surgery, lack of physical exercise, laptop heat exposure, occupational heat exposure and consumption of more than two cups of coffee per day were not statistically associated with low sperm motility or concentration.
DISCUSSION
The inability to have children is caused by various factors including physiological, genetic, environmental and social factors affecting both men and women. Men are responsible for 40% to 50% of the failure to conceive child among couples. The most initial and essential step of infertility evaluation in men is semen analysis.[13] According to WHO, the cut-off value for normal sperm count is greater than or equal to 15 million/mL of semen, whereas for sperm motility, the reference limit is considered to be ≥40%.[11] This study compared the possible risk factors of infertility with the abnormal sperm count and motility.
This study found that 16% of the participants had AZ and nearly 6% had OL. A study among the men attending the infertility clinic in Rajasthan found that nearly 4% of the participants had AZ and 14% had OL,[14] whereas another study in central India also found the higher proportion of men with OL than AZ throughout the years.[15] Similarly, only 2.25% of the total study participants had AS in Rajasthan,[14] whereas the proportion of AS was very high in our study (19.76%) when compared. The higher proportion of the abnormal semen quality in our study may be because the study participants had visited the treatment centre as the last option after years of trying to conceive.
BMI and age did not have a significant correlation with sperm concentration and motility in our study. However, a separate study on BMI and sperm parameters found the inverse association between BMI and sperm total count.[16] OL was more common among the male with higher BMI. In addition, with increasing BMI, the prevalence of low progressively motile sperm count was greater.[16] Unlike our study, a study in 2013 found that OL or AZ were more likely for underweight men as well as overweight and obese men compared to those with normal weight.[17] A study performed by Chen et al.[18] found that sperm concentration, total sperm count and motility decrease significantly as age increases. However, a recent systematic review found that sperm concentration did not decline as the age increases, although it found age-associated decline in sperm motility.[19]
A meta-analysis on effects of tobacco smoking and alcohol consumption found that smoking is likely to reduce the sperm concentration and cause impairment of sperm motility.[4] It also found that alcohol consumption has a strong association with reduction of seminal volume and sperm concentration as well as impairment of sperm motility and morphology. A study on the effect of lifestyle factors on semen quality in India showed that sperm count was lower in participants who smoke, chew tobacco and consume alcohol. Similarly, the total progressive motility was significantly reduced in tobacco chewers compared to nonchewers.[20] Our study also found that tobacco chewing was statistically associated with OL/AZ but not with AS. Regular alcohol consumption and cigarette smoking were not found to have a significant association with semen quality in this study.
This study explored the association of abnormal sperm quality with a history of medical conditions such as mumps orchitis, varicocele, scroto-perineal surgery and chronic diseases that include hypertension, diabetes mellitus and hypo/hyperthyroidism. History of varicocele was found to have statistical association with both AS and OL/AZ, whereas history of mumps orchitis was associated with OL/AZ, but the history of scroto-perineal surgery and chronic diseases were not statistically associated with any abnormality in semen quality. A review on risk factors for male infertility showed varicocele, mumps viral infection, diabetes, hypertension and thyroid diseases as the potential risk factors.[21] Another study on risk factors for poor semen quality showed no statistical association between semen quality and history of mumps.[22] A longitudinal study did not find any association of semen quality parameters with chronic diseases such as hypertension and diabetes.[23]
This study also tried to explore the influence of stress and heat exposure to genitalia in sperm quality. The factors like use of tight-fitting underwear, motorcycle riding, bodily use of laptop, exposure to occupational heat and hot water bath were analysed whereas motorcycle riding and hot water bath was found to have a statistical association with both AS and OL/AZ. Surprisingly, participants who rode a motorcycle or took hot water bath regularly were less likely to have poor semen quality. A systematic review on the influence of heat stress on semen quality showed that the negative influence of sauna and tight-fitting underwear were not sufficiently proven, whereas the hot water bath was found to impair the semen quality.[24] Although we could not access the literature on effect of motorcycle riding specifically, it was found on the systematic review that the semen quality of professional drivers were reduced.[24] Unlike our study, an evaluation of the effects of laptop computers connected to the Internet through WiFi showed a significant decrease in sperm progressive motility.[25,26] As our study did not specify the use of WiFi, the result may be less comparable. Similarly, exposure to extreme occupational heat was not found to have an association with sperm quality in other studies.[23,27]Caffeine from coffee intake was not likely to affect the semen quality in our study as well as in a study by Ricci et al.,[9] but another study showed that coffee drinking was related to an increase in the percentage of motile sperm cells along with increase in sperm neck abnormalities.[28] Similarly, when the relationship between physical activity and semen quality was observed, our study showed no association. However, a study by Gaskins et al.[29] showed that higher moderate-to-vigorous activity was likely to be associated with higher sperm concentration. Similarly, exercise-induced BMI decline was associated with increased sperm motility in young male.[30]
CONCLUSION
History of varicocele, mumps orchitis and use of chewable tobacco can significantly decrease the sperm quality. Heat as such, in forms of occupational heat or laptop heat, was not found to affect sperm count or motility. A similar study with a larger sample size needs to be performed for the better establishment of causality of abnormalities seen in semen analysis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
ACKNOWLEDGEMENTS
The authors are thankful to Dr. Angoor Karki, Dr. Dalucky Sherpa, the participants of the study and the entire Infertility Centre staff for their valuable contributions during the study.
REFERENCES
- International estimates of infertility prevalence and treatment-seeking: Potential need and demand for infertility medical care. Hum Reprod. 2007;22:1506-12.
- [Google Scholar]
- Contribution of environmental factors to the risk of male infertility. Hum Reprod. 2001;16:1768-76.
- [Google Scholar]
- Cigarette smoking and semen quality: A new meta-analysis examining the effect of the 2010 World Health Organization laboratory methods for the examination of human semen. Eur Urol. 2016;70:635-45.
- [Google Scholar]
- Risk factors and causes of male infertility − A review. Biochem Anal Biochem. 2016;5:271.
- [Google Scholar]
- Associated factors with male infertility: A case control study. J Clin Diagn Res. 2014;8:FC11-3.
- [Google Scholar]
- Relationship between semen quality and tobacco chewing in men undergoing infertility evaluation. Fertil Steril. 2005;84:649-53.
- [Google Scholar]
- Coffee and caffeine intake and male infertility: A systematic review. Nutr J. 2017;16:37.
- [Google Scholar]
- The influence of varicocele on parameters of fertility in a large group of men presenting to infertility clinics. World Health Organization. Fertil Steril. 1992;57:1289-93. [No authors listed].
- [Google Scholar]
- WHO laboratory manual for the examination and processing of human semen. (5th). Available at: http://www.who.int/reproductivehealth/publications/infertility/9789241547789/en/
- Limitations of semen analysis as a test of male fertility and anticipated needs from newer tests. Fertil Steril. 2014;102:1502-7.
- [Google Scholar]
- Significance of sperm characteristics in the evaluation of male infertility. Fertil Steril. 2006;85:629-34.
- [Google Scholar]
- Clinical pattern and major causes of male infertility in a tertiary referral center in the state of Rajasthan. Indian J Appl Res. 2018;8 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3621293
- [Google Scholar]
- Prevalence of male factor infertility in last ten years at a rural tertiary care centre of central India: A retrospective analysis. Indian J Obstet Gynaecol Res. 2015;2:132-6.
- [Google Scholar]
- Body mass index in relation to semen quality, sperm DNA integrity, and serum reproductive hormone levels among men attending an infertility clinic. Fertil Steril. 2010;93:2222-31.
- [Google Scholar]
- BMI in relation to sperm count: An updated systematic review and collaborative meta-analysis. Hum Reprod Update. 2012;19:221-31.
- [Google Scholar]
- Seasonal variation and age-related changes in human semen parameters. J Androl. 2003;24:226-31.
- [Google Scholar]
- Consistent age-dependent declines in human semen quality: A systematic review and meta-analysis. Ageing Res Rev. 2015;19:22-33.
- [Google Scholar]
- Effect of lifestyle factors on semen quality. Int J Life Sci Scienti Res. 2016;2:627-31.
- [Google Scholar]
- Infertility in male; risk factors, causes and management − A review. J Microbiol Biotechnol Res. 2017;2:641-5.
- [Google Scholar]
- Modifiable and non-modifiable risk factors for poor semen quality: A case-referent study. Hum Reprod. 2012;27:2799-806.
- [Google Scholar]
- Relationship between physical occupational exposures and health on semen quality: Data from the Longitudinal Investigation of Fertility and the Environment (LIFE) Study. Fertil Steril. 2015;103:1271-7.
- [Google Scholar]
- Influence of genital heat stress on semen quality in humans. Andrologia. 2007;39:203-15.
- [Google Scholar]
- The fundamental reasons why laptop computers should not be used on your lap. J Biomed Phys Eng. 2016;6:279.
- [Google Scholar]
- Use of laptop computers connected to internet through Wi-Fi decreases human sperm motility and increases sperm DNA fragmentation. Fertil Steril. 2012;97:39-45.e2.
- [Google Scholar]
- Routine assessment of occupational exposure and its relation to semen quality in infertile men: A cross-sectional study. Turk J Med Sci. 2017;47:902-7.
- [Google Scholar]
- Lifestyle and semen quality: Role of modifiable risk factors. Syst Biol Reprod Med. 2014;60:43-51.
- [Google Scholar]
- Physical activity and television watching in relation to semen quality in young men. Br J Sports Med. 2015;49:265-70.
- [Google Scholar]
- PO-036 exercise-induced BMI declined were association with increased sperm motility in college students: A short paper. Exer Biochem Rev 2018:1. https://ojs.uclouvain.be/index.php/EBR/article/view/10013
- [Google Scholar]







