Translate this page into:
Association Between Number of Oocytes Retrieved with Cumulative Live Birth Rate

*Corresponding author: Dr Deepika Nagarwal, MS, Department of Centre of IVF and Human Reproduction, Sir Gangaram Hospital, Rajinder Nagar, New Delhi, India deepikanayan4oct@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Nagarwal D, Tiwari N, Majumdar A, Majumdar G, Association between Number of Oocytes Retrieved with Cumulative Live Birth Rate. Fertil Sci Res. 2024;11:15. doi: 10.25259/FSR_25_2024
Abstract
Objectives
To find the correlation between oocyte number and cumulative live birth rate (CLBR) in different age groups. It is a retrospective cohort study conducted from January 2022 to December 2022 at Centre of IVF & Human Reproduction, Sir Gangaram Hospital, New Delhi.
Material and Methods
Retrospective data were sought for all women with primary and secondary infertility who underwent assisted reproductive technology treatment from January 2022 to December 2022 at Sir Gangaram Hospital, meeting the inclusion and exclusion criteria. Controlled ovarian stimulation was performed using any suitable gonadotropins - urinary or recombinant with agonist or antagonist protocol used at our centre. To calculate the CLBR, the outcome of fresh and frozen embryo transfer was followed till one live birth or followed till a minimum of 1 year from the day of oocyte retrival (i.e., maximum up to 31 December 2023), whichever is earlier. Age-wise stratification of data was done to find out the association between CLBR and oocyte number in different age groups. Group 1 included women aged 35 years or less, and Group 2 included women aged more than 35 years.
Results
Both the groups in the study were similar in terms of body mass index, stimulation protocol used, and fertilisation protocol used. In group 1, the median oocyte number was 10 per stimulation cycle, whereas in group 2, it was 7. Notably, the oocyte number tends to decrease as age advances. Analysis of the data in both groups, i.e., group 1 (Age ≤35 years) and group 2 (Age >35 years), revealed a significant correlation between oocyte number and no change (p-value <0.001), indicating a strong positive relationship between the variables. This correlation indicates that as the oocyte number in a single stimulation cycle increases, the CLBR also increases.
Conclusion
It was observed that as the oocyte number escalates, there is a corresponding increase in the CLBR across all age groups without any evident plateau. These data can serve as a valuable tool for counselling patients regarding their likelihood of achieving a live birth, based on the oocyte number during one stimulation cycle.
Keywords
Oocyte number
CLBR
ART
IVF
INTRODUCTION
Ovarian stimulation is an important determinant of in-vitro fertilisation (IVF), but still, after many years, there is no consensus on the association between the oocyte number and cumulative live birth rate (CLBR). Also, the data remains elusive on an ideal number of oocytes that should be retrieved in a stimulated IVF cycle for achieving a live birth.[1]
The oocyte number in IVF is a critical parameter that holds profound implications on the IVF outcomes. At present, most clinical decisions on ovarian stimulation are based on tests for ovarian reserve, but these tests do not predict the number of live births, which is the prime objective of every assisted reproductive technology (ART) cycle.[2,3]
The overall trend in studies examining cumulative LBR indicates that there is a positive correlation between the oocyte number and higher cumulative LBR.[4–7]
Women aged 35 and above are known to have a reduced ovarian reserve with a lesser number of retrieved oocytes and are at a greater risk of developing aneuploid oocytes and embryos.[8,9]
Previous studies were mainly done on the Western population, and the association between the CLBR and oocyte number is still not well understood in the Indian population with respect to different age groups. Oocyte number can be used in future as a “surrogate marker” for predicting the CLBR.
In our present study, we aim to evaluate the correlation between the oocyte number to the outcome, that is, the CLBR across different ages in the North Indian population.
Aims and objective
To find the correlation between oocyte number and CLBR per stimulated cycle in different age groups.
Inclusion and exclusion criteria
Inclusion Criteria
Age: 23–45 years.
Diagnosed with primary or secondary infertility.
Had undergone control ovarian stimulation (COS) by suitable protocols of IVF/ICSI (intracytoplasmic sperm injection) used in our centre.
Self-oocyte retrieval.
Fresh or frozen embryo transfer.
Exclusion Criteria
Severe male factor (Azoospermia with surgical sperm retrieval or donor sperms).
Received ovum donor for IVF.
Recurrent implantation failures (≥3 blastocyst transfer failed).
Surrogacy.
Oocyte cryopreservation.
MATERIAL AND METHODS
Study design: Retrospective cohort study.
Period of study: January 2022–December 2022.
Study location: Centre of IVF & Human reproduction, Sir Gangaram Hospital, New Delhi.
Study population: Women who underwent IVF/ICSI cycles in Sir Gangaram Hospital in the specified study period who met the inclusion and exclusion criteria.
Sample size: Retrospective data were looked at for all the women with primary and secondary infertility who underwent ART treatment from January 2022 to December 2022 at Sir Gangaram Hospital. A total of 1004 IVF stimulation cycles underwent oocyte retrieval during the study period. Two hundred ninety-eight cycles were excluded based on exclusion criteria. A total of 706 cycles were studied for the oocyte number and CLBR.
Methodology
Retrospective data were sought for all women with primary and secondary infertility who underwent ART treatment from January 2022 to December 2022 at Sir Gangaram Hospital, meeting the inclusion and exclusion criteria. COS was performed using any suitable gonadotropins – urinary or recombinant with agonist or antagonist protocol used at our centre. To calculate the CLBR, the outcome of fresh and frozen embryo transfer was followed till one live birth or followed till a minimum of 1 year from the day of OCR (i.e., maximum up to 31 December 2023), whichever is earlier.
Age-wise stratification of data was done to find out the association between CLBR and oocyte number in different age groups. Group 1 included women aged 35 years or less, and Group 2 included women aged more than 35 years. Figure 1 shows study flowchart, from January 2022 to December 2022, total 706 patients were included in the study and were divided into two groups.
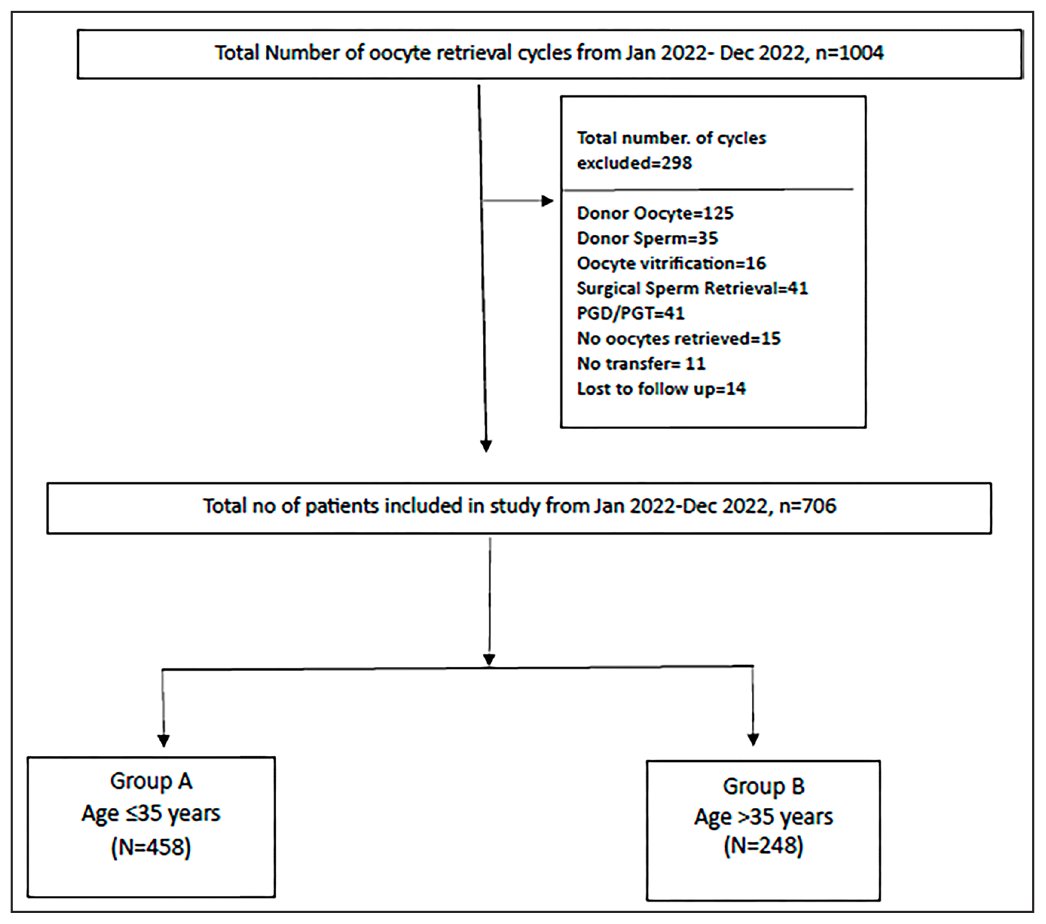
- Study flow chart.
Statistical analysis
Descriptive statistics will be analysed with SPSS version 28.0 software. Continuous variables will be presented as mean ± SD, median (IQR). Categorical variables will be expressed as frequencies and percentages. Nominal categorical data between the two or more variables will be compared using the Chi-squared test or Fisher’s exact test as appropriate. The comparison of normally distributed continuous variables between different age groups will be performed using ANOVA or the Kruskal–Wallis test for non-normally distributed data. For all statistical tests, a p-value less than 0.05 will be taken to indicate a significant difference.
RESULTS
Patients were stratified into two major groups:
Group 1 - Age ≤35 years and,
Group 2 - Age >35 years.
Both the groups in the study were similar in terms of body mass index, stimulation protocol used, and fertilisation protocol used. In group 1, the median oocyte number was 10 per stimulation cycle, whereas in group 2, it was 7 [Table 1]. Notably, the oocyte number tends to decrease with advancing age. In the provided graphical representation, it is evident that the CLBR for fresh/frozen embryo transfer cycles in group 1 (n = 458) was 39.60%, while in group 2 (n = 248), it stood at 27.2% [Figure 2]. This disparity in CLBR signifies a reduction as age advances. Analysis of the data in both groups, i.e., group 1 (Age ≤35 years) and group 2 (Age >35 years), revealed a significant correlation between oocyte number and CLBR (p-value <0.001), indicating a strong positive relationship between the variables. This correlation indicates that as the oocyte number in a single stimulation cycle increases, the CLBR also increases [Figure 3].
| Age | N | Median |
|---|---|---|
| ≤35 years | 458 | 10 |
| >35 years | 248 | 7 |
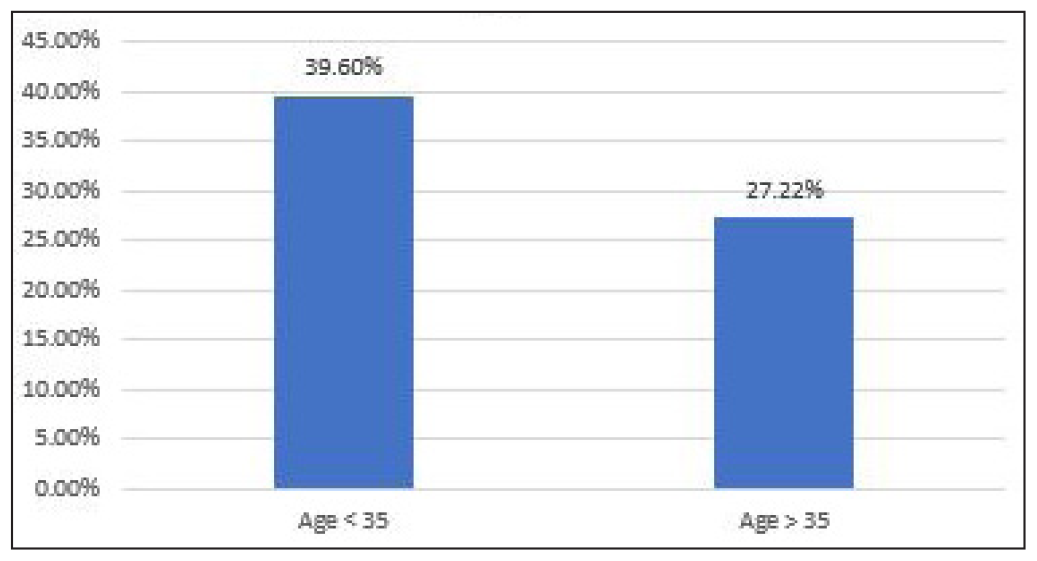
- CLBR in study groups. CLBR: Cumulative live birth rate.
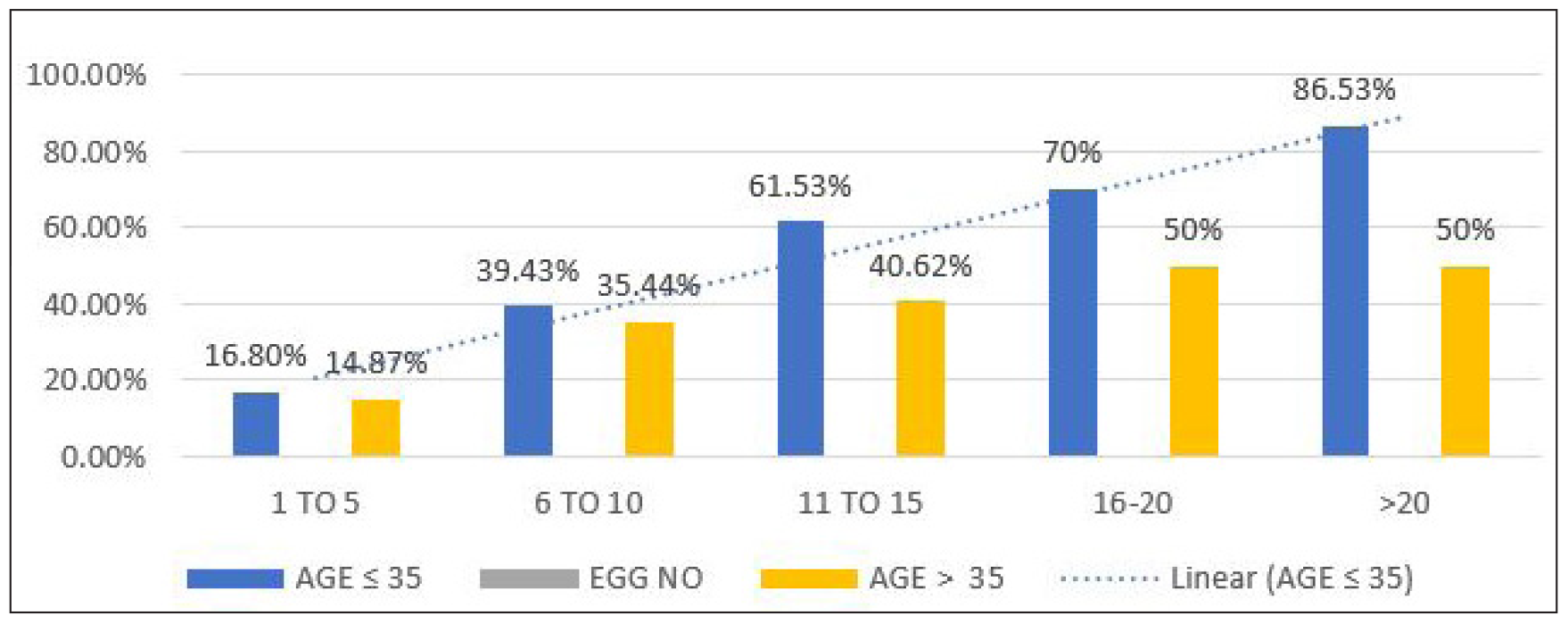
- Correlation between oocyte number and CLBR. CLBR: Cumulative live birth rate. EGG: Oocyte number
DISCUSSION
ART has undergone significant advancements over the past two decades, primarily attributable to enhanced cryopreservation methodologies. These techniques facilitate the cryopreservation of embryos, enabling their subsequent transfer at a later time, thereby contributing to an improved CLBR. Nevertheless, consensus remains elusive regarding the relationship between the oocyte number with CLBR and, the data are lacking on the specific number of retrieved oocytes that can reliably predict the live birth rate.
In our research, the cohort was categorised into two primary groups: group 1 - Age ≤35 years and group 2 - Age >35 years. The distribution revealed that 64.9% of the cases were 35 years or younger, while 35.1% were over 35 years old. Whereas, in a study conducted by Wang et al., 81.2% of cases were 35 years or younger, and 18.8% were 36 years or older.[10]
The median oocyte number in age ≤35 was 10, and at more than 35 years was 7. Gunasheela et al in a study, observed a median number of 8 and 6 oocytes in age ≤35 and >35, respectively.[11]
We observed that the CLBR in women of age 35 years or less in fresh/frozen embryo transfer cycles was 39.60%, whereas CLBR in women of age 36 years or more was observed to be 27.22%, which signifies the reduction in CLBR with advancing age. These observations in our study were consistent with the findings of Wang et al.; they found that CLBR exhibited a marked decline from 68.3% in the group aged 35 or younger to 34.4% in the group aged 36 or older. Notably, it may diminish to below 20% in the cohort aged 40 or above.[10]
We observed a linear relationship between the oocyte number and CLBR in all age groups. The maximum cumulative live birth of 86.53% was attained when more than 20 oocytes were retrieved in women 35 years and less, and CLBR of 50% was attained in women 36 or more when more than 20 oocytes were retrieved. Similarly, Polyzos et al. published a retrospective multicentre analysis in which they analysed 14,469 patients; they studied the first stimulated cycle for IVF/ICSI from 2009 to 2014. The CLBR exhibited a steady increase in the number of oocytes, reaching 70% when more than 25 oocytes were retrieved. Notably, no plateau in cumulative LBR was observed; however, a moderate average increase of 5.1% was detected beyond 27 oocytes.[1]
Our research findings represent a pioneering contribution to the field, being only the second study conducted in the Indian population to investigate the relationship between the oocyte number and the CLBR across different age groups. Additionally, our study also focuses on the correlation between the oocyte number and the generation of utilisable embryos and an overall correlation between the number of oocytes, utilisable embryos, and live birth rate. This information holds the potential to assist clinicians in devising effective strategies for ovarian stimulation and in providing comprehensive guidance to their patients in the future.
CONCLUSION
It was observed that as the quantity of oocytes retrieved escalates, there is a corresponding increase in the CLBR across all age groups without any evident plateau. These data can serve as a valuable tool for counselling patients regarding their likelihood of achieving a live birth, based on the oocyte number during one stimulation cycle.
Ethical approval
The research/study was approved by Independent Ethical Committee, approval number F.1/IEC/IFS/2023/No. 08, dated: 02/12/2023.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
REFERENCES
- Cumulative Live Birth Rates According to the Number of Oocytes Retrieved After the First Ovarian Stimulation for in vitro Fertilization/Intracytoplasmic Sperm Injection: A Multicenter Multinational Analysis Including ~15,000 Women. Fertil Steril. 2018;110:661-670.e1.
- [CrossRef] [PubMed] [Google Scholar]
- A Higher Number of Oocytes Retrieved Is Associated With an Increase in Fertilized Oocytes, Blastocysts, and Cumulative Live Birth Rates. Fertil Steril. 2023;119:762-9.
- [CrossRef] [PubMed] [Google Scholar]
- Association Between the Number of Eggs and Live Birth in IVF Treatment: An Analysis of 400 135 Treatment Cycles. Hum Reprod. 2011;26:1768-74.
- [CrossRef] [PubMed] [Google Scholar]
- Conventional Ovarian Stimulation and Single Embryo Transfer for IVF/ICSI. How Many Oocytes Do We Need to Maximize Cumulative Live Birth Rates After Utilization of all Fresh and Frozen Embryos? Hum Reprod. 2016;31:370-6.
- [CrossRef] [PubMed] [Google Scholar]
- Is there an Association Between Oocyte Number and Embryo Quality? A Systematic Review and Meta-analysis. Reprod Biomed Online. 2019;39:751-63. Available from: https://doi.org/10.1016/j
- [CrossRef] [PubMed] [Google Scholar]
- Can You Ever Collect Too Many Oocytes? Hum Reprod. 2015;30:81-7.
- [CrossRef] [PubMed] [Google Scholar]
- How Many Oocytes are Optimal to Achieve Multiple Live Births With One Stimulation Cycle? The One-and-done Approach. Fertil Steril. 2017;107:397-404.e3.
- [CrossRef] [PubMed] [Google Scholar]
- Maternal Age, Morphology, Development and Chromosome Abnormalities in Over 6000 Cleavage-stage Embryos. Reprod Biomed Online. 2007;14:628-34.
- [CrossRef] [PubMed] [Google Scholar]
- Human Female Meiosis Revised: New Insights into the Mechanisms of Chromosome Segregation and Aneuploidies From Advanced Genomics and Time-lapse Imaging. Hum Reprod Update. 2017;23:706-22.
- [CrossRef] [PubMed] [Google Scholar]
- The Association Between the Number of Oocytes Retrieved and Cumulative Live Birth Rate in Different Female Age Strata. Sci Rep. 2023;13:14516.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Cumulative Live Birth Rate Per Oocyte Aspiration in Artificial Reproduction Technology: A Retrospective Observational Study of the Association Between Maternal Age and the Number of Oocytes Retrieved in an Indian Population. J Hum Reprod Sci. 2022;15:284-92.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]







