Translate this page into:
Efficacy of Hysteroscopy in Improving Fertility Outcomes in Assisted Reproductive Techniques

*Corresponding author: Sergio Haimovich, Department of Obstetrics and Gynecology, Adelson School of Medicine, Ariel University, Ariel, Israel sergio.haimovich@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Haimovich S. Efficacy of Hysteroscopy in Improving Fertility Outcomes in Assisted Reproductive Techniques. Fertil Sci Res. 2025;12:11. doi: 10.25259/FSR_1_2025
Abstract
Objectives
Successful outcomes in assisted reproductive technologies (ART) depend on three interrelated factors: a high-quality embryo, a structurally and functionally optimal uterine cavity, and a receptive endometrium. While embryo quality has traditionally been the principal focus, growing evidence suggests that undiagnosed or untreated intrauterine pathologies—such as congenital uterine anomalies or chronic endometritis—may compromise implantation and pregnancy success. To provide a comprehensive review of the role of hysteroscopy, in combination with advanced imaging modalities (notably three-dimensional ultrasound [3D USG]), in optimising fertility outcomes for patients undergoing ART.
Material and Methods
Literature was evaluated to summarise the diagnostic and therapeutic utility of hysteroscopy, its synergy with imaging techniques (3D USG, saline infusion sonography [SIS]), and its effects on key reproductive endpoints. Particular emphasis was placed on its ability to directly visualise and treat pathologies in a single procedure and its influence on clinical pregnancy rates (CPR) and live birth rates (LBR).
Results
Hysteroscopy, often performed as an office-based procedure without general anaesthesia, demonstrated notable advantages: direct visualisation of the uterine cavity, real-time characterisation of lesions, and immediate therapeutic intervention. When combined with 3D USG, which offers high specificity for diagnosing uterine anomalies and precise measurement of cavity dimensions, hysteroscopy further refines diagnostic accuracy and management. Meta-analyses and cohort studies reported improved CPR and LBR in patients undergoing hysteroscopic evaluation, particularly in those with recurrent implantation failure or suspected uterine abnormalities.
Conclusion
Hysteroscopy serves as a critical ‘bridge’ between imaging and intervention, enhancing the management of intrauterine pathologies that may hinder ART outcomes. Future randomised controlled trials are needed to clarify the role of routine hysteroscopic assessment in broader patient populations and to refine guidelines for integrating hysteroscopy into standard fertility workups.
Keywords
Hysteroscopy
IVF
ART
Reproduction
3D ultrasound
SIS
INTRODUCTION
In the multifaceted field of fertility interventions, emphasis has historically been placed on the embryo as the central determinant of success in assisted reproductive technologies (ART). Nonetheless, achieving successful implantation and ongoing pregnancy depends on a triad of interdependent factors: the embryo, the uterine cavity, and the endometrium. Even a morphologically high-quality embryo may fail to implant or may result in early pregnancy loss if the uterine milieu is compromised by conditions such as uterine fibroids or chronic endometritis.[1] This review examines the role of hysteroscopy, used in conjunction with other diagnostic modalities, in enhancing fertility outcomes among patients undergoing ART.
THE TRIAD OF FERTILITY: EMBRYO, UTERINE CAVITY, AND ENDOMETRIUM
In the multifaceted realm of fertility treatment, the embryo has historically been regarded as the primary determinant of success in ART. However, successful implantation and ongoing pregnancy hinge on three closely interdependent factors: the embryo, the uterine cavity, and the endometrium. Even a morphologically high-quality embryo may fail to implant or may result in early pregnancy loss if the uterine milieu is compromised by pathological conditions such as fibroids or chronic endometritis.[1,2]
A distorted uterine cavity whether due to structural anomalies like fibroids [Figure 1] or an endometrium affected by chronic inflammation [Figure 2] can markedly reduce implantation rates and adversely influence pregnancy outcomes. In this context, hysteroscopy, in conjunction with advanced imaging modalities, provides a comprehensive diagnostic and therapeutic strategy. By directly visualising and, when necessary, correcting intrauterine abnormalities, this combined approach aims to enhance fertility outcomes for patients undergoing ART.
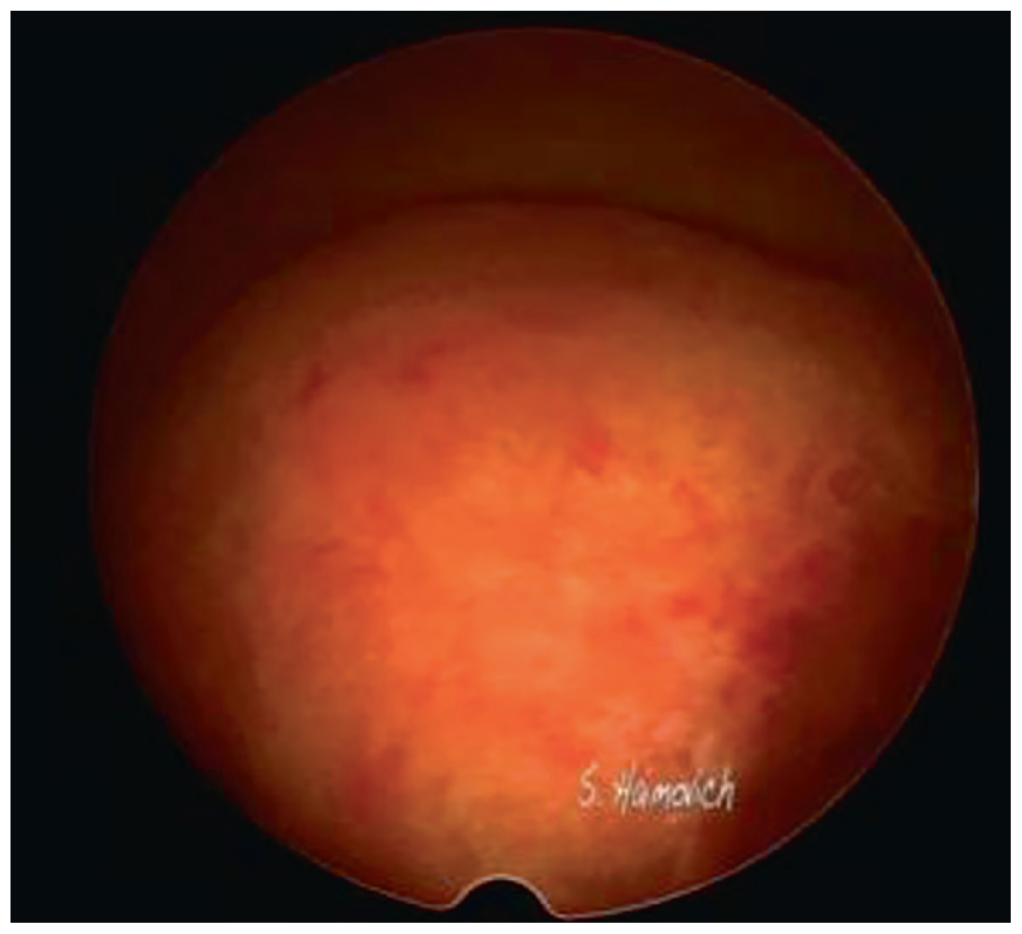
- Big fibroid inside the cavity.
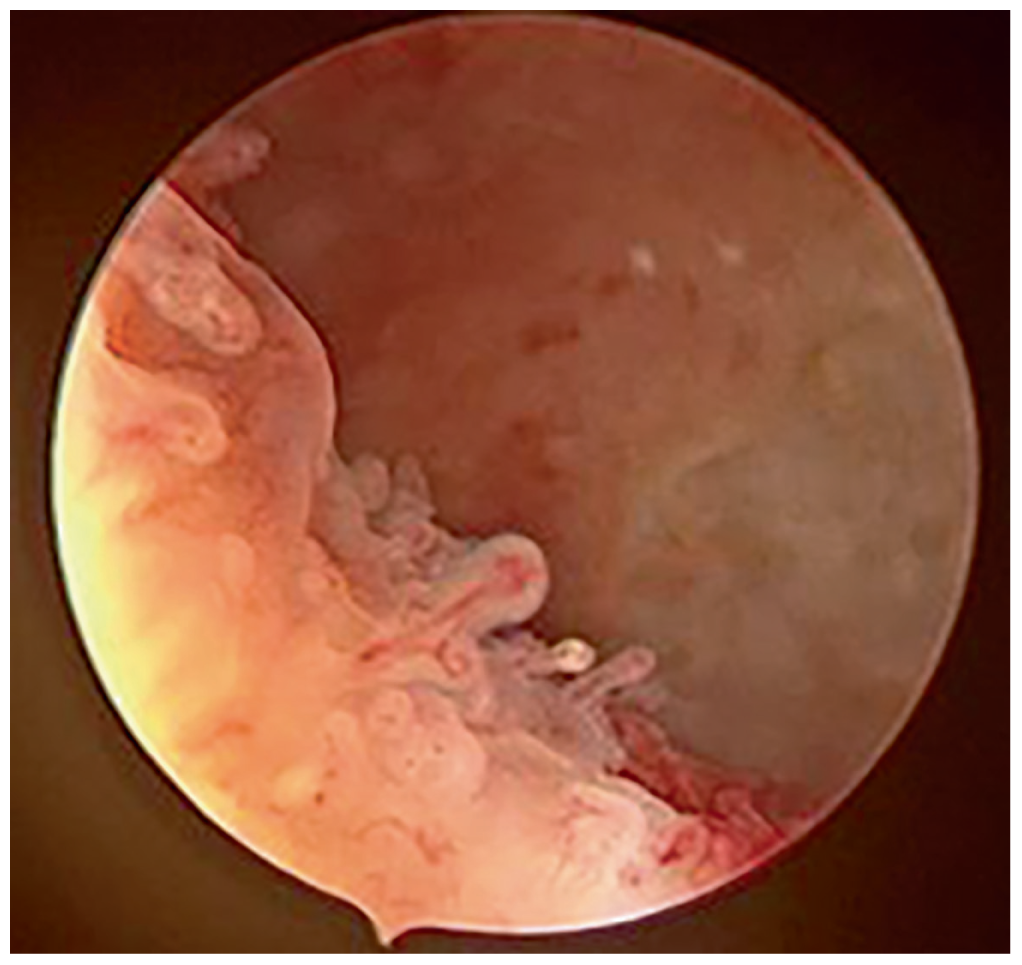
- Micropolyps on the endometrium showing chronic endometritis.
COMPLEMENTARY ROLE OF IMAGING TECHNIQUES
Three-Dimensional Ultrasound (3D USG) in Uterine Cavity Assessment
3D USG has emerged as a valuable imaging modality for evaluating the uterine cavity. By providing detailed visualisation of both the internal cavity and external uterine contour, 3D USG helps clinicians identify structural anomalies that may impact fertility outcomes.[1] Key advantages include:
Coronal view visualisation: Offers a unique perspective, facilitating accurate assessment of uterine shape.
Comprehensive cavity evaluation: Enables precise measurement of both cavity dimensions and external uterine contour.
High diagnostic accuracy: Sensitivity and specificity approaches 100% for diagnosing congenital uterine anomalies, comparable to magnetic resonance imaging and surgical evaluation via laparoscopy.
Two-Dimensional Ultrasound (2D USG) and Endometrial Assessment
While 2D USG remains clinically useful for measuring endometrial thickness, it provides limited information regarding endometrial receptivity and microstructure.[1] This limitation underscores the need for complementary diagnostic techniques, such as hysteroscopy, to fully assess and address endometrial factors influencing implantation.[2]
SIS: Enhancing Diagnostic Capabilities
SIS offers an additional method to improve the sensitivity of ultrasound-based evaluation. By distending the uterine cavity with saline, SIS facilitates the detection of intrauterine pathologies, often with patient discomfort levels comparable to hysteroscopy.[1] However, unlike hysteroscopy, SIS is purely diagnostic and does not allow immediate therapeutic intervention.
HYSTEROSCOPY: THE BRIDGE BETWEEN DIAGNOSIS AND TREATMENT
Hysteroscopy provides a unique, integrated approach to the evaluation and management of uterine pathologies by enabling direct visualisation of the endometrial cavity and simultaneous therapeutic intervention.[3] This real-time ‘see and treat’ capability can streamline patient care, potentially reducing both the time to diagnosis and the need for multiple procedures.
Key Features of Modern Hysteroscopy
-
Office-Based Procedure
Can be performed in an outpatient setting, improving patient convenience and reducing healthcare costs.
-
No General Anaesthesia Required
Minimises anaesthesia-related risks and allows for shorter recovery times.
-
Use of Low-Diameter Scopes
Decreases patient discomfort and reduces the risk of cervical or endometrial trauma.
-
Simultaneous Diagnosis and Treatment
Permits direct visualisation of intrauterine abnormalities and immediate operative intervention when indicated.[2,3]
While hysteroscopy does not provide precise volumetric measurements of the uterine cavity, it offers several critical benefits:
-
Direct Visualisation of the Uterine Cavity
Facilitates detection of lesions that may be missed or underestimated by imaging modalities alone.
-
Accurate Diagnosis of Intrauterine Abnormalities
Enables the definitive identification and classification of pathologies such as polyps, fibroids, adhesions, and congenital anomalies.
-
Detailed Lesion Characterisation
Assesses lesion size, shape, location, and vascular pattern, aiding in the selection of the most appropriate therapeutic approach.
-
Simultaneous Treatment Capabilities
Allows immediate resection or correction of identified lesions, thereby eliminating the need for additional procedures.[2, 3]
IMPROVING ART OUTCOMES THROUGH HYSTEROSCOPY
A growing body of evidence underscores the value of hysteroscopy in optimising ART outcomes, particularly by identifying and managing intrauterine pathologies:
-
Live Birth Rate (LBR)
Moderate-quality evidence indicates that performing hysteroscopy before initiating ART or after an unsuccessful cycle is associated with a higher LBR (RR 1.24, 95% CI: 1.09–1.43).[2, 3]
-
Clinical Pregnancy Rate (CPR)
Hysteroscopic evaluation and treatment have been linked to increased CPR (RR 1.36, 95% CI: 1.18–1.57), suggesting improvements in endometrial receptivity and embryo implantation.[3]
-
Implantation Failure
Among patients with a history of implantation failure, hysteroscopy significantly enhances reproductive outcomes (RR 1.40, 95% CI: 1.12–1.74 for CPR).[3]
-
Treating Intrauterine Pathologies
Although based on low-quality data, operative hysteroscopy for removing or correcting pathologies such as polyps or fibroids has demonstrated an increase in CPR (RR 2.13, 95% CI: 1.56–2.92).[2,3]
Collectively, these findings highlight the critical role of hysteroscopy in ART. By identifying and remedying intrauterine abnormalities that may otherwise impair embryo implantation, hysteroscopy can improve pregnancy rates, enhance LBRs, and reduce the incidence of repeated implantation failure.
SYNERGY OF HYSTEROSCOPY AND 3D USG
The integration of hysteroscopy with 3D USG affords a comprehensive assessment of the uterine cavity:
-
Diagnostic Accuracy
3D Transvaginal Ultrasound: Demonstrates high specificity (99.21%) but comparatively lower sensitivity (88.46%) when detecting uterine abnormalities, as measured against hysteroscopy.[1]
-
Complementary Strengths
3D USG: Offers superior measurement of uterine cavity dimensions and contour.
Hysteroscopy: Allows direct visualisation and concurrent treatment of intrauterine lesions.[1,2]
CONCLUSION
Hysteroscopy, in conjunction with 3D USG and other diagnostic modalities, plays a pivotal role in optimising fertility outcomes for patients undergoing ART. By combining both diagnostic precision and therapeutic capability, hysteroscopy bridges the gap between imaging findings and active management, with the potential to enhance perinatal outcomes.
The synergy of hysteroscopic evaluation and ultrasound-based imaging supports a more holistic approach to fertility, addressing the three principal factors required for successful implantation and pregnancy: the embryo, the uterine cavity, and the endometrium. As research continues to evolve, the integration of hysteroscopy into standard fertility evaluations may gain even greater clinical relevance.
Current evidence endorses the judicious use of hysteroscopy, particularly in cases of recurrent implantation failure or before ART in women with suspected uterine anomalies. Nonetheless, additional high-quality randomised controlled trials are necessary to delineate the exact role of routine hysteroscopic evaluation in diverse patient populations and to further clarify its utility in initial fertility assessments.
This is an invited article to the author, on the topic presented in the Indian Fertility Society Conference.
Author contribution
SH: Literature review and writing of the manuscript.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that they have used artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript or image creations. AI was used for medical edition.
REFERENCES
- Whether Hysteroscopy Improves Fertility Outcomes in Infertile Women: A Meta-Analysis and Systematic Review. Front Endocrinol (Lausanne). 2024;15:1489783.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Outpatient Hysteroscopy Impact on Subsequent Assisted Reproductive Technology: A Systematic Review and Meta-Analysis in Patients With Normal Transvaginal Sonography or Hysterosalpingography Images. Reprod Biol Endocrinol. 2024;22:18.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Efficacy of Hysteroscopy in Improving Fertility Outcomes in Women Undergoing Assisted Reproductive Technique: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Gynecol Obstet Invest. 2023;88:336-48.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]







