Translate this page into:
FFP as an alternative to albumin in management of severe OHSS − what an IVF specialist should know?
Address for correspondence: Nairuti Sompura, MD, Clinical Fellow, Department of Reproductive Medicine and Surgery, KJK Fertility and Research Centre, Trivandrum – 695015, Kerala, India. E-mail: nairuti90@gmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Ovarian hyperstimulation syndrome (OHSS) may occur in the luteal phase or in setting of early pregnancy. In severe late-onset OHSS, albumin supplementation may be required to maintain intravascular oncotic pressure, but cases with albumin allergy still lack approved treatment. With this in mind, we discussed here the role of fresh frozen plasma as an albumin substitute in a patient with late-onset OHSS who developed severe albumin allergy. We also evaluated the efficacy and safety of pigtail catheter drainage for the management of ascites complicating severe OHSS.
BACKGROUND
Ovarian hyperstimulation syndrome (OHSS) is a dreaded iatrogenic complication of controlled ovarian stimulation (COS) resulting in significant morbidity and mortality. Clinically significant OHSS is prevalent in 3% to 6%.[1] Early-onset type occurs within 3 to 7 days of exogenous HCG administration, which is a self-limited type and happens in any stimulated cycle requiring only supportive management, but late-onset OHSS (after 7th day) arising in a setting of pregnancy is likely to be severe and prolonged, demanding a multifaceted and individualized treatment approach (RCOG, 2016). Several strategies have been described depending upon the severity. Macromolecule-like albumin has been the main hyperosmotic agent to maintain intravascular volume over other colloids owing to its longer intravascular persistence. There is a paucity of literature on the management of OHSS-induced hypoalbuminemia in cases of allergic reactions to albumin. Limited data suggest using fresh frozen plasma (FFP) as an alternative to albumin supplementation in such cases. We herein present a case of late-onset OHSS in the context of multiple pregnancy managed by FFP supplementation in a patient with severe albumin allergy. Informed consent was obtained from the patient.
CASE PRESENTATION
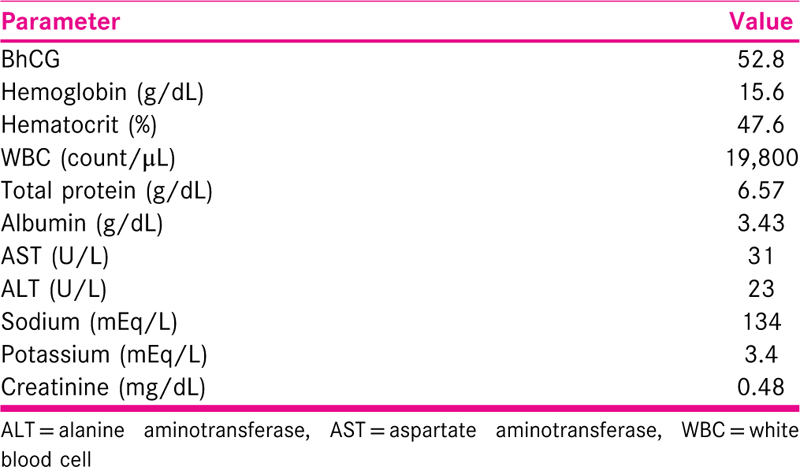
This is a 29-year-old lady with regular menstrual history who presented to our institute with primary infertility of 6 years. At initial evaluation, antimullerian hormone (AMH) was 6.85 ng/mL and antral follicle count (AFC) was 18. Operative laparoscopy was done after six failed IUI cycles with bilateral ovarian drilling. She was started on controlled Ovarian stimulation (COS) with antagonist protocol with recombinant follicle stimulating Hormone (FSH) and hMG. On stimulation Day 10, ovulation was triggered using 250 mcg of recombinant hCG and underwent ultrasound-guided oocyte retrieval 36 hours later. Total 11 mature oocytes were retrieved and a fresh blastocyst transfer was scheduled 5 days later on patient’s request. Seven days after the embryo transfer, patient presented with abdominal fullness and vomiting with lower abdominal pain and reduced urinary output. Abdominal girth increased from 84 to 95 cm. Ultrasonography revealed bilateral ovarian enlargement with gross ascites and bilateral pleural effusion [Figure 1] and other laboratory investigations [Table 1] favored severe late-onset OHSS. She was started on prophylactic anticoagulation with low molecular weight heparin (LMWH) 2500 IU subcutaneously along with intravenous fluids and analgesics. Repeated ultrasound-guided abdominal paracentesis with drainage of 2.5 L of fluid each time was done in view of rapid reaccumulation of ascitic fluid. In view of falling albumin levels, albumin infusion along with paracentesis was started; however, she developed severe allergic reaction, necessitating discontinuation, in the form of itching, redness, and bronchospasm which was managed by IV hydrocortisone 100 mg stat. Further cycles (tapping 2–2.5 L each time) were carried out with oral protein supplementation, which did not suffice and albumin levels dropped down to alarming levels − 2.01 g/dL. As a last resort, decision to use FFP as an /alternative for albumin supplementation was taken. Total 30 FFP were transfused in a span of 7 days intravenously immediately after thawing. Transfusion volume was calculated (22 mL/kg).[2] Patient’s condition improved dramatically and albumin levels also rose. In order to avoid multiple paracentesis, we also offered her pigtail catheter insertion for ascitic fluid drainage. On symptom resolution, pigtail catheter was removed on Day 23 and she was discharged. Currently, it’s an ongoing pregnancy with Live IU DCDA twins [Figure 2].

- USG showing bilateral ovarian enlargement with ascites

- USG at 6 weeks showing Live IU DCDA twins
DISCUSSION
Severe OHSS is a rare iatrogenic complication in ART cycles requiring hospitalization. State of hyperpermeability leads to hamoconcentration, oliguria, ascites, renal failure, thrombosis, and sometimes maternal death.
Intravenous volume replacement with correction of hypoalbuminemia and electrolyte imbalance by fluids, colloids, or proteins along with thromboprophylaxis is the main stay to maintain adequate renal perfusion. In severe OHSS, multiple paracentesis may be required for complete drainage to relieve symptoms and avoid serious sequelae of hemoconcentration, hypotension, decreased renal perfusion, and severe respiratory compromise.
In our case, worsening of hypoalbuminemia despite oral protein supplementation along with repeated reaccumulation of ascites despite repeated paracentesis made us resort to albumin infusion and pigtail catheter insertion. Recurrent ascites may require repeated paracentesis in which volume of the fluid removed at a time should be limited to 5 to 6 L along with administration of volume expanding agents.
Albumin, blood-derived plasma expander, in doses of 6 to 8 g/L of ascitic fluid drained is the choice of replacement to maintain intravascular volume.[3] The European Association for the Study of the Liver (EASL) guidelines recommend the administration of 8 g of HA per litre of ascites removed, with a greater strength of recommendation for paracentesis of at least 5 L. One in 6600 may have a minor or major reaction. Severe life-threatening reactions occur in 1 in 30,000 patients.[4]
In this patient also, severe reaction to albumin precluded its use. In such cases of albumin allergy, a substitute for volume expansion and correction of hypoalbuminemia became necessary. HES was considered but due to falling albumin levels below 2g/L and reports of adverse events like nephrotoxicity and coagulopathy, FFP was considered. FFP served a dual purpose of albumin replacement and volume expander. Decision was taken after weighing all the pros and cons and lack of viable alternatives.
FFP contains all of the clotting factors, fibrinogen (400 to 900 mg/unit), plasma proteins (particularly albumin), electrolytes, physiological anticoagulants (protein C, protein S, antithrombin, tissue factor pathway inhibitor), and anticoagulants. Not a first line in correction of hypoalbuminemia or volume expander, FFP can be considered as a substitute in patients with severe albumin allergy as it contains ∼30 g/L (3.0 g/dL) of albumin. Around
22 mL/kg of plasma to raises the albumin concentration by 5 g/L (0.5 g/dL)]. As a source of albumin, FFP administration appears to be relatively safe, although large volumes might be necessary. Kamath et al. in his report showed dramatic improvement in patients’ clinical condition with use of FFP and demonstrated this alternative therapeutic measure before drastic measures like oophorectomy were called for.[5]
Certain complications are more likely with plasma than other blood components like TRALI (transfusion-related acute lung injury), TACO (transfusion-associated circulatory overload), and allergic/anaphylactic reactions. As large volumes would be needed for correction, these complications should be borne in mind and effective preventive strategies such as appropriate infusion rates and diuretic use in susceptible patients are recommended.
In critical cases of OHSS, instead of multiple paracentesis, pigtail catheters can be used to provide immediate relief and to avoid serious adverse effects.[6]
CONCLUSION
Although rare, this case highlights the role of FFP transfusion for albumin supplementation and volume replacement while managing severe OHSS. Seeking effective alternative strategies over termination of pregnancy in late-onset OHSS is a constant dilemma. Only disadvantage is if the goal of the plasma transfusion is to achieve adequate albumin supplementation, substantial volume per kilogram is needed, particularly when dealing with ongoing albumin loss. Further, it also emphasizes the usefulness of pigtail catheter in hands of reproductive endocrinologists in patients requiring multiple paracentesis.
Financial support and sponsorship
Nil.
Conflicts of interest
The authors report no conflicts of interest.
COMMENTARY
“FFP as an alternative to albumin in management of severe OHSS what an IVF specialist should know?”
This case report and discussion highlights several lessons in the prevention and management of severe Ovarian hyperstimulation stimulation syndrome (OHSS), including the crucial role of endogenous Human Chorionic gonadotropin (HCG) in pathophysiology, the benefit from paracentesis, role of indwelling catheter to drain ascites, and the lack of evidence to support standard management. The authors have chosen among these to focus on what options the clinician has when face an woman with severe OHSS and who is allergic to human albumin solution. They used fresh frozen plasma (FFP), a product that is typically reserved for severe coagulation disorders. A few considerations come to the mind − when we administer albumin, or FFP, to a patient of OHSS − what are we treating? Is it the low serum albumin level in itself? This is almost certainly the result of transient liver dysfunction and increased vascular permeability, which will improve as the OHSS improves. Or is it with the aim of increasing oncotic pressure and reducing ascites? If so, then any colloidal volume expander (such as HES) is likely to be beneficial. It goes without saying that there is little evidence on which to base practice, but in the meantime clinicians must treat their patients safely and effectively. The authors are to be commended for sharing their experience, and more importantly, their rationale, in such a case.
Dr Raj Mathur, Consultant Gynaecologist, Subspecialist in Reproductive Medicine & Surgery, at Manchester University NHS Trust, & Hon Senior Lecturer, at University of Manchester.
REFERENCES
- gtg_5_ohss., pdf [Internet]. [cited 2022 Nov 25]. Available from: https://www.rcog.org.uk/media/or1jqxbf/gtg_5_ohss.pdf
- Guidelines for the use of fresh-frozen plasma, cryoprecipitate and cryosupernatant. Br J Haematol. 2004;126:11-28.
- [Google Scholar]
- [Internet]. [cited 2021 Dec 5]. Available from: https://www.cochrane.org/CD001302/MENSTR_intravenous-plasma-expanders-preventing-ovarian-hyperstimulation-syndrome-ohss
- Unsuspected adverse effect of albumin in severe ovarian hyperstimulation syndrome: a case report. JBRA Assist Reprod. 2019;23:430-3.
- [Google Scholar]
- Management of severe ovarian hyperstimulation syndrome with thawed plasma. J Hum Reprod Sci. 2013;6:82.
- [Google Scholar]
- Outpatient Management of Severe Ovarian Hyperstimulation Syndrome (OHSS) with Placement of Pigtail Catheter. Facts Views Vis ObGyn. 2014;6:31-7.
- [Google Scholar]






