Translate this page into:
Medical management of ectopic pregnancy with two different regimens of methotrexate: A comparative study
Address for correspondence: Dr Pinkee Saxena, MD, MBBS, Department of Obstetrics and Gynecology, Deen Dayal Upadhyay Hospital, Hari Nagar, New Delhi, Delhi 110064, India. E-mail: drpnkee@hotmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
The timely and early diagnosis of ectopic pregnancy has made medical management of ectopic pregnancy the preferred treatment. Methotrexate is used in various regimens to treat ectopic pregnancy. A study was carried out to compare the effectiveness of double-dose and single-dose methotrexate regimen in medical management of unruptured ectopic pregnancy.
Materials and Methods:
The study included 80 hemodynamically stable patients with unruptured ectopic pregnancy. They were then randomly assigned in to two groups. Group A patients received two doses of methotrexate 50 mg/m2 on day 1 and day 4 whereas group B patients received single dose 50 mg/m2 methotrexate on the day 1. Serum β human chorionic gonadotropin (β-hCG) and blood parameters were measured in both the groups on day 4 and day 7 followed by serial serum β-hCG weekly till negative value was obtained. Outcome measures were success rate of treatment, need for extra dose of methotrexate, need of laparotomy, and side effects of methotrexate.
Results:
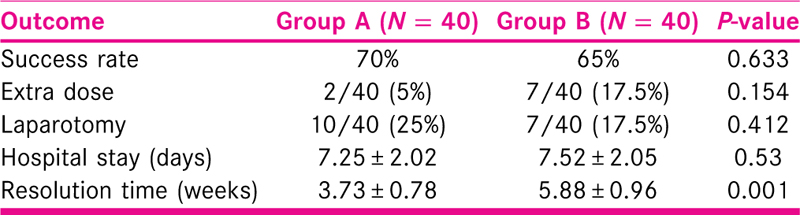
The two groups were comparable in demographic parameters, baseline serum β-hCG, and blood parameters. The treatment success rate was slightly more in group A (70%) than group B (65%); however, it was statistically insignificant. Need of extra dose of methotrexate was 5% in group A and 17.5% in group B, respectively. Ten patients in group A and seven patients in group B underwent laparotomy for rupture of the ectopic mass. The reported side effects of methotrexate was comparable in both the groups.
Conclusion:
Study shows that double-dose methotrexate is as effective as single dose in the medical management of ectopic pregnancy. It has slightly better success rate though statistically insignificant, with less need for extra dose and less duration of follow-up.
Keywords
Doses
ectopic pregnancy
medical management
methotrexate
INTRODUCTION
Ectopic pregnancy is defined as pregnancy that occurs outside the true uterine cavity. It is one of the leading causes of maternal morbidity and mortality which accounts for 3.5% to 7.1% of maternal deaths in India.[1] It is common in cases who have undergone IVF or assisted reproduction and in those with tubal factor. Fallopian tube is the most common location for ectopic pregnancy. The clinical picture is very unpredictable ranging from no symptom at all to acute abdomen with shock. Transvaginal ultrasonography and serum β human chorionic gonadotropin (β-hCG) levels help in early and accurate diagnosis of ectopic pregnancy.[2] Early diagnosis allows us to manage these patients conservatively, either expectantly or medically using methotrexate. Medical therapy of ectopic pregnancy is appealing over surgical options. It offers good success rate with preserved future fertility potential. Methotrexate is a folate antagonist which acts by blocking DNA synthesis by inhibiting the enzyme dihydrofolate reductase. It acts on rapidly dividing cells at the implantation site, most notably trophoblast cells. This drug is used in medical management of ectopic pregnancy due to its antiproliferative property in different doses.[3] Studies have been done to compare double-dose and single-dose regimens. Study done by Kasum et al.[4] has shown high success rate with single dose while others[5,6,7] have found double dose more effective. We carried out this study to compare effectiveness of double-dose and single-dose methotrexate in medical management of unruptured ectopic pregnancy.
MATERIALS AND METHODS
A prospective randomized comparative study was conducted in a tertiary care hospital in New Delhi. The study period was 18 months. Patients attending the outpatient department who were diagnosed as ectopic pregnancy were recruited for the study. The diagnosis of ectopic pregnancy was done by transvaginal ultrasonography and serial serum β-hCG. Inclusion criteria for the study was unruptured tubal ectopic pregnancy, hemodynamically stable patient, absent cardiac activity, and serum β-hCG in the range from 1500 to 10,000 mIU/mL. Patients having non-tubal ectopic pregnancy, ruptured tubal ectopic pregnancy, and hemodynamically unstable patients were excluded from the study. In addition, patient with deranged laboratory parameters, immunodeficiency, active pulmonary disease, lactating women, and not willing to follow-up were also excluded from the study.
The study was approved by the ethical committee of the hospital. Informed written consent was taken from willing patients. A detailed history was taken and complete examination was done in patient fulfilling the inclusion criteria. Baseline serum β-hCG, complete blood count, liver function tests (LFT), kidney function tests, and ultrasound were done in all patients. Randomization was done by envelope method and they were assigned in to two groups. Group A − to receive double dose methotrexate, and group B − to receive single dose methotrexate. Total 80 patients were recruited for this study, 40 in each group.
Sample size was calculated using anticipated proportion of success rate of ectopic pregnancy in both groups. Forty subjects per group was sufficient to detect significant difference of 20% (75% versus 95%)[8] in success rate of two groups to compare efficacy of two regimens of methotrexate in medical management of unruptured ectopic pregnancy using two-tailed alpha value (0.05) and beta value (0.2).
Patients in group A received two doses of methotrexate, 50 mg/m2 methotrexate on day 1 and on day 4, whereas patients in group B received 50 mg/m2 methotrexate on the day 1. Serum β-hCG, LFT, complete blood count were done in both the groups on day 4 and day 7. Serial serum β-hCG was done weekly till negative value was obtained (<5 mIU/mL).
Outcome measures were success rate, need for extra dose of methotrexate, need of laparotomy, and side effects of methotrexate. More than 15% decrease in β-hCG level between day 4 and day 7 was considered as treatment success. Patients who required surgery in view of rupture of the tubal ectopic pregnancy and those who required an extra dose of methotrexate when the fall of β-hCG was <15% were labelled as treatment failure. General condition and laboratory parameters of the patient were taken into consideration before giving extra dose of methotrexate.
Statistical analysis was done by SPSS software version 21.0. Quantitative variables were compared using independent t test/Mann–Whitney U test between the two groups. Qualitative variables were correlated using chi-square test/Fisher exact test. P-value < 0.05 was considered statistically significant.
RESULTS
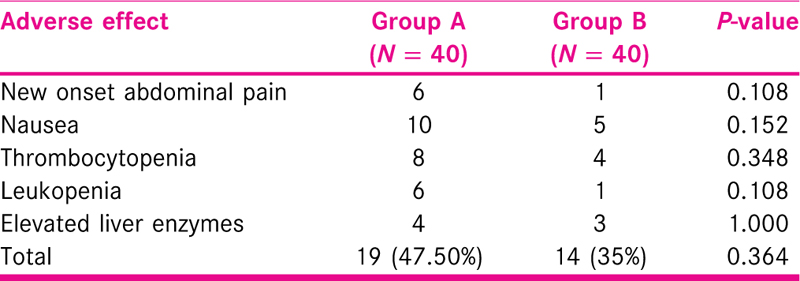
A total of 80 patients were recruited in this study, 40 in group A and 40 in group B. The demographic parameters including age, parity, body mass index(BMI), period of gestation, and history of previous ectopic pregnancy were comparable in both the groups. Patients mainly presented with the complaint of pain in abdomen and bleeding per vaginum. The size of the ectopic mass, endometrial thickness, baseline β-hCG, and laboratory parameters between the two groups were similar as shown in Table 1. The treatment success rate was slightly more in group A (70%) than group B (65%); however, it was statistically insignificant (P = 0.633). In group A, a rapid decline in the levels of serum β-hCG was seen between day 4 and day 7 whereas in group B, the decline of β-hCG was steady [Figures 1 and 2]. The need of extra dose of methotrexate (in case of <15% decline, plateau or increase in β-hCG) was 5% in group A and 17.5% in group B, respectively. Less patients in group A required extra dose of methotrexate; this was, however, statistically insignificant. Ten patients in group A (25%) and seven patients in group B (17.5%) underwent laparotomy for rupture of the ectopic mass. In group A, duration of follow-up was less as compare to group B (3.73 weeks versus 5.88 weeks) [Table 2]. New onset pain, nausea, and change in laboratory parameter were few of the side effects noted. The reported side effect was more in group A than group B; however, it was not statistically significant [Table 3].
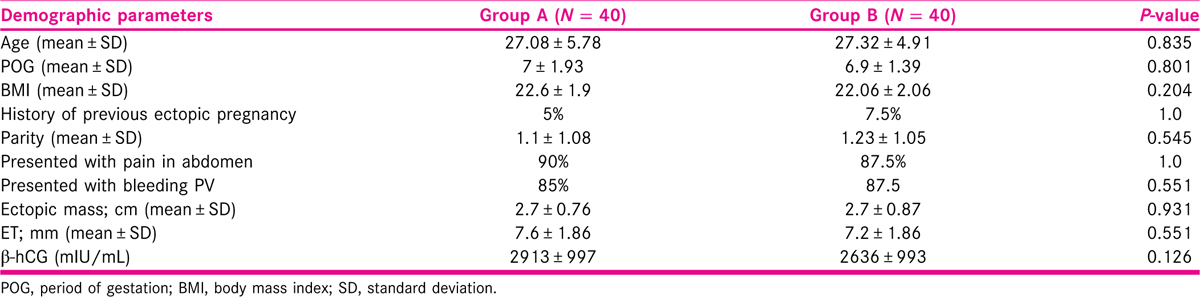
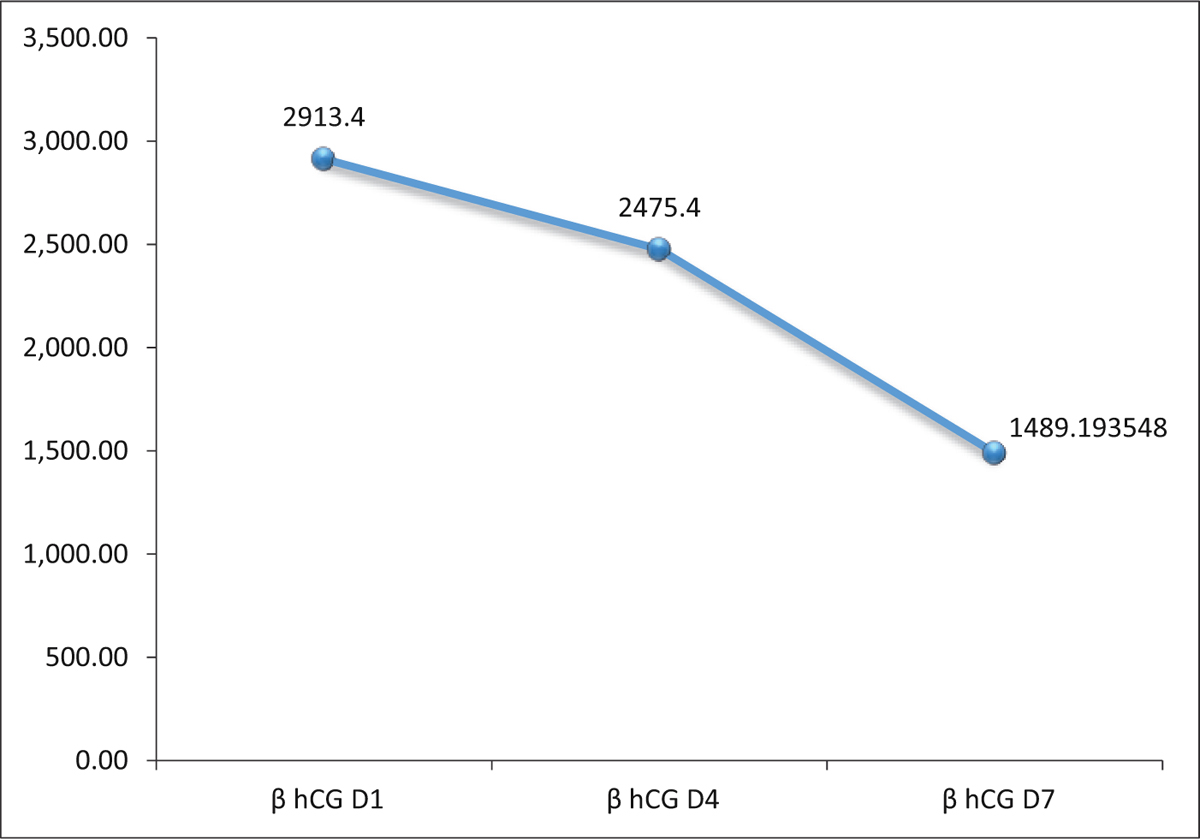
- Declining trend of β-hCG in group A over 7 days
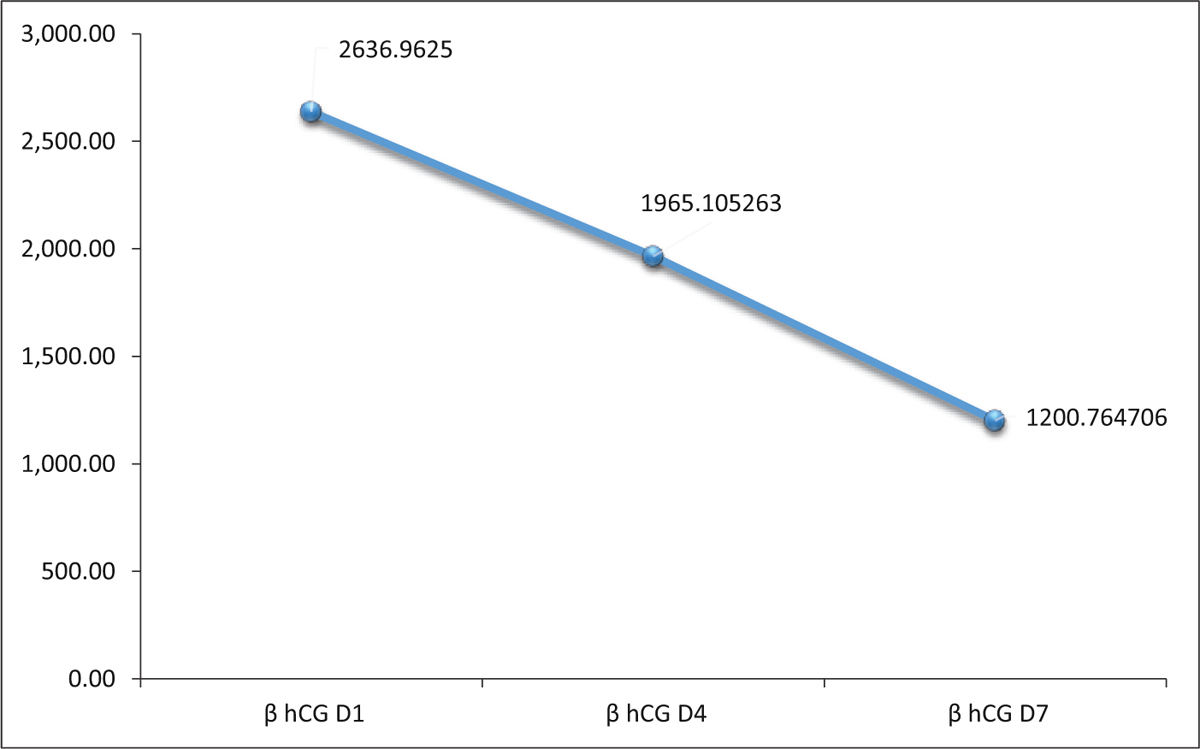
- Declining trend of β-hCG in group B over 7 days
DISCUSSION
Successful use of methotrexate in medical management of interstitial ectopic pregnancy was first reported in 1982 by Kimura et al.[9] Since then methotrexate has been used for the medical management of ectopic pregnancy. Medical management of an ectopic pregnancy is more cost-effective than surgical management. Various regimens that have been used in the management of ectopic pregnancy are single-dose regimen, two-dose regimen, and fixed multiple dose regimens. The two-dose regimen was initially proposed by Barnhart et al.[10] in 2007 to optimize the balance between convenience, adverse effects, and efficacy.[3]
We studied the effectiveness of double and single dose of methotrexate in medical management of ectopic pregnancy. In this study, baseline serum β-hCG level in group A and group B was 2913 mIU/mL and 2636 mIU/mL, respectively. This was slightly more than the study of Mergenthal et al.[11] (1869 versus 1684 mIU/mL) but lower than the study of Saadati et al.[12] (3311 versus 3249 mIU/mL).
Successful treatment was seen in 70% of patients in group A and 65% in group B. Similar observation was made by Saadati et al.[12] (success rate: 79% versus 69%). Other studies have higher success rate.[8,13]
The extra dose of methotrexate needed was less in double dose as compare to the single dose (5% versus 17.5%). This was similar to the studies by Saadati et al.[12] (6%) and Song et al.[6] (6.5%). The baseline β-hCG was 3314 ± 593.96 mIU/mL in group A and 2383.28 ± 504.88 mIU/mL in group B in women who required extra dose of methotrexate. More patients in group B required extra dose which probably suggests that double dose may have better resolution of ectopic pregnancy than single dose.
Need of laparotomy was less in double dose group when compared to single dose group. Similar results were obtained by other authors.[6,8,12] The baseline β-hCG in patients requiring laparotomy was 3847 ± 1143.78 mIU/mL in group A and 3970.85 ± 1600.38 mIU/mL in group B, (P = 0.04). A higher initial β-hCG value at times is associated with failure of medical treatment.[14]
Side effects of drug were mild and transient in patients. The frequency of adverse effects was comparable in both groups (47% versus 35%) which was statistically insignificant. Nausea and new onset pain were the most frequent side effect observed. It is often very difficult to differentiate the pain of separation from the pain of rupture of the ectopic mass. Others were thrombocytopenia, raised liver enzymes, and leukopenia. It was observed that the adverse effects noted were not related to the dose of methotrexate administered (P = 0.364).
Resolution time for β-hCG to normal level was lower in double dose compared to single dose (3.75 versus 5.8 weeks). This was found to be statistically significant, P-value < 0.001. Other studies[12,13] have also shown similar results. It was observed that the resolution time of β-hCG level to normalcy was less in double dose. Also the patients with high level of β-hCG often showed a rapid decline. Even the requirement of repeat dose of methotrexate was less in double dose regimen. Follow-up duration was also less in double-dose group as compared to single dose.
In conclusion, double-dose methotrexate is as effective as single dose in the medical management of ectopic pregnancy. It has slightly better success rate though statistically insignificant, with less need for extra dose of methotrexate and less duration of follow-up.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Clinical analysis of ectopic pregnancies in a tertiary care centre in Southern India: a six-year retrospective study. J Clin Diagn Res. 2016;10:QC13-16.
- [Google Scholar]
- Clinical factors affecting the accuracy of ultrasonography in symptomatic first-trimester pregnancy. Obstet Gynecol. 2011;117:299-306.
- [Google Scholar]
- ACOG Practice Bulletin No. 193: tubal ectopic pregnancy. Obstet Gynaecol. 2018;131:e91-103.
- [Google Scholar]
- Double versus single dose methotrexate regimens in management of undisturbed ectopic pregnancy. Obstet Gynecol Int J. 2016;5:00184.
- [Google Scholar]
- Single-dose versus two-dose administration of methotrexate for the treatment of ectopic pregnancy: a randomized controlled trial. Hum Reprod. 2016;31:332-8.
- [Google Scholar]
- Multiple-dose and double-dose versus single-dose administration of methotrexate for the treatment of ectopic pregnancy: a systematic review and meta-analysis. Reprod Biomed Online. 2017;34:383-91.
- [Google Scholar]
- Comparison of single-dose and two-dose methotrexate protocols for the treatment of unruptured ectopic pregnancy. J Obstet Gynecol. 2011;31:330-4.
- [Google Scholar]
- Two cases of malignancy-associated hypercalcemia treated with mithramycin. Japanese Journal of Clinical Oncology. 1982;12(2):277-84.
- [Google Scholar]
- Use of “2-dose” regimen of methotrexate to treat ectopic pregnancy. Fertility and sterility. 2007;87(2):250-6.
- [Google Scholar]
- Medical management of ectopic pregnancy with single-dose and 2-dose methotrexate protocols: human chorionic gonadotropin trends and patient outcomes. Am J Obstet Gynecol. 2016;215:590.e1-5.
- [Google Scholar]
- Comparison of two different protocols of methotrexate therapy in medical management of ectopic pregnancy. Iran Red Crescent Med J. 2015;17:e20147.
- [Google Scholar]
- Comparison of double- and single-dose methotrexate protocols for treatment of ectopic pregnancy. Int J Gynecol Obstet. 2012;116:67-71.
- [Google Scholar]
- Predictors of success of a single-dose methotrexate in the treatment of ectopic pregnancy. J Obstet Gynecol India. 2016;66:233-8.
- [Google Scholar]







