Translate this page into:
Preovulatory normal saline pertubation prior to intrauterine insemination increases conception rate in unexplained infertility
Address for correspondence: Dr. Sudha Prasad, Bungalow No. 02, New Moti Bagh, Shanti Path, New Delhi - 110 021, India. E-mail: drsprasad@yahoo.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Context:
Intrauterine insemination (IUI) is widely used for fertility management for unexplained infertility (UI). Washed sperm are placed into uterine cavity to achieve pregnancy. The success rate of IUI with combined ovulation induction is always debated.
Aims:
The aim of the study is to analyze the effect of preovulatory pertubation with lignocaine, normal saline versus no-pertubation on conception rate during IUI cycle in women with UI.
Settings and Design:
A prospective, randomized controlled trial was conducted at University hospital tertiary referral center.
Subjects and Methods:
Of 464 women with UI, 320 women who fulfilled inclusion criteria were enrolled in the study. Ovulation induction was started with appropriate protocol. Women underwent transvaginal sonography till they achieved 2–3 dominant follicles of size ≥17–18 mm and endometrial thickness of ≥7 mm. Randomization was done by chit-pull system into three groups. Pertubation was carried out with low dose lignocaine or normal saline after 12–14 h of human chorionic gonadotropin administration. Pertubation groups were compared with no-pertubation IUI group.
Statistical Analysis:
Data were compared with unpaired Student’s t-test and Chi-square test appropriately.
Results:
Conception rate was 7.4% in lignocaine group, 20.7% in normal saline group, and 10.3% in control group.
Conclusions:
Pertubation with normal saline was associated with significant increase in IUI conceptions and live births as compared to no-pertubation group. Lignocaine pertubation was associated with the lowest conception rates but outcomes were not significantly different from the control. Hence, preovulatory saline pertubation prior to IUI is recommended to improve pregnancy rates in UI.
Keywords
Intrauterine insemination
ovulation induction
pertubation
pregnancy
unexplained infertility
INTRODUCTION
Unexplained infertility (UI) is the diagnosis if standard fertility investigations are normal and couples are not conceiving.[1] In vitro fertilization (IVF) is invasive and intricate.[2] Intrauterine insemination (IUI) is recommended for women with UI. Pregnancy rates vary between 10% and 20%, depending upon various factors.[3,4,5,6]
Tubal flushing/pertubation may increase chances of conception in infertile couples.[7] Hysterosalpingo-contrast-sonography with pertubation and hysterosalpingography (HSG) with oil-based medium reduce sperm phagocytosis. Tubal flushing with lipiodol showed ∼30% pregnancy rate as it decreases, inhibits sperm phagocytosis, and opens loose adhesions.[8,9,10,11,12,13,14]
The present study was conducted to evaluate the effect of lignocaine and normal saline pertubation during IUI cycles in UI.
SUBJECTS AND METHODS
This prospective, randomized controlled single-blinded trial was conducted from October 2010 to February 2012. Patients were recruited from fertility and assisted reproductive technology clinic after obtaining ethical clearance from the Institutional Ethics Committee of College and Associated Hospitals. This protocol was submitted to register under the Clinical Trial Registry-India (CTRI: Website URL http://ctri.nic.in). The reference number (REF/2015/04/008842) has been obtained. At present, registration of the study is under process.
A sample size of 320 women was calculated on the basis of 15% prevalence of infertility, 30% prevalence of UI, 95% confidence interval (95% CI), and 5% error to conduct the study.[15] Women in age group of 20–38 years with UI and normal body mass index (BMI) (19–24 kg/m2) were included in the study. Couples with ovulatory cycles, patent tubes, and normal semen analysis who had not conceived for 2 years after regular unprotected vaginal intercourse were considered to have UI. Women with moderate to severe endometriosis, uterine anomalies, or any other systemic disorder or obvious endocrinal disorder were excluded from the study. During the recruitment process, a total of 1716 women were screened, of which 464 (27.02%) were found to have UI. These 464 women with UI were further screened and 351 women fulfilled inclusion criteria as mentioned earlier.
An informed written consent was taken from all women. They subsequently underwent detailed evaluation, which included clinical history, complete physical examination, and routine subfertility investigations including semen analysis and culture and sensitivity test.[16] Any curable pathology was treated prior to starting the ovulation induction. All the women had premenstrual endometrial biopsy to rule out genital tuberculosis (TB) by histopathological examination, polymerase chain reaction for TB, and acid fast bacilli staining and culture prior to recruitment. Tubal status was confirmed by HSG/diagnostic laparoscopy and chromopertubation. Endocrinal evaluation was performed on day 2/3 of menstrual cycle. Basal follicle-stimulating hormone, luteinizing hormone, thyroid-stimulating hormone, and prolactin levels were estimated in all participants.
Women were called on day 2/3 of menstrual cycle, and transvaginal sonography (TVS) was performed to assess antral follicle count and endometrial thickness (ET). Accordingly, ovulation induction was started with appropriate protocol. All women were followed repeatedly by TVS till they achieved 1–2 dominant follicle of size ≥17–18 mm in diameter and ET of ≥7 mm. Human chorionic gonadotropin (hCG) 10,000 IU (Fertigyn, Sun Pharmaceuticals Industries Private Limited, Mumbai, Maharashtra, India) was administered to achieve final follicular maturation.
Of 351 women, a total of 11 women, who were not able to complete investigations or were lost to follow-up during ovulation induction, dropped from the study. The remaining 340 women completed the study. These 340 women were randomized into three groups as lignocaine pertubation group (Group A; n = 108 women), normal saline pertubation (Group B; n = 116 women), and no-pertubation group (Group C; n = 108 women). Randomization was achieved by chit-pull method.
Pharmacological 0.5 mL of lignocaine hydrochloride solution was taken from 1.0 mL ampoule (Injection, Lignocaine 2% w/v, 20 mg/mL, Laborate, India) and diluted in 99.5 mL normal saline to achieve 0.1 mg/mL concentration of lignocaine hydrochloride, which was used in women in Group A. Clinically applicable fresh lignocaine solution was prepared in IUI laboratory, exclusively on the day of pertubation for women in Group A. Pertubation procedures were performed in the single-blinded manner. All women of Group A and Group B were called 12–14 h after hCG injection. Pertubation was carried out with the help of Cook’s insemination catheter (Shepard Intrauterine Insemination Set; 5.4 Fr/20 cm; J-IUI-E-542009; G16465). A 10 mL syringe was connected to catheter and filled with lignocaine solution for women in Group A, and with normal saline for women in Group B whereas women in Group C had no-pertubation and served as control group. TVS was performed to assess ovulation 36 h following hCG trigger. The husband’s semen was analyzed and prepared either by swim-up or density gradient methods. IUI procedure was carried out with 0.3–0.5 mL of prepared (postwash) sperm sample by Cook insemination catheter (Shepard Intrauterine Insemination set; 5.4 Fr/20 cm; J-IUI-E-542009; G16465).
Luteal support was provided as vaginal pessaries of micronized progesterone (Naturogest, Zydus Healthcare, India) 200 mg twice daily along with 5.0 mg tablet of folic acid (Folvite, Wyeth, India) once a day for next 14 days. The women were called after 2 weeks for urine pregnancy test and estimation of serum βhCG levels.
Conception rates were estimated as the number of βhCG positives divided by the number of IUI cycles irrespective of outcome. Further confirmation of viable pregnancy was achieved by performing TVS at 6–8 weeks for fetal cardiac activity. Outcome data were used to estimate the clinical pregnancy rates. Unpaired Student’s t-test and Chi-square test were applied as appropriate to compare the parameters among three groups. P < 0.05 was considered statistically significant.
The study design is presented as a Figure 1 which is given as follows:

- Flowchart of study showing participants as per consort diagram
RESULTS
Of 340 recruited women, 108 (31.8%) were randomized to pertubation with low-dose balanced solution (0.1 mg/mL) of lignocaine (Group A), 116 (34.1%) to normal saline pertubation (Group B), and 116 (34.1%) women to no-pertubation (Group C) groups. Women underwent IUI cycles without pertubation (Group C) was served as control and compared with other two groups.
Demographic profile and cycle characteristics were compared, and no significant differences were found among three groups. Mean age of women in Group A was 29.04 ± 4.15 years, in Group B was 28.93 ± 4.07, and in Group C was 28.90 ± 4.23 years (P = 0.453). In addition, no significant difference in BMI was observed when compared among groups. It was 22.58 kg/m2, 23.00 kg/m2, and 22.84 kg/m2 in Group A, Group B, and Group C, respectively. Mean duration of infertility was also not statistically significant among them (data not given). No significant differences in mean number of follicles and ET on day of trigger were found among Group A, Group B, and Group C. Mean number of dominant follicles (>17 mm) was 1.56 ± 0.80 mm in Group A, 1.52 ± 0.68 mm in Group B, and 1.72 ± 0.84 mm in Group C (P = 0.200) whereas the ET was 8.27 mm, 8.41 mm, and 8.86 mm in Group A, Group B, and Group C, respectively (P = 0.229). There were no significant differences in postwash counts of motile spermatozoa among three groups. The postwash total count of motile spermatozoa in Group A was 67.30 million/mL, in Group B was 70.72 million/mL, and in Group C was 66.45 million/mL (P = 0.992) as shown in Table 1.

The conception rates among three groups were compared. It was 7.4% (8/108) in Group A, 20.7% (24/116) in Group B, and 10.3% (12/116) in Group C. The differences in conception rate among them were not statistically significant (P = 0.293) although an apparent increase in conception rate was noted in Group B (normal saline pertubation group) as shown in Table 2. Clinical pregnancy rates were also compared to observe the statistical significant differences among them.

The clinical pregnancy rate was 7.4% (8/108) in Group A (lignocaine pertubation), 14.2% (16/112) in Group B (normal saline pertubation), and 6.9% (8/116) in Group C (no pertubation) as shown in Table 2.
All eight (08/108; 7.4%) women in lignocaine pertubation group (Group A) were reached up to term pregnancy. In normal saline pertubation group (Group B), one (01/116; 0.8%) patient had a missed abortion after 8 weeks of gestation, one (01/116; 0.8%) patient had ectopic conception which was conservatively managed, and two patients (02/116; 1.7%) had biochemical pregnancy; however, unfortunately, one (01/116; 0.8%) patient was lost to follow-up after pregnancy test. A total of twenty (20/116; 17.2%) women with viable intrauterine pregnancies were ended with successful deliveries. In no-pertubation group (Group C), one (01/116; 0.8%) patient had a missed abortion, one (01/116; 0.8%) patient had ectopic conception which was also conservatively managed, and one (01/116; 0.8%) had biochemical pregnancy whereas the remaining nine (09/116; 7.7%) women with viable intrauterine pregnancies were successfully delivered. There were no multiple gestations in any group as shown in Table 2.
Conception rate in pertubation groups (both Group A and Group B, who received pertubation either with lignocaine or with normal saline) was combined together and further compared with no-pertubation group (Group C). No significant difference in conception rate between pertubation groups and no-pertubation groups was observed [14.28% (28/224) vs. 10.34% (12/116), respectively (P = 0.863)] as shown in Table 3.

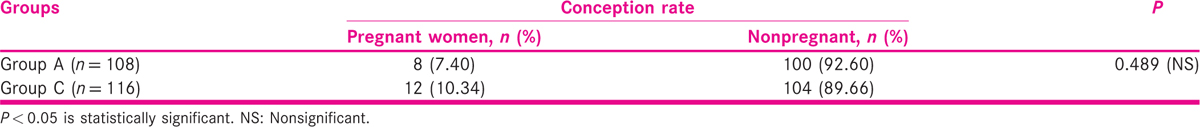
Group comparisons between interventional (pertubation groups) and control (no-pertubation group) groups, such as Group A versus Group B, Group A versus Group C, and Group C versus Group A, were also evaluated by means of two by two tables. The comparison was made between Group A and Group C, and conception rate in Group C was found higher as compared to Group A but was not statistically significant (7.4% vs. 10.34%; P = 0.489) as shown in Table 4. Similarly, women in Group B were compared to women in Group C, to assess impact of normal saline pertubation over no prior pertubation in IUI cycles. The conception rate was 20.7% in normal saline pertubation group (Group B) as compared to 10.3% in the control (Group C). There was apparent increase and statistically significant difference was observed in conception rate in normal saline pertubation group as compared to the control (P = 0.045) as shown in Table 5. Likewise, conception rate of Groups A and B was also compared to assess influence of lignocaine pertubation and normal saline pertubation. Normal saline pertubation group was found to have higher conception rate than lignocaine pertubation group, and this difference was statistically highly significant (P = 0.004) as shown in Table 6.


The conception and live birth rates in saline pertubation group were significantly higher than lignocaine and control groups. No significant difference was observed between outcomes of lignocaine versus control group.
DISCUSSION
The present study is focused on evaluating adjuvant effect of tubal flushing/pertubation on pregnancy rates in IUI cycles in women diagnosed with UI. Outcomes of this study were evaluated with the findings of similar trials performed by different investigators. The present study showed highest IUI success rate in normal saline pertubation group, i.e., 20.7% followed by 10.3% in no-pertubation group whereas the lowest was found in women who had lignocaine pertubation prior to their IUI, i.e., 7.4%. The saline pertubation group showed significantly better pregnancy and live birth rates compared to the control group and lignocaine pertubation group.
Edelstam et al.[1] observed statistically significant difference (P = 0.044) in clinical pregnancies in the lignocaine pertubation (18.9%) when compared to the group of women underwent IUI without pertubation (4.1%). On the other hand, our study showed significantly better conception rates in saline pertubation group when compared to lignocaine and control groups. Lignocaine pertubation followed by IUI yielded the lowest pregnancy rate (7.2%). However, the conception rate was not significantly different than control group.
Aboulghar et al.[6] showed pregnancy rates of 12.6% and 8.2% in hydrotubation and nonhydrotubation groups, respectively. This study recommended the benefit of hydrotubation over no-pertubation although results did not show any statistically significant difference in outcome between the two groups (odds ratio [OR] = 1.66; 95% CI = 0.62–4.63).
Pertubation with water-soluble contrast medium versus no pertubation was compared by Lindborg et al.[17] They found very high conception rate as well as live birth rate, not only in pertubation group of women but also in no-pertubation group of women. The pregnancy rate was 29.2% in pertubation group and 26.5% in the no-pertubation group, the difference being 2.7% (P = 0.63). The live birth rates were 22.6% and 20.5%. However, clinical impression of adding the pertubation could not be confirmed in this study.[17]
The effect of pertubation with oil-soluble contrast or water-soluble contrast media was also evaluated in 12 trials involving 2079 participants.[18] Pertubation with oil-soluble contrast media versus no intervention (no-pertubation) was found associated with a significant increase in pregnancy (OR = 3.30, 95% CI = 2.0–5.43) and of live birth (OR = 2.98, 95% CI = 1.40–6.37) rates.
Morad and Abdelhamid[19] observed that hydrotubation with Lignocaine had higher clinical pregnancy rates in UI when compared with saline group, but there was no significant difference (17.43% vs. 11.2%, respectively; P = 0.193).
The contrasting observation and recommendations are present in literature. Owing to the controversial findings and conflicting suggestions from different group of investigators in relation to application of prior Pertubation with lignocaine and/or with saline for its routine use in all IUI cycles needs more randomized controlled trials with larger population.
The results of the present study are comparable to the findings of Edelstam et al.,[1] Lindborg et al.,[17] Johnson et al.,[18] and Morad and Abdelhamid.[19] Thus, the body of evidence supporting the benefit of tubal pertubation for UI is growing. The authors would like to propose that multicentric, randomized controlled trials having larger sample size to evaluate the benefit of saline pertubation in IUI cycles for UI should be conducted so that definitive guidelines may be formed.
CONCLUSION
Pertubation with normal saline improves fertility outcome in infertile women with UI who are undergoing ovulation induction and IUI procedure. Higher conception rate was observed in women who had normal saline pertubation prior to IUI although multicentric trials with large number of patients are required to further support this hypothesis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
The authors deeply acknowledge the patients for providing their consent to conduct the study. Technical assistance form the staff of IVF and Reproductive Biology Centre is also extremely acknowledged.
REFERENCES
- Pertubation with lignocaine – A possible new treatment for women with endometriosis and impaired fertility. Ups J Med Sci. 2001;106:51-7.
- [Google Scholar]
- Predictive factors for pregnancy after intrauterine insemination (IUI): An analysis of 1038 cycles and a review of the literature. Fertil Steril. 2010;93:79-88.
- [Google Scholar]
- Efficacy of superovulation and intrauterine insemination in the treatment of infertility. National Cooperative Reproductive Medicine Network. N Engl J Med. 1999;340:177-83.
- [Google Scholar]
- Further considerations on natural or mild hyperstimulation cycles for intrauterine insemination treatment: Effects on pregnancy and multiple pregnancy rates. Hum Reprod. 2005;20:3141-6.
- [Google Scholar]
- Superovulation combined with insemination or timed intercourse in the treatment of couples with unexplained infertility and minimal or mild endometriosis. Acta Obstet Gynecol Scand. 1997;76:550-4.
- [Google Scholar]
- Controlled ovarian hyperstimulation and intrauterine insemination for treatment of unexplained infertility should be limited to a maximum of three trials. Fertil Steril. 2001;75:88-91.
- [Google Scholar]
- Therapeutic effect of hysterosalpingography: Oil- versus water-soluble contrast media − A randomized prospective study. Radiology. 1991;179:75-8.
- [Google Scholar]
- Morphology of in vitro sperm phagocytosis by rat peritoneal macrophages under influence of oily contrast medium (Lipiodol) Acta Eur Fertil. 1994;25:203-6.
- [Google Scholar]
- A randomized controlled trial of tubal flushing with lipiodol for unexplained infertility. Fertil Steril. 2002;77:173-5.
- [Google Scholar]
- Pulmonary and cerebral oil embolism after hysterosalpingography with oil soluble contrast medium. Respirology. 2004;9:134-6.
- [Google Scholar]
- Toxicological assessment of lidocaine in the pregnant rat. J Dent Res. 1985;64:1214-7.
- [Google Scholar]
- A new rapid and effective method for treatment of unexplained infertility. Hum Reprod. 2008;23:852-6.
- [Google Scholar]
- World Health Organization reference values for human semen characteristics. Hum Reprod Update. 2010;16:231-45.
- [Google Scholar]
- Adequacy of Sample Size in Health Studies. Chichester: John Wiley & Sons Ltd.; 1990.
- WHO Laboratory Manual for the Examination and Processing of Human Semen (5th). Geneva: WHO Press; 2010.
- Influence of HyCoSy on spontaneous pregnancy: A randomized controlled trial. Hum Reprod. 2009;24:1075-9.
- [Google Scholar]
- Prospective randomized study for hydrotubation with or without lidocaine before intrauterine insemination in unexplained infertility. Middle East Fertil Soc J. 2012;17:250-5.
- [Google Scholar]







