Translate this page into:
The predictive value of endometrial thickness for assessing neonatal birth weight in ART
Address for correspondence: Dr Sudha Prasad, Matritava Advanced IVF & Training Centre, 29, Paschimi Marg, Vasant Vihar, New Delhi-110057, India. E-mail: drsprasad@yahoo.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Neonatal birth weight is lower after assisted reproductive technology (ART) conception compared with natural conception. The aim of this retrospective study was to evaluate the predictive potential of measuring maternal endometrial thickness (ET) in women undergoing ART for assessing neonatal birth weight.
Methods:
and Results</ST> The patients (n = 100) were screened for meeting inclusion criteria with primary or secondary infertility and who underwent In-vitro Fertilization/Intracytoplasmic sperm injection (IVF/ICSI) or frozen embryo transfer (FET) cycles were enrolled in the study. All women received the antagonist protocol with recombinant gonadotropins/urinary gonadotropins or human menopausal gonadotropin as a stimulation protocol. Only singleton pregnancies were used in neonatal birth weight (n = 70) measurements. Retrospective data were collected for age, body mass index (BMI), and ET done by two-dimensional ultrasound that had successful pregnancy. The antenatal details, birth weight/gender of neonates were noted. A univariate regression analysis was performed between ET and neonatal birth weight in patients with live births (n = 70) to evaluate association between these parameters. The data were adjusted for variables such as age, BMI, and gestational duration. There was significant association of ET with neonatal birth weight and ET was observed to be a significant independent predictor for neonatal birth weight (slope 0.168, P = 0.0052).
Conclusion:
The present study suggests that ET measurement at the time of human chorionic gonadotropin (hCG) trigger in Indian women undergoing ART cycles can be a reliable independent predictor for assessing neonatal birth weight
Keywords
Endometrial thickness
infertility
IVF
neonatal birth weight
INTRODUCTION
A successful pregnancy has three major stages − fertilization, implantation, and embryo development. It has been observed that any complications in any stages may lead to infertility. Implantation plays a pivotal role in conception of fetus, which got impacted by following two major parameters: endometrial thickness (ET) and endometrial receptivity (ER). Further studies have shown that inadequate ET is one of the major causes of infertility in females. ER is clinically measured by an ER assay test, while ET can be measured by a simple transvaginal two-dimensional (2D) scan. ET is the most widely used prognostic factor for ER during assisted reproductive techniques (ART). Thus ET, if measured correctly on the day of human chorionic gonadotropin (hCG) triggering, can offer a reliable predictive value for live birth rates and neonatal birth weights. In view of recent studies, it has been observed that ET might be an important factor to have effect on placentation that may lead to complications such as placenta previa and low neonatal birth weight. A number of previous studies have shown that neonatal birth weight is lower after assisted reproductive technology (ART) conception compared with natural conception.[1,2,3,4] Furthermore, in case of ART conception, the risk for obstetrical complications and perinatal mortality is increased even in singleton pregnancies.[5,6,7] Very few studies have reported possible relationship between ET measurement and neonatal birth weights.[8,9,10]
A thin endometrial lining, in both fresh and frozen ET cycles, has been reported to correlate with lower ART success rates.[11,12,13,14,15] In another study, it was further reported increased ET was an independent risk factor for placenta previa, suggesting that the potential effect of ET may extend beyond implantation.[16] Few recent studies have studied the relationship of the above-mentioned endometrial variables with birth rates and neonatal birth weights. In a recently conducted single cohort ART cycles retrospective study,[1] an ET less than 7 mm was associated with a decrease in neonatal birth weight; however, it was not found to have predicted value for clinically defined low birth weight (LBW).
Most of the previous studies have been performed retrospectively and differ in ethnicities and other factors. While the recent studies have reported association of ET with neonatal birth weights, these differ in the degree of association and whether the birth weight is clinical LBW category or not. Also, other factors such as infertility cause, treatment days, paternal body mass index (BMI), frozen embryo transfer (FET) preparation, and year of treatment can impact the birth weights after successful implantation. Clearly, more retrospective and prospective studies are required to ascertain the role of ET measurement on neonatal birth weights and live birth rates, especially in Indian women.
Therefore, we studied the significance of ET measurement in addition to endocrinology before implantation step during ART for assessing neonatal birth weights.
MATERIALS AND METHODS
Study design and patients
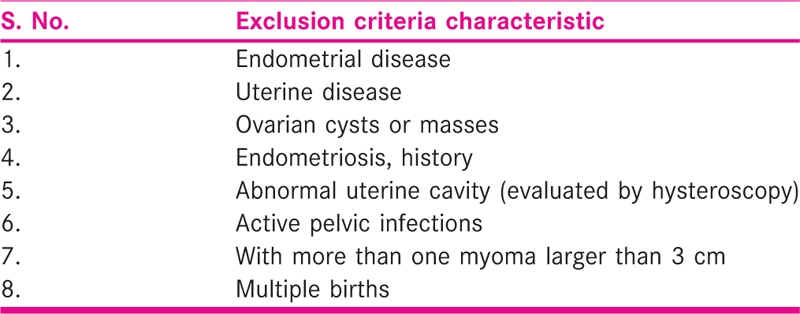
This retrospective study was conducted at Matritava Advanced IVF & Training Centre between February 2019 and February 2021. The study was approved by Independent Ethics Committee of Indian Fertility Society as per the letter (Ref F.I./IEC/IFS/2020 NO. 60) dated December 31, 2020. All patients (n = 100) aged 24 to 42 years with BMI less than 30 kg/m2 were screened for exclusion criteria [Table 1]. The patients with primary or secondary infertility recruited for In-vitro Fertilization/Intracytoplasmic sperm injection (IVF/ICSI) or FET cycles were enrolled in the study. Only singleton pregnancies were used in neonatal birth weight (n = 70) measurements.
Clinical protocol
Retrospective data was recruited for IVF/ICSI and FET cycles and data were collected for age, BMI, and ET done by 2D ultrasound that had successful pregnancy after IVF/ICSI or FET cycles. The antenatal details of the patients, birth weight of neonates, and obstetrics complications were noted.
All women received the antagonist protocol with recombinant gonadotropins/urinary gonadotropins or human menopausal gonadotropin as a stimulation protocol. Transvaginal ultrasound was done using Voluson S8 machine (GE Healthcare Austria) equipped with a 5 to 7.5 MHz transvaginal probe for folliculometry and ET was done every other day starting from the sixth day of the gonadotropin stimulation till achievement of hCG trigger criteria as our standard protocol.
At the day of hCG triggering, transvaginal ultrasound ET was measured in the longitudinal plane at the widest anteroposterior diameter with a transvaginal 2D ultrasound. All measurements were done three times by the same examiner and the mean of these measures was calculated.
Similarly, endometrium was prepared by oral estrogen (tab estradiol valerate 8–6 mg/day) therapy maximum of 12 to 14 days and ET was measured before starting progesterone in the same manner in FET cycles. Embryos were transferred at cleavage (D3) or blastocyst (D5) stage with partially filled bladder under guidance of transabdominal ultrasound. Luteal phase support was given in all women as per the standard protocol.
Parameters
The primary outcome variables measured in the study cohort are as follows:
Endometrial thickness: We consider the ET as the maximal anterior–posterior distance between both endometrial layers about 1 cm from the uterine fundus by ultrasonographic visualization.
Neonatal birth weight: Weight (in grams) of live born neonate beyond 28 weeks of gestational age measured at the time of birth.
Along with these, there are other variables to be considered for their potential to be confounders such as female age, BMI, and fresh or frozen embryo transfer.
Statistical analysis
A univariate regression analysis was performed between ET and neonatal birth weight in patients with live births (n = 70) to evaluate association between these parameters. The patient characteristics will be compared between fresh embryo transfer and frozen embryo transfer cycles by t-test or chi-square test as appropriate. A multiple regression analysis was also performed to provide the effect of all secondary variables (age, BMI, etc.) on predictive value of ET for neonatal birth weight. The primary goal of the statistical analysis was to determine whether ET or associated factors significantly and independently can predict the neonatal birth weight. Results are presented as regression slopes with corresponding standard errors and P values. All statistical analyses were performed by using GraphPad Prism software.
RESULTS
The overall demographic characteristics of the patients who met inclusion criteria (n = 70) such as age, BMI, cause of infertility are given in Table 2. The mean values or percentage of patients are shown for all cycles [Table 2].
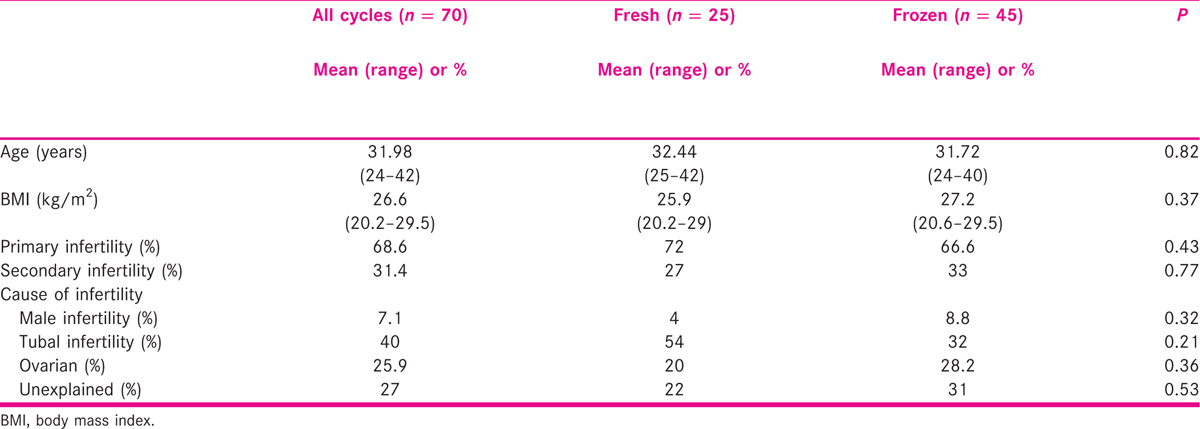
The patients were grouped into frozen or fresh embryo transfer cycles with comparable demographic characteristics. There were no significant differences in means of age, BMI, infertility type or causes between frozen or fresh embryo transfer cycles when analyzed with t-test or chi-square test as applicable [Table 2].
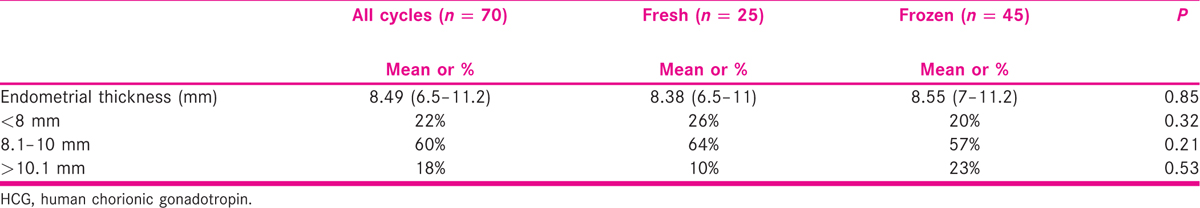
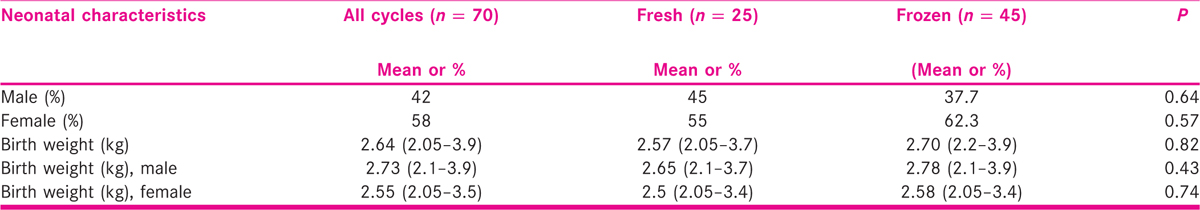
We observed no significant differences in ET [Table 3] or neonatal birth weights [Table 4] between fresh and frozen type cycles (P = 0.85). We also analyzed data for the predictive value of measuring ET for assessing the neonatal birth weight in all live births from our fresh and frozen cycles. The univariate linear regression test was applied, and we observed a significant association (slope 0.162, P = 0.004, unadjusted) of neonatal birth weight with ET [Figure 1, Table 5].
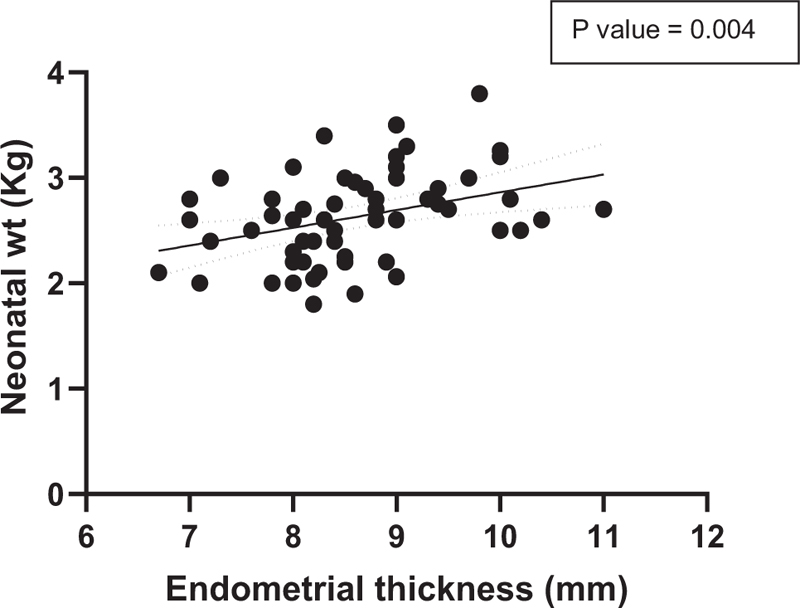
- The univariate regression curve showing association of neonatal birth weight with endometrial thickness for both genders of neonates (n = 70). The endometrial thickness was found to be a significant independent predictor (P = 0.004) for neonate birth weight (unadjusted) in all singleton pregnancies included in the study
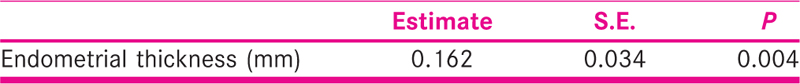
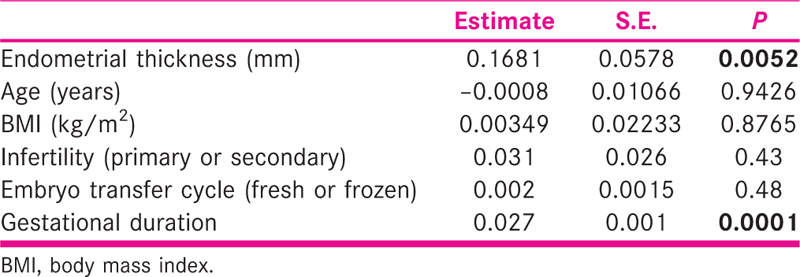
We also performed the multiple regression test for predictive value of ET for assessing neonate birth weight where other variables such as age, BMI, infertility diagnosis, embryo transfer cycle type, and gestational duration [Table 6] were also included in regression analysis as all these variables can affect birth weight. All variables passed the normality testing during analysis. After adjusting for these variables, the ET value still remained to be a significant independent predictor for neonatal birth weight (slope 0.168, P = 0.0052). The only other factor that was observed to be a significant predictor of birth weight was found to be gestational duration (slope 0.027, P = 0.0001) as expected [Table 3].
DISCUSSION
Some of the previous studies have reported an association between ET and neonatal birth weight in women undergoing ART.[8,9,10] While there appears to be a relation between these two factors, the degree of association varies.[11,12] Thus, the present study attempted to explore the predictive potential of ET for assessing neonatal birth weight in our cohort of Indian women undergoing ART cycles. We observed a strong association of ET values, measured at the day of hCG trigger during standard ART protocol, with the neonatal birth weight from singleton pregnancies (n = 70). The statistical analysis also revealed that there is a significant predictive value of ET as an independent predictor for assessing birth weight.
The contributing factors of LBW after ART procedure can be diverse, with little understanding on the main underlying causes. These causes that are thought to affect birth weight after ART can range from age, BMI, gestational duration to genetics or environmental factors.
The adjustment of regression with age, BMI, gestational duration, and neonatal gender also led to the predictive value of ET to be significant for assessing neonatal birth weight in our study cohort [Table 6]. Our study consisted of fresh cycle or frozen cycle embryo transfer, which may also be affecting fetal growth and thus birth weight; therefore, we adjusted the data for this variable also. However, there was no significant effect of this variable on birth weight assessment by ET. The gestational duration however was another independent predictor of neonate birth weight, which was expected as the shorter than normal gestational period is a well-known factor that leads to reduced neonatal birth weight. Previous studies have also clearly shown that assisted reproduction techniques are also associated with preterm birth that is associated with reduced birth weight.[10,11,12,13] The lower birth weight has long-term consequences for health of future adults.[14] Recently, a study found that ET was an independent predictor of neonatal birth weight in women undergoing ART with obstetric complications.[17] However, our study group was a diverse one that included women with and without obstetric complications, which make these observations even more important. The limitations of this study are the retrospective nature and the relatively small sample size (n = 70), which limited our ability to categorize patients into subgroups based on several variables including obstetric complications. Another limitation remains the unaccounted variables such as diet and other environmental factors. Even with these limitations, we were successfully able to test our hypothesis, the results of which are in line with previous reports.
In conclusion, our study suggests that ET measurement at the time of hCG trigger in Indian women undergoing ART cycles can be a reliable independent predictor for assessing neonatal birth weight and this aspect should be taken into consideration for making clinical decisions wherever required.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Comparative birth weights of singletons born after assisted reproduction and natural conception in previously infertile women. Hum Reprod. 2006;21:705-12.
- [Google Scholar]
- Impact of frozen-thawed single-blastocyst transfer on maternal and neonatal outcome: an analysis of 277,042 single-embryo transfer cycles from 2008 to 2010 in Japan. Fertil Steril. 2014;101:128-33.
- [Google Scholar]
- Infant outcome of 957 singletons born after frozen embryo replacement: the Danish National Cohort Study 1995–2006. Fertil Steril. 2010;94:1320-7.
- [Google Scholar]
- Factors affecting low birthweight after assisted reproduction technology: difference between transfer of fresh and cryopreserved embryos suggests an adverse effect of oocyte collection. Hum Reprod. 2008;23:1644-53.
- [Google Scholar]
- Smaller fetal size in singletons after infertility therapies: the influence of technology and the underlying infertility. Fertil Steril. 2011;96:1100-6.
- [Google Scholar]
- Perinatal outcome of singleton siblings born after assisted reproductive technology and spontaneous conception: Danish national sibling-cohort study. Fertil Steril. 2011;95:959-63.
- [Google Scholar]
- Comparative analysis of fetal and neonatal outcomes of pregnancies from fresh and cryopreserved/thawed oocytes in the same group of patients. Fertil Steril. 2013;100:396-401.
- [Google Scholar]
- Should we continue to measure endometrial thickness in modern-day medicine? The effect on live birth rates and birth weight. Reprod Biomed Online. 2018;36:416-26.
- [Google Scholar]
- Endometrial thickness and pregnancy rates after IVF: a systematic review and meta-analysis. Hum Reprod Update. 2014;20:530-41.
- [Google Scholar]
- Perinatal outcomes associated with assisted reproductive technology: the Massachusetts Outcomes Study of Assisted Reproductive Technologies (MOSART) Fertil Steril. 2015;103:888-95.
- [Google Scholar]
- Perinatal outcomes in singletons following in vitro fertilization: a metaanalysis. Obstet Gynecol. 2004;103:551-63.
- [Google Scholar]
- Obstetric and neonatal outcome after single embryo transfer. Hum Reprod. 2007;22:1073-9.
- [Google Scholar]
- Low and very low birth weight in infants conceived with use of assisted reproductive technology. N Engl J Med. 2002;346:731-7.
- [Google Scholar]
- Growth and chronic disease: findings in the Helsinki birth cohort. Ann Hum Biol. 2009;36:445-58.
- [Google Scholar]
- The impact of a thin endometrial lining on fresh and frozen-thaw IVF outcomes: an analysis of over 40 000 embryo transfers. Hum Reprod. 2018;33:1883-8.
- [Google Scholar]
- Risk of placenta praevia is linked to endometrial thickness in a retrospective cohort study of 4537 singleton assisted reproduction technology births. Hum Reprod. 2014;29:2787-93.
- [Google Scholar]
- Endometrial thickness influences neonatal birth weight in pregnancies with obstetric complications achieved after fresh IVF–ICSI cycles. Arch Gynecol Obstet. 2017;296:115-22.
- [Google Scholar]







