Translate this page into:
To Assess the Impact of Smoking on Semen Quality: A Comprehensive Study of Semen Parameters in North Indian Men

*Corresponding author: Pooja Gupta, M.S, Matritava Advanced IVF and Maternity Centre, Gurugram, Haryana, India dr.poojagupta23@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gupta P, Prasad S, Prasad S. To Assess the Impact of Smoking on Semen Quality: A Comprehensive Study of Sperm Parameters in North Indian Men. Fertil Sci Res. 2024;11:16. doi: 10.25259/FSR_28_2024
Abstract
Objectives
Infertility affects a large proportion of couples worldwide, with male factors accounting for approximately half of the cases. Smoking and other lifestyle choices have been linked to decreased sperm quality, which includes factors such as sperm count, motility, and morphology. This study intends to assess the influence of smoking on sperm quality among north Indian males seeking reproductive treatment.
Material and Methods
A cross-sectional study was conducted at Matritava Advanced IVF and Maternity Centre in Gurugram, Haryana, India, from September 2023 to June 2024. The study comprised 100 men aged 21–55 years old who were coming for infertility treatment and inclined to participate in the study and were divided into two groups: smokers (n = 50) and non-smokers (n = 50). Semen samples were analysed according to WHO guidelines (2021) to evaluate parameters such as semen volume, sperm concentration, total sperm count, motility, and morphology. Statistical analysis was performed using SPSS software version 25.0.
Results
The average age of smokers and non-smokers was 35.10 ± 4.41 years and 35.72 ± 3.80 years, respectively (p = 0.45). Smokers showed more abnormalities in semen parameters compared to non-smokers. Key findings include semen volume of (2.86 ± 1.04 ml) in smokers as compared to non-smokers (2.40 ± 0.67 ml) (p = 0.01). Smokers exhibited lower average sperm concentration (51.91 ± 37.81 million/ml) than non-smokers (67.14 ± 56.76 million/ml) (p = 0.07). Smoking significantly reduced sperm morphology (2.70 ± 0.81%) compared to non-smokers (3.50 ± 0.76%) (p < 0.001). There were no significant differences between total and progressive motility between the two groups.
Conclusion
Smoking has a considerable negative impact on sperm quality, particularly morphology, in males seeking fertility treatment. These findings emphasise the necessity to incorporate smoking cessation 3 months before Starting the fertility treatment to improve reproductive outcomes. Healthcare organisations should emphasise the negative effects of smoking on male fertility and advocate lifestyle modifications as part of comprehensive fertility care.
Keywords
Smoking
Semen Quality
Sperm Parameters
Male Infertility
North India
Fertility Treatment
Smoking Cessation
INTRODUCTION
Infertility affects 8–12% of couples worldwide, with male infertility accounting for 40–50% of cases. In India, the cultural emphasis on childbearing increases the pressure and stigma associated with infertility.[1]
Despite being a well-known global health risk, smoking is still glamorised, notably in India, the world’s second-largest tobacco consumer. Infertility is becoming more common in India, and smoking is a major risk factor. Approximately 266.8 million Indians currently smoke tobacco in various forms, making India the industry’s second-largest tobacco consumer, with a prevalence among men aged 25–44 years of 21.9%.[2]
There has been a tremendous global reduction in sperm quality, which has been related to factors related to lifestyle, such as smoking. Smoking lowers sperm count, motility, and morphology due to the harmful effects of nicotine and polycyclic aromatic hydrocarbons found in cigarette smoke. These chemicals can cause oxidative stress and DNA damage and impair spermatogenesis.[3] Smoking has both direct and indirect effects on male fertility, as evidenced by hormonal changes. Smoking reduces testosterone levels, causes inflammation, and has negative effects on reproductive tissues.[1]
The purpose of this study is to assess the effect of smoking on semen quality among North Indian men seeking fertility treatment by analysing semen parameters between smokers and non-smokers and finding specific abnormalities.
Aims and Objectives
To compare the prevalence of abnormal sperm parameters in smokers and non-smokers groups of North Indian males.
To compare sperm concentration, sperm count, motility, and morphology in both groups.
MATERIAL AND METHODS
Study Design and Setting
This cross-sectional study was carried out between September 2023 and June 2024 at the Matritava Advanced IVF and Maternity Centre in Gurugram, Haryana, India. The study aimed to determine the impact of smoking on semen parameters in men seeking reproductive treatment.
Study Population
The study included 100 men aged 21–55 who visited the Matritava clinic to seek fertility treatment. The participants were split into two groups: smokers (n = 50) and non-smokers (n = 50). Smokers included those who smoked <5 cigarettes per day (mild smokers) for the previous year, whereas non-smokers were those who had never smoked or had stopped smoking for more than a year.[4]
Inclusion Criteria
Age ranges from 21 to 55 years.
All men visit clinics to seek fertility treatment.
Exclusion Criteria
History of consumption of gonadotoxic medicines.
History of sexually transmitted infections.
History of chronic medical disorders (such as diabetes or high blood pressure).
History of reproductive system problems (e.g., varicocele, cryptorchidism).
History of exposure to occupational or environmental contaminants.
Non-willing males to participate in the study
Data Collection
Smoking History
After taking the detailed written consent, a standardised questionnaire was used to collect the complete smoking history, including questions regarding smoking duration, intensity, and frequency.
Semen Analysis
Semen samples were collected through masturbation following 2–7 days of sexual abstinence. Samples were examined within 1 h of receiving a semen sample, according to World Health Organisation (WHO) guidelines (2021).[5] Semen volume, sperm concentration, total sperm count number, sperm motility (innovative, non-innovative, and immotility), and sperm morphology were assessed. Abnormal parameters were referred to as oligospermia, asthenozoospermia, teratozoospermia as definition, or a combination of the two.
Statistical Analysis
The data were examined with SPSS software model 25.0. To describe the facts, descriptive statistics were employed. Continuous variables were expressed as mean ± SD, while categorical variables were expressed as percentages.
The independent t-test for constant variables and the chi-square test for categorical variables were used to compare smokers to non-smokers. A p-value of less than 0.05 is considered statistically significant.
RESULTS
Result 1
Age of the Study Population
The mean age of smokers was 35.10 ± 4.41 years, while the mean age of nonsmokers was 35.72 ± 3.80 years. The difference in mean age between the two groups was not statistically significant (p = 0.45) [Table 1, Figure 1].
| Smoker (n = 50) | Non-smoker (n = 50) | p-value | |
|---|---|---|---|
| Mean age in years | 35.10 ± 4.41 | 35.72 ± 3.80 | 0.45 |
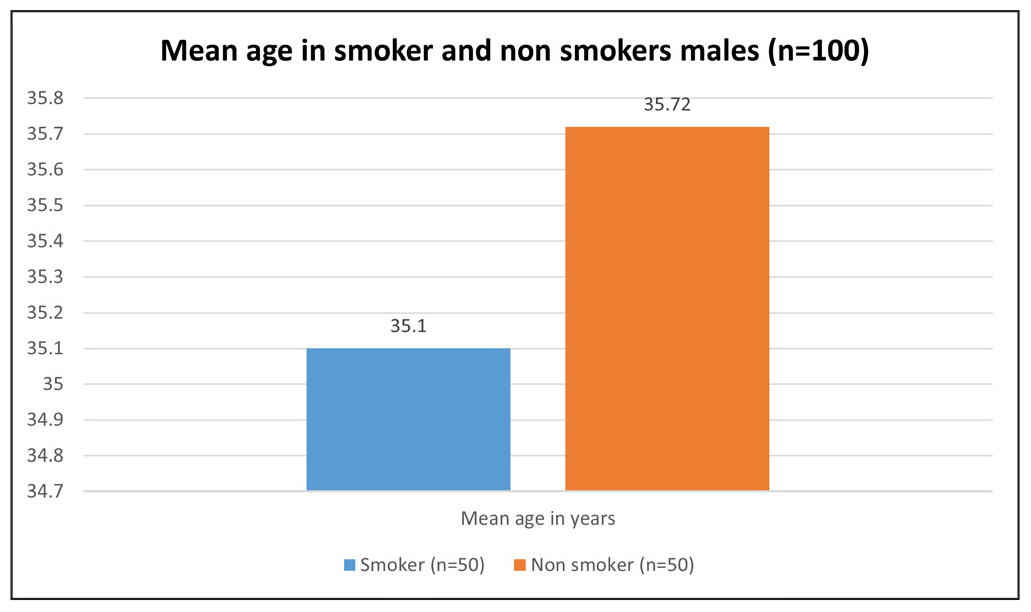
- Represents mean age in smoker and non-smokers males.
Result 2
Semen Analysis Results in Smoker and Non-Smokers Males (n = 100)
The semen analysis results showed varying abnormalities in semen quality between smokers and nonsmokers. A significant difference was found in teratozoospermia in both groups [Table 2, Figure 2].
| Semen analysis | Smoker (n = 50) | Non-smoker (n = 50) |
| Asthenoteratozoospermia | 9 (18.0%) | 4 (8.0%) |
| Mild oligozoospermia | 1 (2.0%) | 0 (0.0%) |
| Normozoospermia | 4(8.0%) | 24 (48.0%) |
| Normozoospermia with hypospermia | 0 (0.0%) | 1 (2.0%) |
| Oligoasthenoteratozoospermia | 1 (2.0%) | 0 (0.0%) |
| Oligoasthenoteratozoospermia | 6 (12.0%) | 3 (6.0%) |
| Oligoasthenoteratozoospermia with hypospermia | 2 (4.0%) | 0 (0.0%) |
| Oligoasthenozoospermia | 0 (0.0%) | 4 (8.0%) |
| Oligoteratozoospermia | 1 (2.0%) | 4 (8.0%) |
| Oligozoospermia | 3 (6.0%) | 2 (4.0%) |
| Severe Oligoteratozoospermia | 0 (0.0%) | 1 (2.0%) |
| Teratozoospermia | 23 (46.0%) | 5 (10.0%) |
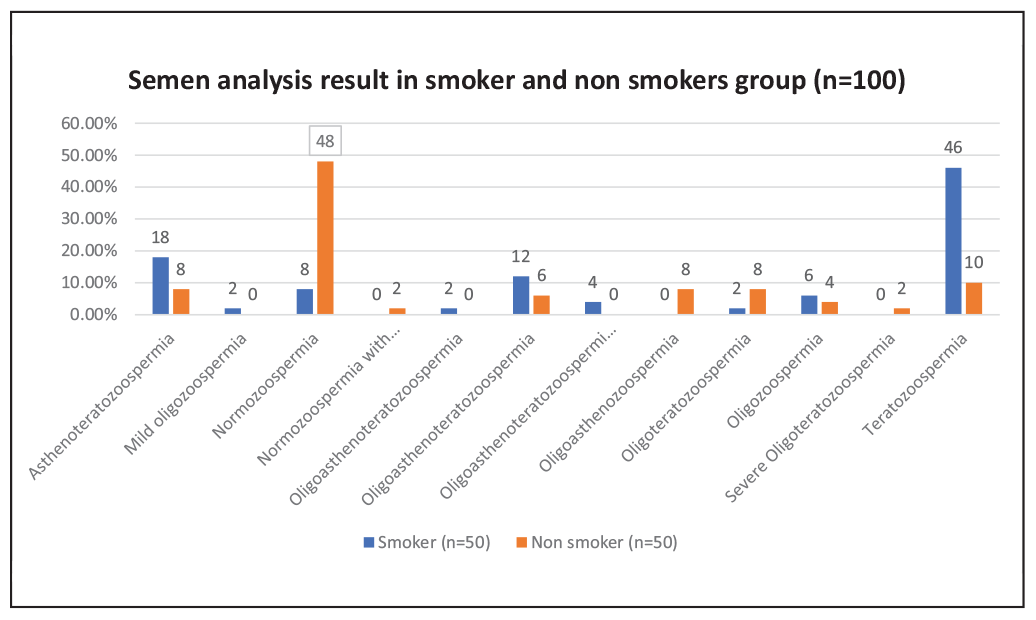
- Represents the semen analysis result in the smoker and non-smokers group.
Result 3
Semen Parameters in Smoker and Non-Smoker Group
The analysis of semen parameters showed that smokers had lower mean total sperm concentration and count (p = 0.07) (p = 0.42). Smokers showed no significant differences in total motility, progressive motility, or non-progressive motility compared to non-smokers. However, it has been observed that a slightly higher percentage of immotile sperm were in the smokers’ group than in non-smokers, with no significant difference (p = 0.41). Smokers had a significantly lower percentage of normal morphology (2.70 ± 0.81%) compared to non-smokers (3.50 ± 0.76%), with a p-value of <0.001 [Table 3, Figure 3].
| Semen parameters | Smoker (n = 50) | Non-smoker (n = 50) | p-value |
| Volume (ml) | 2.86 ± 1.04 | 2.40 ± 0.67 | 0.01 |
| Total Sperm Conc. (million/ml) | 51.91 ± 37.81 | 67.14 ± 56.76 | 0.07 |
| Total Sperm count (million/ejaculate) | 145.60 ± 123.69 | 157.69 ± 115.77 | 0.42 |
| Total Motility % | 49.78 ± 16.63 | 53.20 ± 15.26 | 0.40 |
| Progressive Motility % | 33.78 ± 12.22 | 37.92 ± 11.83 | 0.19 |
| NP Motility % | 15.56 ± 7.14 | 15.26 ± 5.68 | 0.80 |
| Immotile (©)% | 50.12 ± 16.73 | 46.80 ± 15.26 | 0.41 |
| Morphology % | 2.70 ± 0.81 | 3.50 ± 0.76 | <0.001 |
NP: Non-progressive, bold values means significant value – P value < 0.05 – significant < 0.01 – highly significant.
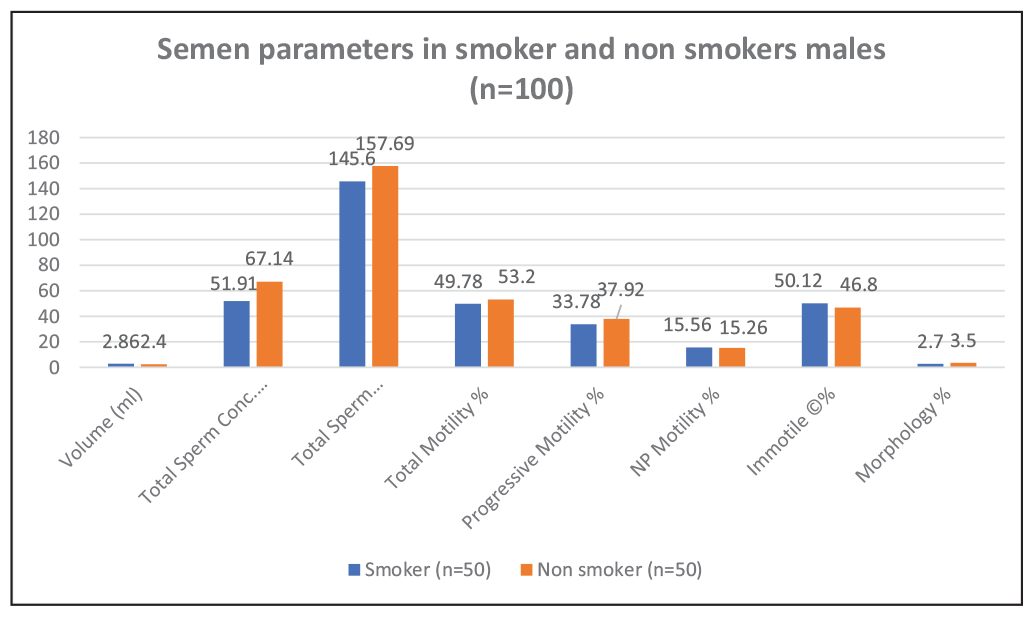
- Represents semen parameters in smoker and non-smokers group.
DISCUSSION
Smoking is one of the oldest and most widespread habits, having a significant impact on wellbeing globally and resulting in an estimated 3 million deaths each year.[2] Smoking has a greater negative impact on male reproductive fitness than alcohol or coffee. Cigarette smoke contains more than 7000 compounds, including carcinogens and mutagens, which can harm human germ cells, decrease sperm production, and cause hormonal imbalance.[6] The present study determines the impact of smoking on semen quality among North Indian men seeking fertility treatment.
In the present study, the average age of smokers was 35.10 ± 4.41 years, whereas non-smokers had an average age of 35.72 ± 3.80 years. There was no significant difference between the two groups (p = 0.45). The similarity in age distribution implies that the observed changes in sperm characteristics are most likely due to smoking rather than age-related variables.
Semen Analysis Results in Smokers and Non-Smokers
Our study found significant variations in semen parameters between smokers and non-smokers. Among smokers, 18% had asthenoteratozoospermia, compared to 8% of non-smokers. Mild Oligozoospermia develops in 2% of smokers but not in non-smokers. Normozoospermia was found in 8% of smokers and 48% of non-smokers. Oligoasthenoteratozoospermia was found in 18% of smokers and 6% of non-smokers, demonstrating that smoking has a significant impact on this situation. Oligozoospermia was observed in 6% of smokers and 4% of non-smokers. Finally, smokers had a much greater rate of teratozoospermia (46%) than non-smokers (10%). These data demonstrate that smoking has a negative impact on multiple semen parameters, especially on sperm count, motility, and morphology.
A systematic review and meta-analysis studied information from 15 studies with 12,503 participants, including smokers, non-smokers, drinkers, and non-alcoholics. The data revealed that smokers were significantly more likely to develop oligozoospermia, teratozoospermia, and asthenozoospermia than nonsmokers. These findings are consistent with our study results.[7]
A cross-sectional study of 1938 infertile males in China discovered that smoking is significantly linked with negative impacts on seminal parameters, such as decreased semen concentration and reduced sperm motility in infertile men. This finding is consistent with our present investigation findings. The findings of this cross-sectional study highlighted the need for smoking cessation programs as part of fertility treatment procedures to increase sperm quality and reproductive outcomes.[8]
A study conducted by Trummer and his colleagues discovered conflicting results, with our study revealing no significant variations in standard sperm parameters such as sperm awareness, motility, and morphology between smokers and non-smokers. People who smoke, on the other hand, have a wider spectrum of round cells and leukocytes in their sperm, which could contribute to infertility by producing reactive oxygen species.[9]
Semen Parameters
The detailed analysis of semen parameters further underscores the negative impact of smoking on semen quality.
Total Sperm Concentration
The present study found no statistically significant difference between smokers and non-smokers in terms of sperm concentration (51.91 ± 37.81 million/ml vs. 67.14 ± 56.76 million/ml) (p = 0.07). Similarly, a study conducted by Afsin et al. (2024) in Turkey found no significant difference in sperm attention between smokers and non-smokers, with an average sperm concentration of 30.0 million/ml in smokers and 27.0 million/ml in non-smokers. This study finding correlates with our study findings.[10,11]
Total Sperm Count
The present study found that smokers had a slightly lower mean overall sperm count (145.60 ± 123.59 million/ejaculate) than non-smokers (157.59 ± 115.77 million/ejaculate), but not significantly (p = 0.42). Similar findings have been discovered by other researchers, including a study by Osadchuk et al., who discovered a significantly lower total sperm count number in smokers, and Afsin et al., who found a median overall sperm count of 90 million in smokers and 78 million in non-smokers, with no significant difference. The present study’s findings are also consistent with Afsin et al. and Osadchuk et al. These findings suggested that smoking definitely affects overall sperm count.[10,11]
Motility
Total Motility
The current study found no significant difference in total motility, with mean total motility of 49.78 ± 16.63% in smokers and 53.20 ± 15.26% in non-smokers (p = 0.40). This finding is consistent with the study by Afsin et al. In contrast, Ramon et al. found an association between smoking with reduced total sperm motility. This suggests that smoking has adverse effects on sperm motility and may become significant with an increase in the number of cigarettes.[7,10]
Progressive Motility
Our study found no significant difference in mean progressive motility between smokers (33.78 ± 12.22%) and non-smokers (37.92 ± 11.83%) (p = 0.19). This study and Afsin et al. discovered no significant differences in progressive motility; however, Osadchuk et al. and Ramon et al. reported substantial reductions in smokers. This suggests that smoking level has a significant impact on sperm motility.[7,8,11]
Non-progressive Motility
There was no significant difference in non-innovative motility between smokers and non-smokers (15.56 ± 7.14% in smokers vs. 15.26 ± 5.68% in non-smokers, p = 0.8). This finding is consistent with the other studies, which found comparable results for non-progressive motility, demonstrating that smoking has no significant effect on this parameter.[7,10,11]
Morphology
The present study found that smokers had considerably significant morphological abnormalities in the sperm (2.70 ± 0.80%) compared to non-smokers (3.50 ± 0.76%) (p < 0.001). These findings were consistent with the studies by Osadchuk et al. and Ramon et al., but Afsin et al. and Trummer et al. failed to identify such statistically significant differences, implying that factors such as smoking intensity, duration, and population variations may vary the degree of damage. These findings highlight the necessity for targeted smoking cessation programs to promote male reproductive health and sperm quality.[7,9–11]
CONCLUSION
This study demonstrates that smoking even less than five cigarettes per day has a significant negative effect on numerous sperm features, particularly sperm morphology. The increased prevalence of teratozoospermia and other sperm abnormalities among smokers underscores the importance of targeted smoking cessation interventions as part of fertility treatment options. By providing specific insights into the effects of smoking on sperm, this study emphasises the importance of lifestyle modifications in improving reproductive outcomes for men seeking fertility treatment. The findings suggest that healthcare professionals should include smoking cessation counselling as an important component of reproductive therapy approaches.
Author contibution
SU.P: Research idea, Design of the study, PG: Acquisition of data for the study, Analysis of data for the study, PG, SU.P and SP: Interpretation of data for the study, PG, SU.P: Drafting the manuscript, PG, SU.P and SP: Revising it critically for important intellectual content and final approval of the version to be published.
Ethical approval
The ethical approval was taken before initiation of the study, reference number F.1/IEC/IFS/2022No.04.
Declaration of patient consent
Patient consent is not required as the patient’s identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using the AI.
REFERENCES
- Effect of Tobacco Use on Semen in Infertile Male. J Pharm Bioall Sci. 2024;16:S412-4.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Tobacco Addiction and Infertility in India: An overview. Int J Reprod Contracept Obstet Gynecol. 2023;12:2590-4.
- [Google Scholar]
- The Effects of Smoking & Alcohol Intake on Sperm Quality. Poonam Shodh Rachna J.. 2024;3((V)):PSR-2304052.
- [Google Scholar]
- Tobacco Smoking is Associated with Decreased Semen Quality. Rep Health. 2016;13:90.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- WHO Laboratory Manual for the Examination and Processing of Human Semen. (6th ed.). World Health Organization;
- [Google Scholar]
- Sperm Concentration and Semen Volume Increase After Smoking Cessation in Infertile Men. Int J Impot Res. 2022;34:614-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Effect of Tobacco Smoking and Alcohol Consumption on Semen Quality and Hormone Reproductive Levels in Infertile Males: A Systematic Review and Meta Analysis. Pharmacia. 2024;71:1–14.
- [Google Scholar]
- Associations Between Tobacco Inhalation and Semen Parameters in Men with Primary and Secondary Infertility: A Cross-Sectional Study. Front. Endocrinol. 2024;15:1396793.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The Impact of Cigarette Smoking on Human Semen Parameters and Hormones. Hum Rep. 2002;17((6)):1554-9.
- [CrossRef] [PubMed] [Google Scholar]
- A Single-Center Study Assessing the Relationship Between Smoking Habits and Sperm Parameters in Men with Suspected Infertility. Firat Med J. 2024;29((2)):68-73.
- [Google Scholar]
- Effects of Cigarette Smoking on Semen Quality, Reproductive Hormone Levels, Metabolic Profile, Zinc and Sperm DNA Fragmentation in Men: Results from a Population-Based Study. Front Endocrinol. 2023;14:1255304.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]







