Translate this page into:
Efficacy of Surgically Extracted Sperm in Assisted Reproductive Technology

*Corresponding author: Dr. Arzoo Chadha, Department of Obstetrics & Gynaecology, RISAA IVF, New Delhi, Green Park Main, New Delhi, Delhi, India. drarzoochadha@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Chadha A, Bakshi R. Efficacy of Surgically Extracted Sperm in Art. Fertil Sci Res. 2024;11:14. doi: 10.25259/FSR_14_2024
Abstract
Objectives
The objective of this study is to evaluate and compare the efficacy of various sperm extraction techniques used in Assisted Reproductive Technology (ART), focusing on sperm retrieval rates, fertilization rates, and clinical outcomes in patients undergoing fertility treatments.
Material and Methods
This retrospective observational study was conducted at RISAA IVF, Green Park, New Delhi, from January 2023 to January 2024. The study included male participants diagnosed with azoospermia, who underwent ART procedures such as in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI). Sperm extraction techniques evaluated include percutaneous epididymal sperm aspiration (PESA), testicular sperm aspiration (TESA), and microdissection testicular sperm extraction (micro-TESE). Data were collected from electronic medical records, laboratory reports, and patient charts, focusing on demographic data, sperm retrieval rates, and clinical outcomes. Statistical analysis was performed using SPSS software, with significance set at P < 0.05.
Results
Surgical sperm retrieval was performed on 11 azoospermic patients. Viable sperm was successfully retrieved using PESA in 18.1% of the patients, while TESA and micro-TESE yielded successful retrievals in 63.6% and 18.1% of the cases, respectively. The overall pregnancy rate achieved through these procedures was 63.6%. No significant difference in pregnancy rates was observed between the different sperm retrieval techniques (P > 0.05).
Conclusion
The study highlights that PESA, TESA, and micro-TESE are effective sperm extraction techniques for azoospermic patients undergoing ART. The success in sperm retrieval and subsequent pregnancy outcomes underscores the importance of selecting the appropriate method based on individual patient conditions. These findings contribute to the evidence base for optimizing fertility treatments in patients with severe male factor infertility.
Keywords
Azoospermia
Assisted Reproductive Technology
Sperm Extraction
PESA
TESA
Micro-TESE
Fertility Treatment
INTRODUCTION
Assisted reproductive technology (ART) encompasses a range of advanced medical procedures designed to aid individuals and couples in overcoming infertility challenges. Sperm extraction plays a fundamental role in ART by providing viable sperm for use in procedures such as in vitro fertilisation (IVF), intracytoplasmic sperm injection (ICSI) and other related techniques.
Various conditions can necessitate sperm extraction in ART, including obstructive azoospermia, non-obstructive azoospermia, retrograde ejaculation and cases where previous attempts at sperm retrieval have been unsuccessful.[1] These conditions highlight the diverse challenges individuals may face in achieving successful fertilisation and pregnancy.
The efficacy of sperm extraction methods in ART is paramount, as it directly influences the success rates of fertility treatments. Advanced techniques such as testicular sperm extraction (TESE), microdissection TESE (micro-TESE), percutaneous epididymal sperm aspiration (PESA) and testicular sperm aspiration (TESA) have significantly improved the ability to retrieve viable sperm even in challenging cases of severe male factor infertility.[2]
Research and clinical studies have focused on optimising these extraction methods to enhance sperm retrieval rates while minimising potential risks and complications. Factors such as sperm quality, quantity and genetic integrity are carefully assessed to ensure the best possible outcomes for fertility treatments.[3]
Moreover, advancements in sperm cryopreservation techniques have expanded the possibilities for preserving fertility in cases where sperm extraction is successful but immediate use is not required. This has particularly benefitted individuals undergoing treatments such as cancer therapies that may impact future fertility.[4]
In conclusion, the efficacy of sperm extraction techniques in ART underscores the continuous progress and innovation in reproductive medicine. These methods not only offer hope to individuals facing fertility challenges but also contribute significantly to the overall success and advancements in ARTs.
OBJECTIVE
This study aims to evaluate and compare the efficacy of various sperm extraction techniques in ART, specifically focusing on sperm retrieval rates, fertilisation rates and clinical outcomes in individuals undergoing fertility treatments.
MATERIAL & METHODS
Study Design
-
-
Retrospective observational study conducted at RISAA IVF, Green Park, New Delhi.
-
-
Duration of study: 1 year, from January 2023 to January 2024.
Participants
-
-
Inclusion Criteria:
Male participants are undergoing ART procedures (IVF or ICSI) at the clinic.
Male participants were diagnosed with azoospermia according to WHO criteria Semen Analysis (6th edition, WHO 2021), i.e., the complete absence of spermatozoa in the ejaculate in at least two semen samples, including high-speed centrifugation with an examination of the entire pellet.
History of sperm extraction using one of the following techniques: micro-TESE, PESA or TESA.
Adequate medical records and follow-up data are available.
-
-
Exclusion Criteria:
Participants with incomplete medical records or missing data.
Participants with known genetic abnormalities impacting fertility.
Patients with no sperm or immature sperm after surgical sperm extraction.
Data Collection
Data was collected from electronic medical records, laboratory reports and patient charts.
Variables of interest.
Demographic data (age, BMI, medical history).
Sperm extraction technique used (micro-TESE, PESA, TESA).
Sperm retrieval rates (% of successful sperm retrieval per technique).
Clinical outcomes (pregnancy rates, live birth rates).
Clinical Pregnancy Rate–Pregnancy confirmed via ultrasound (at six weeks post last menstrual period or 4 weeks post transfer).
Procedure
For every azoospermic patient, PESA was performed. TESA was carried out on the specimen if there was no sperm or if there was only non-motile sperm. In addition, micro-TESE was carried out if PESA and TESA had already been completed, but there were still no sperm or only non-motile sperm in the specimen. Sperm motility and quantity were assessed using light microscope with 10X magnification lens. In the IVF programme, the recovered sperm was used for ICSI. ICSI may be performed either immediately or at a later time following sperm retrieval. ‘Fresh sperm’ refers to sperm that was extracted concurrently with ovum extraction and ICSI. In the meantime, the retrieved sperm needed to be frozen in order to be used later (‘frozen sperm’) if the Oocyte retrieval and ICSI were completed at some point after the sperm retrieval.
Data Analysis
Data analysis was done using SPSS software (SPSS version 26, IBM(r), Chicago, IL, USA). When comparing categorical data, the chi-square test was employed, and when comparing means, the t-test was employed. P < 0.05 was regarded as significant.
Ethical Considerations
-
-
Approval obtained from the Institutional Review Board (IRB) or Ethics Committee.
-
-
Confidentiality and anonymity of participants ensured throughout data collection and analysis.
-
-
Informed consent was waived due to the retrospective nature of the study and the use of de-identified data.
RESULTS
RISAA IVF, New Delhi, performed surgical sperm retrieval (SSR) on 11 azoospermic patients in 2023–2024. The patients’ ages were between 31.6 +/- 5.6 & 40.4 +/- 4.5 years old.
As seen in Table 1, all azoospermic patients had PESA performed initially, but only two patients (18.1%) had viable sperm recovered. More intensive SSR (TESA/micro TESE) was necessary for the remaining nine patients (81.8%). For seven patients (63.6%) on TESA, viable sperm was discovered. MICRO TESE was necessary for the final two patients (18.1%). In seven couples (63.6%), there was a pregnancy. According to the statistical analysis in Table 2, among the SSR methods, there was no discernible variation in the pregnancy rate (p > 0.05). Table 3 shows that, in contrast to two patients (18.1%) who underwent frozen sperm cycles, nine patients (81.8%) underwent ICSI on the same day as oocyte retrieval [Figure 1].
| Technique | Number of Patients | Successful Retrieval (%) |
|---|---|---|
| PESA | 11 | 18.1% |
| TESA | 7 | 63.6% |
| Micro-TESE | 2 | 18.1% |
| Comparison | P-value | Conclusion |
|---|---|---|
| Pregnancy Rates (PESA vs TESA vs Micro-TESE) | P > 0.05 | No significant difference |
| Outcome | Conclusion |
|---|---|
| Pregnancy Rates (PESA vs TESA vs Micro-TESE) | No significant difference |
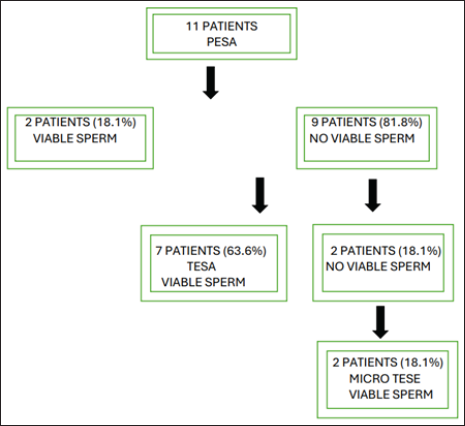
- Study design. PESA: Percutaneous epididymal sperm aspiration; TESA: Testicular sperm aspiration; MICRO-TESE: Microdissection testicular sperm extraction
As depicted in Table 4, hundred per cent (2) of the patients in the PESA group, 57.1% (4) of the patients in the TESA group and 50% (1) of the patients in the micro-TESE group were successful in achieving pregnancy.
| Technique | Successful Retrieval (n) | Pregnancy Achieved (n) | Pregnancy Rate (%) |
|---|---|---|---|
| PESA | 2 | 2 | 100% |
| TESA | 7 | 4 | 57.1% |
| Micro-TESE | 2 | 1 | 50% |
DISCUSSION
‘Absence of sperm in ejaculate after centrifugation’ is the definition of azoospermia. NOA or OA are two different clinical diagnoses that are typically observed in men with azoospermia.[5] These days, ART has established itself as a reliable option for these men to become parents, with reliable outcomes in both classes.
Surgical intervention can be used to locate sperm in the testis or epididymis of azoospermic patients. Since its development two decades ago, sperm retrieval by PESA, TESA and TESE has demonstrated a good success rate.[6] In this investigation, viable sperm can be obtained using micro-TESE, TESA and PESA techniques. According to a 2011 study by Esteves et al., retrieving sperm using MESA or TESE had a higher success rate than using PESA.[7] Similar results were found in this study: after failing in PESA, viable sperm could be retrieved in seven patients (63.6%) by TESA and in two patients (18.1%) by micro-TESE (p < 0.05).
There could be a number of reasons for the higher success rate in sperm retrieval by TESA or TESE in this study as opposed to PESA, including a higher percentage of non-obstructive azoospermic patients, technical challenges in executing precise PESA (hematoma or missed puncture site) and superior sperm quality and quantity in testes. Even though TESA or TESE had a higher success rate than PESA at retrieving sperm, in our setting, PESA is still the first treatment of choice for azoospermic patients for a number of reasons: it is highly successful at retrieving sperm, causes little discomfort to the patients, has a lower rate of complications than TESA or TESE, is less expensive, is simple to repeat in an outpatient clinic and doesn’t require a microscope.
Numerous studies assessed the success rates of different surgical sperm retrieval techniques. The success rate by PESA and TESA was higher in patients with obstructive azoospermia than non-obstructive azoospermia, and TESE has a higher success rate than PESA, according to various studies by [Dohle et al. (1998),[8] Levine et al. (2003)[9] and Esteves et al. (2011)].[7] Our success rate may have been comparable to that of the same group in the Esteves et al. study because a larger percentage of non-obstructive azoospermic patients were included in our analysis (PESA group: 31.5% vs 35% and TESE group: 41.3% vs 50%).[7] This study compared the sperm retrieval techniques (TESE and PESA) in order to assess the pregnancy rate in IVF courses. Pregnancy rates did not vary depending on whether sperm was recovered using TESE or PESA. Research by Semiao-Fransisco et al. (2010)[10] and Pasqualotto et al. (2002)[11] revealed no difference in the pregnancy rate between sperm recovered by TESE and PESA. Furthermore, a lack of evidence prevented the Cochrane review from concluding whether the surgical sperm retrieval methods and the pregnancy rate in IVF programmes were correlated.
In the meantime, a study conducted in 2000 by Mercan et al.[12] revealed that in non-obstructive azoospermic patients, the pregnancy rate in IVF was higher when sperm was extracted using less invasive techniques. The quality of the sperm was a major factor in the pregnancy success rate. As a result, sperm quality and sperm retrieval ease were related. Less invasive methods and higher concentrations of retrieved sperm were associated with easier sperm retrieval. According to certain research, patients with non-obstructive azoospermia and those who had less concern for sperm (difficult sperm retrieval) had higher rates of spermatogenetic impairment and chromosomal abnormalities.
The pregnancy rates between sperm recovered by TESE and PESA did not differ statistically in our investigation (p > 0.05). Two biases may have contributed to this outcome: the high concentration of sperm recovered from our patients and the lack of distinction between obstructive and non-obstructive azoospermic patients. This may indirectly result in the inclusion of patients with higher sperm concentrations and, as a result, likely better sperm quality (lower chromosomal abnormalities and spermatogenetic impairment). Moreover, factors related to the spouse (a female) that were not examined in this study also had an impact on the success rate of pregnancy.
Limitations
Retrospective design may limit the availability of certain data points or introduce potential biases.
A small sample size (11 participants) may affect the generalisability of findings.
Lack of a control group for direct comparison of outcomes between different extraction techniques.
CONCLUSION
The study aims to provide valuable insights into the efficacy of sperm extraction techniques in ART, with a focus on sperm retrieval rates, quality parameters, and fertilisation rates, contributing to the evidence base for optimising fertility treatments. Using PESA, TESA, and TESE, sperm can be extracted from azoospermic patients, and surgically extracted sperm has a good success rate in achieving clinical pregnancy during IVF.
Ethical approval
The study was approved by the Institutional Ethics Committee, Ethical committee number Ec/Iirft/24-01.
Declaration of patient consent
Patient’s consent not required as patients’ identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
REFERENCES
- Differential Diagnosis of Azoospermia in Men with Infertility. J Clin Med. 2021;10:3144.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Surgical Sperm Retrieval: Techniques and Their Indications. Indian J Urol. 2011;27:102.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Sperm Retrieval Rates and Clinical Outcomes for Patients with Different Causes of Azoospermia Who Undergo Microdissection Testicular Sperm Extraction-intracytoplasmic Sperm Injection. Asian J Androl. 2021;23:59.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Advancements in Fertility Preservation Strategies for Pediatric Male Cancer Patients: A Review of Cryopreservation and Transplantation of Immature Testicular Tissue. Reprod Biol Endocrinol. 2024;22:47.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Comparative Analysis of Surgically Retrieved Sperms in Cases of Obstructive and Nonobstructive Azoospermia Treated for Infertility. J Hum Reprod Sci. 2020;13:201.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- An update on sperm retrieval techniques for azoospermic males. Clinics.. 2013;68:99-10.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Sperm Retrieval Techniques for Assisted Reproduction. Int Braz J Urol. 2011;37:570-83.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical Sperm Retrieval and Intracytoplasmic Sperm Injection as Treatment of Obstructive Azoospermia. Hum Reprod. 1998;13:620-3.
- [CrossRef] [PubMed] [Google Scholar]
- Testicular and Epididymal Percutaneous Sperm Aspiration in Men with Either Obstructive or Nonobstructive Azoospermia. Urology. 2003;62:328-32.
- [CrossRef] [PubMed] [Google Scholar]
- Assisted Reproductive Technology Outcomes in Azoospermic Men: 10 years of Experience with Surgical Sperm Retrieval. Aging Male. 2010;13:44-50.
- [CrossRef] [PubMed] [Google Scholar]
- Outcome of In Vitro Fertilization and Intracytoplasmic Injection of Epididymal and Testicular Sperm Obtained from Patients with Obstructive and Nonobstructive Azoospermia. J Urol. 2002;167:1753-6.
- [CrossRef] [PubMed] [Google Scholar]
- Outcome of Testicular Sperm Retrieval Procedures in Non-obstructive Azoospermia: Percutaneous Aspiration versus Open Biopsy. Hum Reprod. 2000;15:1548-51.
- [CrossRef] [PubMed] [Google Scholar]







