Translate this page into:
Categorisation of Adnexal Masses in Infertile Women: A Retrospective Cohort Analysis

*Corresponding author: Dr. Aditi Jain, MD, Department of Centre for IVF and Human Reproduction, Sir Gangaram Hospital, Rajendra Nagar, Delhi, India aditijain1205@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Jain A, Satwik R, Majumdar A, Rastogi D, Rao S, Kankra M. Categorisation of Adnexal Masses in Infertile Women: A Retrospective Cohort Analysis. Fertil Sci Res. 2024;11:17. doi: 10.25259/FSR_22_2024
Abstract
Objectives
Adnexal lesions are often detected incidentally during infertility evaluation. However, limited data exists on the pathological profile of adnexal lesions detected, particularly in infertile women. In this study, we aim to assess the histopathological profile of adnexal masses in infertile women.
Material and Methods
Retrospective analysis of infertile women with an adnexal mass undergoing surgery between 1 January 2018 and 30 May 2024 was done. Details pertaining to demographic profile, ultrasonography, biochemical markers, surgical findings and histopathology were retrieved. Histopathological profile was studied as per the Royal College of Obstetricians and Gynaecology (RCOG) histopathological classification. Statistical analysis was done using the SPSS Statistics software (v27.0).
Results
Of the 5170 patients screened, 62 patients eligible for study criteria were included. The mean age (standard deviation [SD]) was 33.1 (4.6) years, with 85.5% (53/62) of patients being nulliparous. Ultrasonographic evaluation revealed bilateral adnexal lesions in 25.8% (16/62) patients. Most patients underwent laparoscopic surgery (91.9%, 57/62). CA-125 was available for 34 patients and was raised in 58.9% (20/34) patients. The histopathological profile revealed 93.6% (58/62) of patients having benign lesions of ovarian origin, while 3.2% (2/62) had benign lesions of non-ovarian origin. Endometriosis (66.1%, 41/62) and mature teratoma (12.9%, 8/62) were the most common benign lesions. Two patients (3.2%) with malignancy had borderline mucinous tumours.
Conclusion
Benign ovarian lesions form the most common adnexal masses in women of reproductive age group who present with infertility; however, malignancy is not uncommon. Endometriosis and mature teratoma appeared to be the most common benign lesions.
Keywords
Adnexal mass
Infertility
Laparoscopy
Ovarian malignancy
Endometriosis
INTRODUCTION
Adnexal masses comprise lesions which arise from the adnexal region of the uterus. Though the term ’adnexa’ has its origin in the Latin term ’adnexus’, which implies appendage, adnexal lesions include lesions arising from ovaries, fallopian tubes or any of the structures lying in the vicinity of the uterus, such as broad ligament of the uterus or parametrium. Their prevalence ranges between 7% and 10%.[1,2] Adnexal masses can be of gynaecologic or non-gynaecologic origin. Among gynaecologic origin, the adnexal masses can be classified as ovarian or non-ovarian based on the organ of origin and benign or malignant based on the neoplastic ability. In premenopausal women, benign cysts, leiomyomata and ectopic pregnancy comprise the most common adnexal masses, whilst ovarian malignancy is rare. Corpus luteum cyst is the most adnexal lesion in pregnant women, whereas functional cysts and leiomyomata are most common in non-pregnant women.[3,4] Sometimes, pathology in contiguous structures such as the appendix may also present as an adnexal mass, especially on radiological examination. Although an adnexal mass can be found in women of all age groups, it is most frequently reported in women of reproductive age.[4] An adnexal mass can be benign or malignant, and this risk of malignancy necessitates early and accurate diagnosis. About 10% of women may undergo surgery for a mass in their lifetime. Of these, less than 20% will be malignant.[2] The evaluation of adnexal lesions involves history and physical examination, ultrasonography, biochemical markers and often laparoscopy.[3]
Adnexal masses are often incidentally found on ultrasounds when evaluating infertile women. The risk of malignancy necessitates early and accurate diagnosis to lessen morbidity and mortality. However, limited data[5,6] exist on the systematic characterisation of these adnexal lesions amongst women who present with infertility. Our study aims to characterise these adnexal lesions as per the Royal College of Obstetricians and Gynaecology (RCOG) histopathological classification[7] and estimate their distribution in patients presenting with infertility.
MATERIAL AND METHODS
After approval from the Institutional Ethics Committee, a retrospective analysis of reproductive-aged women (18–45 years) was performed. Women who presented with infertility and underwent surgery for an adnexal mass between 1 January 2022 and 1 May 2024 were included. Their demographic parameters, including age, parity, associated menstrual disturbances and history of prior hormonal therapy and prior surgery, were included. Biochemical markers, including cancer antigen (CA)-125, CA-19.9, carcinoembryonic antigen (CEA), lactate dehydrogenase (LDH), alpha-fetoprotein (AFP), beta human chorionic gonadotropin (beta-hCG), human epididymis protein-4 (HE4) and Risk for Ovarian Malignancy Algorithm (ROMA) index were recorded. The ultrasonographic and laparoscopic findings were also recorded. The histopathological reports were retrieved, and the adnexal lesions were classified as per RCOG classification.[7] The Institutional Ethics Committee approved the study (ref no: F.1/IEC/IFS/2023/No.15).
Statistical analysis
All the data were entered in a Microsoft Excel datasheet using a pre-filled proforma. Categorical variables were expressed as proportions (percentage), and continuous variables were expressed as mean ± standard deviation (SD) or median (interquartile range [IQR]) as appropriate. Categorical variables were compared using the Chi-square test, and continuous variables were compared using the student’s t-test, Multiple Analysis of Variance (MANOVA), Mann-Whitney test or Kruskal-Wallis test as appropriate. All statistical tests were two-sided. Statistical significance was taken as p < 0.05. Data were analysed using IBM SPSS Statistics software (version 27.0, Chicago, IL, USA).
RESULTS
Records of 5170 patients who underwent a gynaecologic surgery between 1 January 2022 and 23 December 2023 were screened. After eliminating women above 45 and below 18, we were left with 2060 patients. Records of these 2060 patients were individually analysed for the presence of adnexal masses, and 503 patients were screened for clinical presentation. Of these 503 patients, 62 patients presented for the evaluation of infertility, which comprised our study population.
The mean age (SD) was 33.1 (4.6) years, and 85.5% (53/62) of patients were nulliparous. Most patients had eumenorrhea (53.2%, 33/62) and had received prior hormonal therapy (72.6%, 45/62). Table 1 highlights the demographic profile of the study population.
| Parameter | Mean (SD) for numerical variables |
|---|---|
| N (%) for categorical variables | |
| Mean age (SD), years | 33.1(4.6) |
| Parity | |
| Nulliparous, n(%) | 53(85.5%) |
| Multiparous, n(%) | 9(14.5%) |
| Menstrual cycles | |
| Eumenorrhea, n(%) | 33(53.2%) |
| Menorrhagia, n(%) | 23(37.1%) |
| Hypomcnorrhca, n(%) | 06(9.7%) |
| H/o oral ovulogens/gonadotropin intake | |
| None | 17(27.4%) |
| 1 or 2 cycles | 26(41.9%) |
| 3 or more cycles | 19(30.7%) |
| H/o prior surgery | |
| Yes, n(%) | 10(16.1%) |
| No, n(%) | 52(83.9%) |
H/o- History of; SD-Standard Deviation
The ultrasonographic evaluation revealed bilateral adnexal lesions in 25.8% (16/62) patients, and the median (IQR) largest dimension of the adnexal mass was 4.8 (3.6,7.3) cm. Most lesions were cystic in consistency (85.5%, 53/62) and unilocular (88.3%, 53/60). Only 14.5% (9/62) of patients had septations on ultrasonography. None of the patients had ascites on ultrasonography. Based on ultrasonographic evaluation, all lesions appeared to be benign, with 96.8% (60/62) of ovarian in origin and 3.2% (2/62) of non-ovarian in origin. Most patients underwent laparoscopic surgery for adnexal masses (91.9%, 57/62), whereas only 8.1% (5/62) underwent laparotomy. On laparoscopy, 59.7% (37/62) of patients had intraoperative pelvic adhesions. Table 2 depicts the comparison of laparoscopic and ultrasonographic features of adnexal masses.
| Parameter | Surgical findings | USG findings | p-value# |
|---|---|---|---|
| Surgical approach | |||
| Laparoscopic, n(%) | 57(91.9%) | ||
| Laparotomy upfront, n(%) | 5(8.1%) | ||
| Largest dimension of mass, median (IQR), cm | >(3.7) | 4.8(3.6,7.3) | 039 |
| Locularity (n=60) | 0.76 | ||
| Unilocular. n(%) | 54(90%) | 53(883%) | |
| Multilocular, n(%) | 6(10%) | 7(11.7%) | |
| Consistency | 0.79 | ||
| Cystic, n(%) | 54(87.1%) | 53(85.5%) | |
| Mixed, n(%) | 08(12.9%) | 9(14.5%) | |
| Laterality | 1.0 | ||
| Unilateral, n(%) | 46(74.2%) | 46(74.2%) | |
| Bilateral, n(%) | 16(25.8%) | 16(25.8%) | |
| Septations | |||
| Yes, n(%) | 08(12.9%) | 09(14.5%) | 0.79 |
| No, n(%) | 54(87.1%) | 53(85.5%) | |
| Intraoperative Adhesions | |||
| No | 25(40.3%) | ||
| Yes | 37(59.7%) | ||
| Flimsy, n(%) | 35(56.5%) | ||
| Dense, n(%) | 02(3.2%) | ||
| Predominantly pelvic, n(%) | 37(59.7%) | ||
| Presence of papillary projections (n=60) | |||
| Yes, n(%) | 0 | 0 | |
| No, n(%) | 60(100%) | 60(100%) | |
| Presence of ascites | |||
| Yes, n(L%) | 0(0%) | 0(0%) | |
| No, n(%) | 62(100%) | 62(100%) | |
| Diagnosis* | 036 | ||
| Benign ovarian, n(%) | 58(93.6%) | 60(96.8%) | |
| Benign non-ovarian, n(%) | 2(3.2%) | 2(3.2%) | |
| Malignant ovarian, n(%) | 2(3.2%) | 0 | |
| Malignant non-ovarian, n(%) | 0 | 0 |
*Diagnosis on laparoscopic findings is based on histopathological findings:
#p<0.05 is considered statistically significant
IQR- Interquartile range
Biochemical markers were available for limited patients, and Table 3 outlines the biochemical assessment available for the study cohort. CA-125 was available for 34 patients and was raised in 58.9% (20/34) patients. CA-19.9 was raised in 22.2% (2/9) patients, and LDH was raised in 27.3% (3/11) patients. ROMA index was high risk in 11.1% (1/9) patients. However, all the patients with raised tumour markers had benign histopathology on surgical specimens.
| Tumour marker | N(%) for categorical variables |
|---|---|
| CA-125 (n = 34) | |
| Normal | 14 (41.2%) |
| Abnormal | 20(58.8%) |
| CA-19.9 (n = 9) | |
| Normal | 7(77.8%) |
| Abnormal | 2(2.2%) |
| CEA (n = 9) | |
| Normal | 9(100%) |
| Abnormal | 0 |
| AFP (n = 11) | |
| Normal | 11(100%) |
| Abnormal | 0 |
| Beta-hCG (n = 8) | |
| Normal | 8(100%) |
| Abnormal | 0 |
| LDH (n = 11) | |
| Normal | 8(72.7%) |
| Abnormal | 3(27.3%) |
| HE4 (n = 9) | |
| Normal | 8(88.9%) |
| Abnormal | 1(11.1%) |
| ROMA (n = 9) | |
| Low risk | 8(88.9%) |
| High risk | 1(11.1%) |
ROMA: Risk for Ovarian malignancy algorithm; AFP: Alpha fetoprotein; CA-19.9: Carbohydrate antigen 19.9; CEA: Carcinoembryonic antigen; hCG: Human chorionic gonadotropin; HE4: Human epididymis protein 4; LDH: Lacate dehydrogenase
The histopathological characterisation of adnexal masses revealed 93.6% (58/62) patients having benign lesions of ovarian origin, while 3.2% (2/62) patients had benign lesions of non-ovarian origin [Figure 1]. Approximately 3.2% (2/62) of patients had malignant lesions of ovarian origin. Amongst the benign ovarian lesions, endometriosis (66.1%, 41/62) and mature teratoma (12.9%, 8/62) were the most common lesions, followed by mucinous cystadenoma (6.6%, 4/62) and functional cysts (4.8%, 3/62). Figure 2 depicts the distribution of various benign ovarian lesions. The two patients with benign non-ovarian lesions had tubal/paratubal cysts. Amongst patients with malignant ovarian lesions, both patients had borderline mucinous tumours. Table 4 depicts the histopathological distribution of adnexal masses in our study population.
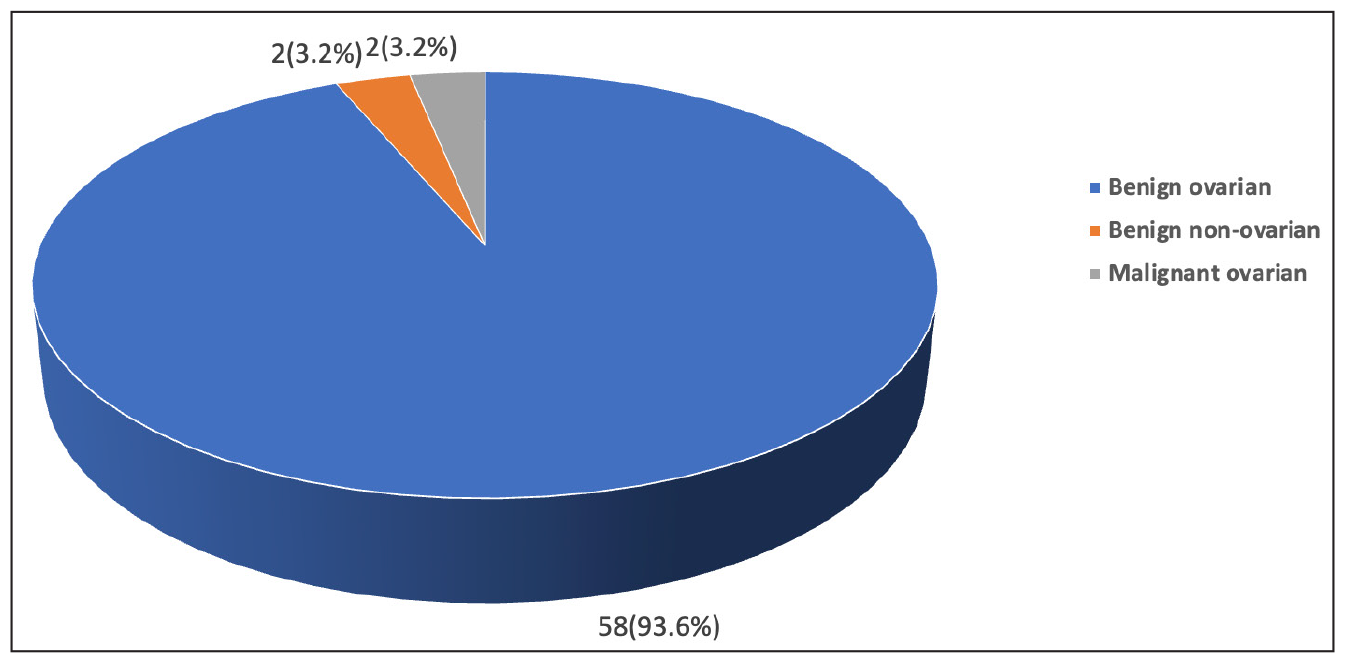
- Histopathological categorisation of adnexal lesions in the study cohort (n = 62).
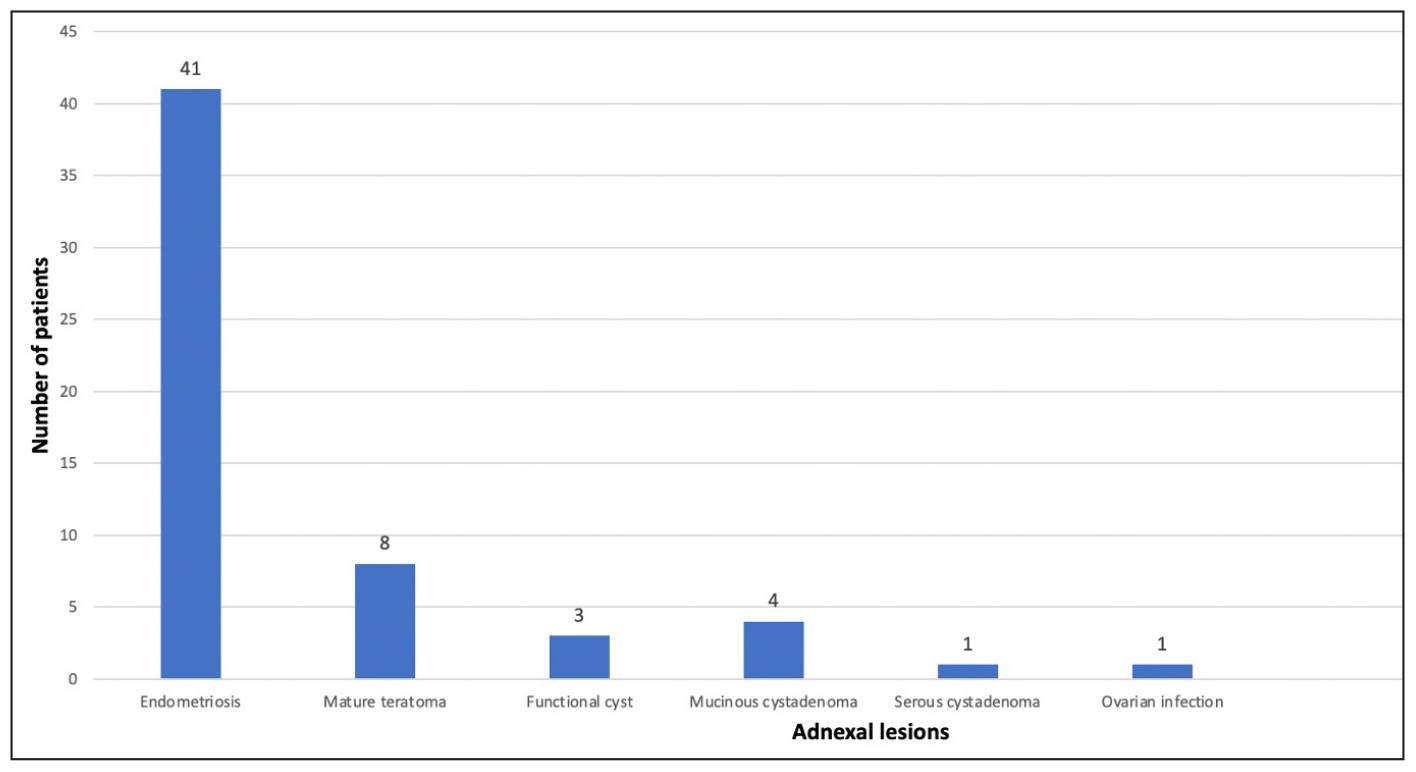
- Distribution of various benign adnexal lesions (n = 58).
| Pathological diagnosis | N(%) for categorical variables |
|---|---|
| Benign Ovarian | 58(93.6%) |
| Endometriosis | 41(66.1%) |
| Mature teratoma | 8(12.9%) |
| Functional cyst | 3(4.8%) |
| Mucinous cystadenoma | 4(6.6%) |
| Serous cystadenoma | 1(1.6%) |
| Ovarian infection | 1(1.6%) |
| Benign Non-ovarian | 2(3.2%) |
| Tubal/paraovarian cyst | 2(3.2%) |
| Malignant ovarian | 2(32%) |
| Borderline mucinous tumour | 2(3.2%) |
| Malignant Non-ovarian | 0 |
‘Bold’ font signify the values for broad categorisation of adnexal mass i.e. benign ovarian, benign non-ovarian, malignant ovarian and malignant non-ovarian.
DISCUSSION
Adnexal masses are often incidentally diagnosed on ultrasounds during the evaluation of infertile women. Though many can be managed conservatively, a small possibility of malignancy warrants timely intervention. In our study, we found that most of the masses were benign (96.8%), 96.8% of masses were of ovarian origin, and only 3.2% were malignant. Endometriosis and mature teratoma remained the most common benign ovarian lesions, while borderline mucinous tumour was the most common malignant lesion.
Various studies have assessed the demographic profile of patients presenting with adnexal mass. In a study from Eastern India evaluating the clinicopathological profile of adnexal lesions in 59 women, with 76% being premenopausal, Dasgupta et al.[8] reported 62% of women being multiparous and 16% of patients having bilateral lesions. Similarly, Bandi et al.[4] studied 100 patients from South India with an adnexal mass, of which 90% were in the reproductive age group and reported abdominal pain as the most common presenting symptom, with only 16% being nulliparous. Several other studies from the Indian subcontinent reported similar findings.[5,6,9,10] However, none of these studies assessed the profile of adnexal lesions, particularly for infertile women. In contrast to the above studies, all our patients wanted to conceive, where 85.5% were nulliparous, and 25.8% had bilateral adnexal lesions.
Ultrasonography is an important tool for the detection and evaluation of adnexal mass in patients presenting with infertility. As the experience with ultrasonography for the characterisation of adnexal masses has evolved, various nomograms and strategies have been proposed to increase the sensitivity and specificity for discrimination between benign and malignant lesions.[11] In a systematic review of recent studies evaluating various ultrasonography models, ultrasonography has been shown to have a sensitivity of 85–90% and specificity of 90–95%.[12] In our study cohort, all patients, except two, reported to be ’probably benign’ on ultrasonography turned out to be malignant on the final histopathology with a false positive error rate of 3.2%.
Biochemical assessment is an integral part of evaluation for adnexal masses. CA-125 is the most widely used tumour marker and is elevated in 50% of cases with early malignancy and up to 92% of cases with advanced malignancy; however, the high false positive rate makes it difficult to differentiate benign and malignant lesions.[13] In our study cohort as well, CA-125 was raised in 58.9% of patients; however, all these patients had benign lesions. ROMA index appeared to be a more accurate model based on CA-125 and HE4 and menopausal status with a sensitivity of 90% and specificity of 92% for differentiating malignancy from benign lesions.[14] In our study cohort as well, the ROMA index was available for nine patients, of which eight were low risk and benign on histopathology.
Various researches have tried to study the pathological profile of adnexal lesions. In a cohort of 511 U.S. women with adnexal lesions, 85.2% of lesions in the study were benign. Endometriosis and mature teratoma were the most common benign lesions.[15] Similarly, in another European cohort of 4905 women, 56% were premenopausal, and 70% of the lesions were benign.[16] In another multi-institutional European study involving 3511 women, Ameye et al. also reported endometriosis (20.3%) and teratoma (11.3%) as the most common benign lesions. [17]
Few studies from the Indian subcontinent have tried to characterise the adnexal lesions. Bhagde et al.[5] studied 50 patients with adnexal lesions prospectively in a tertiary care hospital. Approximately 86% of the masses were ovarian in origin, with benign cystic teratoma, with mucinous cystadenoma being the most common histopathological diagnosis. Bandi et al. [4] studied 100 patients with adnexal lesions, with 10% of patients being post-menopausal. In their study, simple cysts and serous cystadenoma were the most common benign lesions, and serous cystadenocarcinoma was the most common malignant lesion. Deshmukh et al.[6] studied 88 women with adnexal masses undergoing surgery. A benign ovarian tumour (69.32 %) was the most common diagnosis, followed by a malignant ovarian tumour (12.5%), ectopic pregnancy (9.09%), hydrosalpinx (5.68 %) and broad ligament fibroid (3.41%). Agarwal et al.[18] studied 81 patients with adnexal mass and reported 86.4% having benign lesions while 13.6% had malignant lesions with two cases of borderline variety. Rai et al. [10] studied 127 patients with adnexal masses and reported that 80.3% of adnexal masses were of ovarian origin, with 12.7% of them being malignant. Serous cystadenocarcinoma was the most common ovarian cancer. The most common benign lesion was mature cystic teratoma (61.6%), followed by serous cystadenoma (31.5%) and mucinous cystadenoma (6.8%). Compared to these studies, the proportion of malignant adnexal lesions remains low in our study cohort. This can be attributed to the fact that our study comprises of reproductive-aged women desiring fertility.
Our study has several limitations. It is a retrospective analysis of a single tertiary hospital-based database. We studied patients with adnexal lesions undergoing surgery. Multiple radiologists were involved in the evaluation of adnexal lesions, though the ultrasonography was done by expert radiologists. The histopathological specimens were not centrally reviewed. Despite these limitations, our study is the first attempt to study the histopathological profile of adnexal lesions detected in patients presenting with infertility.
CONCLUSION
Benign ovarian lesions form the most common adnexal masses in women of reproductive age group presenting with infertility; however, malignancy is not uncommon. Endometriosis and teratoma appeared to be the most common benign lesions. Ultrasonography and biochemical marker evaluation play an important role in the evaluation of adnexal masses.
Ethical approval
The research/study approved by the Institutional Review Board at the Indian Fertility Society, number F.1/IEC/IFS/2023/No.15, dated 23/12/2023.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
REFERENCES
- Transvaginal Sonographic Ovarian Findings in a Random Sample of Women 25–40 Years Old. Ultrasound Obstet Gynecol. 1999;13:345-50.
- [CrossRef] [PubMed] [Google Scholar]
- Management of the Adnexal Mass: Considerations for the Family Medicine Physician. Front Med (Lausanne). 2022;9:913549.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Diagnosis and Management of Adnexal Masses. Am Fam Physician. 2009;80:815-20.
- [PubMed] [Google Scholar]
- A Clinicopathological Study of Adnexal Masses in the Tertiary Care Hospital, Kadapa. Int J Reprod Contracept Obstet Gynecol. 2022;11:3295-9.
- [Google Scholar]
- Int J Reprod Contracept Obstet Gynecol. 2017;6:262-5.
- Histopathological Study of Adnexal Masses at a Teaching Hospital. MedPulse Int J Gynaecology. 2021;18:53-7.
- [Google Scholar]
- Evaluation of Adnexal Masses – Correlation of Clinical and Radiologic Features with Histopathologic Findings: An Observational Study in a Tertiary Care Center of Eastern India. Biomed Biotechnol Res J. 2021;5:21-6.
- [Google Scholar]
- Adnexal mass: A Clinicopathological Study at a Tertiary Care Centre in Assam, India. Int J Reprod Contracept Obstet Gynecol. 2019;8:1457-62.
- [CrossRef] [Google Scholar]
- Clinicopathological Profile of Adnexal Masses Presenting to a Tertiary-Care Hospital in Bhutan. South Asian J Cancer. 2019;8:168-72.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Assessment of Adnexal Masses Using Ultrasound: A Practical Review. Int J Womens Health. 2014;6:857-63.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Presurgical Diagnosis of Adnexal Tumours Using Mathematical Models and Scoring Systems: A Systematic Review and Meta-Analysis. Hum Reprod Update. 2014;20:449-62.
- [CrossRef] [Google Scholar]
- CA125 and Ovarian Cancer: A Comprehensive Review. Cancers (Basel). 2020;12:3730.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Clinical value of ROMA Index in Diagnosis of Ovarian Cancer: Meta-Analysis. Cancer Manag Res. 2019;11:2545-51.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Diagnostic Performance of Ultrasonography-Based Risk Models in Differentiating Between Benign and Malignant Ovarian Tumors in a US Cohort. JAMA Netw Open. 2023;6:e2323289.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Validation of Models to Diagnose Ovarian Cancer in Patients Managed Surgically or Conservatively: Multicentre Cohort Study. BMJ. 2020;370:m2614.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Clinically Oriented Three-Step Strategy for Assessment of Adnexal Pathology. Ultrasound Obstet Gynecol. 2012;40:582-91.
- [CrossRef] [PubMed] [Google Scholar]
- Analysis of Patients Presenting with Adnexal Mass in a Tertiary Care Centre. J Clinical Diagnostic Res. 2019;13:QC04-QC06.
- [Google Scholar]







