Translate this page into:
Prenatal Implications in A Robertsonian Translocation Silent Carrier Female – A Case Report
*Corresponding author: Dr IMS Sandhu, Assistant Professor, Department of Genetics, Sri Guru Ram Das Institute of Medical Sciences & Research, SGRDUHS, Amritsar, India. imssandhu.gen@sgrdimsr.in
-
Received: ,
Accepted: ,
How to cite this article: Kaur S, Sood R, Singh Sandhu IM, Bhanwer AJS. Prenatal Implications in A Robertsonian Translocation Silent Carrier Female–A Case Report. Fertil Sci Res. 2024;11:2. doi: 10.25259/FSR_45_23
Abstract
Robertsonian translocation (RT) involves the end-to-end fusion of two acrocentric chromosomes. RT between chromosome 21 and any other acrocentric chromosome can lead to infertility, early pregnancy miscarriages or the birth of a Down syndrome (DS) baby in silent carriers. DS is a genetic disorder characterised by distinct physical features and some degree of cognitive disability. Mainly there are three cytogenetic forms of DS – full trisomy 21, mosaic trisomy 21 and RT trisomy 21. However, genetic counselling and targeted prenatal diagnostic testing can help RT carriers give birth to a normal baby. With this, we present a case report where preconception and prenatal genetic counselling and testing helped a RT Carrier female give birth to a healthy child.
Keywords
Down Syndrome
Infertility
Prenatal Diagnosis
Robertsonian Translocation
Silent Carrier
INTRODUCTION
Down syndrome (DS) and the chromosomal abnormality related to it are the most common genetic reasons for congenital malformations in the human population. It was first recognised in the year 1933 with an incidence of 1/733 new births.[1] In India, the incidence is 1.4/1000 live births, which accounts for nearly 40,000 babies born with DS every year.[2] Chromosomal aberrations, including full trisomy of chromosome 21, a translocation between acrocentric chromosomes or mosaic cell lines carrying extra DS region, can cause this disorder.[3] Among all chromosomal aberrations, Robertsonian translocations (RTs) represent the largest number with an incidence of 1.23/1000 live births and are the most common and involve the end-to-end fusion of two acrocentric chromosomes. The silent carriers of RTs have a high risk for miscarriages and progeny with physical anomalies and mental disorders.[4] RTs involving chromosomes 14 and 21 are the most common RTs known to cause DS in the foetus.[5] Chromosomal meiotic disjunction process during gametogenesis of the RT 14q;21q silent carrier can explain the genetic mechanism for offspring of such carrier. Chromosomal segregation and disjunction occur during gametogenesis, and for a silent carrier of RT 14q;21q, this gametogenesis can lead to six types of gametes [Figure 1]. Six types of embryos can be produced after fertilisation with gametes of a cytogenetically normal partner with these gametes [Table 1].[4]
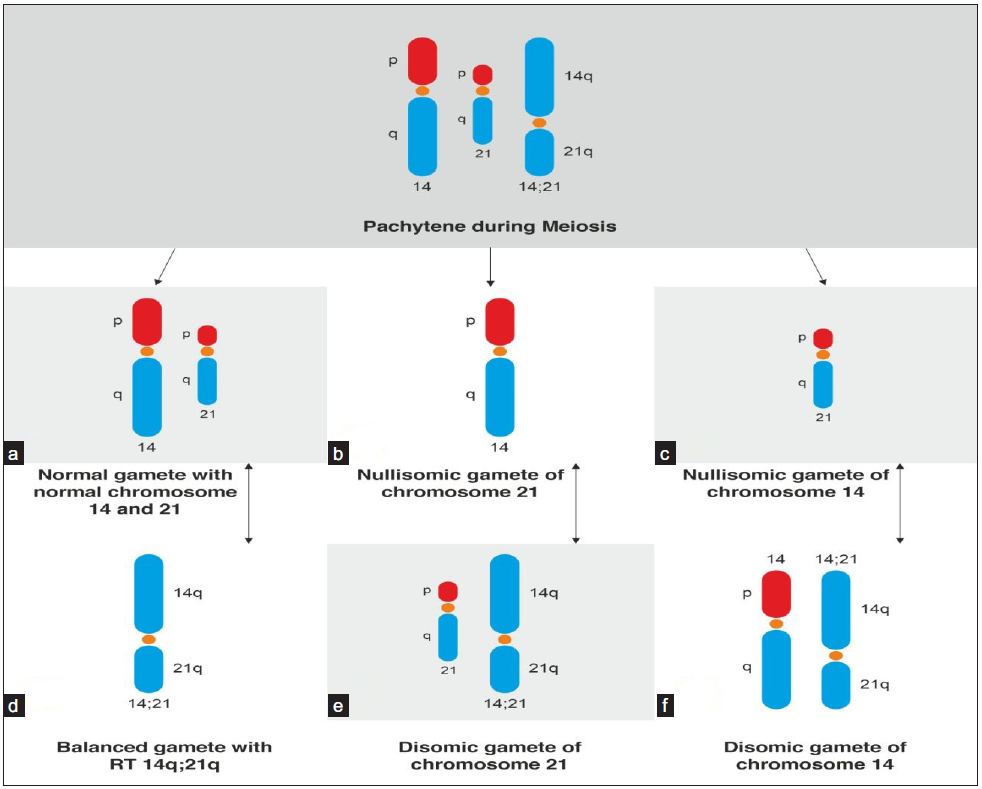
- Chromosomal disjunction and segregation during meiosis (in gametogenesis) in the Robertsonian translocation 14q;21q silent carrier. (a) Normal gamete with normal chromosome 14 and 21, (b) Nullisomic gamete of chromosome 21, (c) Nullisomic gamete of chromosome 14, (d) Balanced gamete with RT 14q;21q, (e) Disomic gamete of chromosome 21, and (f) Disomic gamete of chromosome 14. (Modified from Kolgeci et al., 2015).
| Female ♀ → | 14,21 | 14q;21q | 14 | 21 | 14q;21q,21 | 14, 14q;21q |
|
Male ♂ ↓ 14,21 |
||||||
| Embryo | 14,21: 14,21 | 14,21:14q;21q | 14,21: 14 | 14,21:21 | 14,21:14q;21q,21 | 14,21:14,14q;21q |
| Normal | Silent RT carrier | Monosomy 21 | Monosomy 14 | Trisomy 21 | Trisomy 14 | |
RT: Robertsonian Translocation
CASE REPORT
A higher middle-class income group couple visited the outpatient section of a tertiary healthcare hospital for infertility treatment. Both partners were above the age of 30 years. The couple was infertile for the last 3 years and had not taken any treatment for it. The workup for infertility was done at the Department of Obstetrics & Gynaecology (OBG), and it revealed that both the male and female were normal for their reproductive health. The male was found to be normozoospermic and the female was having a normal menstruation cycle with a normal hormonal profile. The case was marked as idiopathic by the OBG Department and referred to the Genetics Department for genetic counselling and genetic testing if required.
First Session of Genetic Counselling
During the first session of genetic counselling (GC), an extended family history was taken from the couple. As per the information given by them, there was no chromosomal or monogenic disorder present in the family. As the case was marked as idiopathic by the Department of OBG, after taking the family history, couple karyotyping was recommended as the first line of genetic testing to rule out any chromosomal abnormality.
Second Session of GC
The couple came up with their karyotyping reports. The chromosomal analysis report showed a normal euploid cytogenetic constitution for the male partner (46, XY). The genotype of the female showed the presence of an RT between chromosomes 14 and 21 [45, XX, rob(14;21)(q10;q10)]. Being an RT carrier, the chance of a DS child being born is higher if conception is successful.[5] In this session, all the risk analyses were done and explained to the couple. In the case of pregnancy, the risk chances of the foetus being Down syndromic, being a silent carrier for RT, being cytogenetically normal and the chances of miscarriage in case of the foetus being monosomic for chromosomes 14 and 21 were also explained to the couple. As the couple is also over the age of 30 years, the age-related risk for trisomies was also explained to the patient. As many studies suggested that ovulation drugs or assisted reproductive techniques using hormonal therapies can lead to cytogenetic abnormalities in sperm or ova, leading to many genetic disorders in progeny,[6] the couple was advised to try for natural conception, to which the couple agreed. The female was also provided with reproductive genetic counselling and was put on lifestyle modifications for the good health of her ova.
The couple was put on antioxidant supplements and was asked to follow good, balanced dietary habits, which they followed consistently with regular visits to the genetic clinic and the Department of OBG. The couple was supported psychologically for a long time on telegenetic counselling sessions, helping them overcome the emotional and psychological burden.
Third Genetic Counselling Session
The female conceived naturally after one and a half years, but the couple was very anxious and feared giving birth to a child with DS. To make them comfortable and to address their anxiety, they were told about all the prenatal screening and diagnostic tests available to rule out the probability of a DS child.
In consultation with the concerned gynaecologist, a foetal well-being ultrasonography (FWB-USG) at 8 weeks of gestation, NT/NB scan at gestation around 13 weeks, and TIFFA (Targeted Imaging for Foetal Anomalies) scan at around 20 weeks of gestation were suggested to the female. As the couple wanted to go for an early screening test, a non-invasive prenatal test (NIPT) at a gestation of 12 weeks was advised to the couple to rule out the possibility of chromosomal trisomies. The amniotic fluid-based diagnostic tests were recommended to the patient at a gestation of 16 weeks. To rule out any aneuploidy involving chromosomes 13, 18, 21 and sex chromosomes, QF-PCR analysis was recommended. To detect any numerical or structural chromosome rearrangements, karyotyping for the foetus was also suggested. Chromosomal microarray analysis (CMA) to evaluate pathogenic copy number variations (CNVs) was also recommended.
Fourth Genetic Counselling session
In this session, the patient came up with NT/NB USG and a report of NIPT. The NT/NB scan showed normal findings with the presence of nasal bone, nuchal translucency measuring 1.3 mm, and ductus venosus showed normal forward flow throughout the cardiac cycle. NIPT, with a foetal fraction of 11.7%, showed a low risk for all chromosomal aneuploidies. USG scan and NIPT report were explained to the couple in a detailed manner, which helped in reducing their anxiety levels. During this session, the couple was also explained about the amniocentesis procedure in a detailed manner including risks related to it.
The female opted for prenatal testing through an independent genetic testing laboratory, and as reported by her, the amniotic fluid sampling was done at 17 weeks 4 days of gestation.
Fifth Genetic Counselling Session
The patient came up with the reports of prenatal testing and a Targeted Imaging For Fetal Anomalies (TIIFA) scan. The gestation was 22 weeks 0 days on the day of the fifth genetic counselling session. The prenatal testing reports of the foetus showed normal findings. The chromosomal analysis reports showed no evidence of numerical or structural chromosome rearrangements in any of the cells analysed. The karyotype was suggestive of the foetus with a normal chromosome complement (46,**). The sex of the foetus was not revealed in the report as per PCPNDT Act 1994. The QF-PCR analysis showed no aneuploidy in chromosomes 21, 18, 13 and sex chromosomes. The results were consistent with two copies of chromosome 21,18,13 and two sex chromosomes. To detect mosaicism, deletion and duplication of chromosome 21,18,13, the report of CMA was seen which reported no detection of any significant copy number variation. There were no gains or losses in any region of the genome. The report also confirmed the absence of any microdeletions.
TIFFA scan done at 20 weeks 1 day showed the presence of echogenic intracardiac foci (EIF) in the left ventricle of the foetal heart, which is a soft marker for trisomy 21. Flow across in the ductus venosus and the tricuspid valve was normal. As this was an isolated marker and all diagnostic tests showed the absence of any chromosomal trisomies, the patient was counselled to carry on with the pregnancy after consultation with the concerned gynaecologist. All the findings were explained and discussed with the couple in a detailed manner.
The female delivered a healthy male child at term in the OBG Department and he was kept under observation for the first 72 hours in the Neonatology Department and was observed for all morphological features and conditions related to trisomy 21. He was discharged after 3 days in satisfactory condition.
DISCUSSION
There are three major types of chromosomal abnormalities which can cause DS: trisomy 21, translocations or mosaicism. When complete three copies of chromosome 21 are present, it is known as full trisomy 21. It results mostly due to non-disjunction during maternal meiosis. About 95% of DS cases belong to this category. About 3–4% of DS cases result due to translocations, and only 1–2% of DS cases are due to mosaicism.[7] The silent carriers of RTs between chromosomes 13, 14, 15, or 22 and chromosome 21 are at higher risk of early pregnancy miscarriages, giving birth to a child with DS or a silent carrier of RT.[4]
In the present case, the female was a carrier of an RT between chromosome 14 and 21, so the chances of the foetus being DS were very high as 90% of the DS cases occur due to maternal meiotic errors as first meiotic divisions completely take place in the ovary.[8] The likelihood that the embryo being cytogenetically normal, a silent carrier of RT like the mother, or carrying DS, was 1 in 6 for each of this category. Possibilities of miscarriage in early pregnancy were around 2/6 due to monosomy 14 or 21 and 1/6 due to trisomy 14, as embryos with such cytogenetic makeup are not compatible with life [Table 1].
The decision of a couple to try for pregnancy without any controlled ovarian stimulation (COS) may also go in favour of the couple as COS could increase the chances of chromosomal aneuploidy and mosaicism by influencing the oocyte maturation and the completion of the meiosis cycle.[6]
The female went through reproductive genetic counselling and was put on lifestyle modifications for the good health of her ova. Maternal health plays a significant role in the occurrence of DS. The usage of drugs, alcohol, tobacco or other environmental toxins can induce chromosomal non-disjunction during maternal meiosis, thus increasing the chances of a DS baby.[1]
For this case, to rule out the presence of any chromosomal aneuploidy, structural chromosomal variants or copy number variations in the foetus, prenatal tests including NIPT, quantitative fluorescence polymerase chain reaction (QF-PCR), karyotyping and CMA were used. NIPT from maternal blood provided sensitive and specific screening for trisomies and helped this couple reduce anxiety levels in the early weeks of gestation. QF-PCR helped in confirming the absence of foetal aneuploidies. The nominal and positional information was provided by conventional G-band karyotyping which provides it at a resolution of 5–10 MB. CMA can help in detecting copy number variations to the level ∼ 1kb[9] and be used for the present case to rule out CNVs in the foetus.
An isolated soft marker, EIF, was present in the foetal heart in the TIFFA scan. Isolated soft markers such as EIF, bilateral choroid plexus cyst (CPC) or pyelectasis are non-specific and often correlate with high false-positive rates and can be used to assess individual risks if used in conjunction with other screening or diagnostic tests.[10] As all diagnostic tests for the foetus were showing normal findings, this isolated marker was not given much weightage.
CONCLUSION
Genetic workup, including genetic counselling and testing, should be done for every infertile couple, especially in case of unexplained infertility. Genetic testing could help in identifying silent carriers in the population. Prenatal diagnostics have helped a number of couples fulfil their dream of a genetically healthy baby. The right selection of diagnostic tests at appropriate gestation is the key to avoiding false positives and checking false negatives. Pre-test and post-test genetic counselling sessions are extremely important and necessary for the right selection and interpretation of these tests. Though the silent carriers of structural chromosomal aberrations have low chances of normal pregnancy outcomes, appropriately timed genetic counselling and prenatal genetic testing can help such patients deliver healthy progeny with a less stressful prenatal journey.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
REFERENCES
- Association of Parental Age and the Type of Down Syndrome on the Territory of Bosnia and Herzegovina. Med Arch. 2016;70:88-91.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Down Syndrome in India--Diagnosis, Screening, and Prenatal Diagnosis. Clin Lab Med. 2012;32:231-48.
- [CrossRef] [PubMed] [Google Scholar]
- Down Syndrome - Genetics and Cardiogenetics. Maedica (Bucur). 2017;12:208-13.
- [PubMed] [PubMed Central] [Google Scholar]
- Dermatoglyphics and Reproductive Risk in a Family with Robertsonian Translocation 14q;21q. Acta Inform Med. 2015;23:178-83.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Robertsonian Translocation T (21; 21) in a Female Born to Normal Parents: A Case Report. J Clin Diagn Res. 2015;9:GD01-2.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Mild ovarian stimulation. J Assist Reprod Genet. 2007;24:621-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Cytogenetic and Comorbidity Profile of Down Syndrome in Mansoura University Children’s Hospital, Egypt. Indian J Hum Genet. 2011;17:157-63.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Nondisjunction in Trisomy 21: Origin and Mechanisms. Cytogenet Cell Genet. 2000;91:199-203.
- [CrossRef] [PubMed] [Google Scholar]
- The Prenatal Exome - A Door to Prenatal Diagnostics? Expert Rev Mol Diagn. 2021;21:465-74.
- [CrossRef] [PubMed] [Google Scholar]
- Prenatal Diagnosis of Down Syndrome: A 13-year Retrospective Study. Taiwan J Obstet Gynecol. 2017;56:731-5.
- [CrossRef] [PubMed] [Google Scholar]







