Translate this page into:
Role of calcium inophore in assisted oocyte activation and accelerated capacitation in sperm: A literature review
Address for correspondence: Mr Suryakant Prasad, MSc., CrystaIVF Phule Pune University, Pune, Maharashtra, India. E-mail: suryakantprasad984@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Prasad S, Gupta S. Role of calcium inophore in assisted oocyte activation and accelerated capacitation in sperm: A literature review. Fertil Sci Res 2023;10:78-84.
Abstract
This study aimed to evaluate the use of calcium ionophore during assisted oocyte activation (AOA) and achieve hyperactivation in sperms. The number of intracytoplasmic sperm injection (ICSI) cycles has increased notably as the number of infertile individuals has increased, with average fertilization rates estimated to reach 70%, but fertilization failure still occurs in 1% to 5% of ICSI cycles. ICSI enables male factor infertility to be treated through fertilization. Mammalian sperm become hyperactive after changes in membrane potential due to an increase in intracellular calcium level. This hyperactivation of sperm motility is called capacitation. Sperms with defective cAMP/Protein kinase A (PKA) (low levels of cAMP are sufficient for capacitation and PKA activation) signaling pathways, sluggish motility, or genetic infertility are able to fertilize using calcium ionophore. Protein kinase A regulates sperm motility through the cAMP-dependent phosphorylation of proteins. The failure of standard ICSI to fertilize patients with a sufficient number of oocytes, usually >3%, is primarily due to oocyte activation failure, which may be interrelated with oocyte or sperm factors. Nineteen studies were selected for review based on the selection criteria. Seven out of the 19 included studies showed that AOA with calcium ionophore increased fertilization, blastocyst formation, implantation, clinical pregnancy, and live birth rate during ICSI. In addition, calcium ionophore did not increase the top-quality embryo rate, cleavage rate, miscarriage rate, and congenital birth defects. Studies in past showed sperm become hyperactive with the use of calcium ionophore. This review led us to the conclusion that using calcium ionophore to activate oocytes was beneficial for couples with poor fertilization rates following ICSI.
Keywords
Calcium inophore
capacitation in sperm
failed fertilization
intracytoplasmic sperm injection
oocyte activation
INTRODUCTION
In in-vitro fertilization (IVF) or ICSI resulting in few or no embryos for transfer continues to be a significant clinical challenge during treatment.[1,2,3] The introduction of ICSI significantly improved the clinical outcome for patients with male factor infertility, particularly those with low sperm counts, who could not achieve normal levels of fertilization with conventional IVF. Typical fertilization rates with ICSI average 70% for most patients,[4,5] including those with poor semen parameters or surgically retrieved sperm. A significant proportion of ICSI cycles still results in fertilization rates below 50%, with 3% resulting in total failed fertilization.[16] Although ICSI is invasive, and operator-dependent factors may contribute to the proportion of oocytes not fertilizing normally, most commonly the failure of an oocyte to fertilize after sperm injection is failure of oocyte activation or a failure of sperm activation. In most mammals, the mature ovulated oocyte is arrested in metaphase of the second meiotic division (meiosis II) until fertilization by a sperm. Sperm binding with the oolemma activates the oocyte, triggering a series of pulsatile increases in intracellular calcium concentration, which in turn results in the resumption and completion of meiosis II, extrusion of the second polar body (PB2), and the initiation of preimplantation development. Phospholipase C zeta 1 (PLCz), a sperm-specific phospholipase, is considered the trigger for the molecular pathway within the oocyte, resulting in the release of calcium stores from the endoplasmic reticulum. Recent studies have shown that fertilization failure after ICSI can be linked to sperm devoid of PLCz or sperm with abnormal PLCz function.[6,7,8] It has also been demonstrated that oocyte factors as well as sperm factors are involved in failed fertilization after ICSI. This is even with normal sperm parameters and a good ovarian response. The persistent fertilization failure raises the question of an underlying cause and whether other factors, apart from calcium ionophore being located within the oocyte cytoplasm, may play a role in fertilization.
Sperm and oocyte activation are induced by a variety of chemical agents, such as 6-dimethylaminopurine, strontium chloride, or calcium ionophores.[13] A deficiency in intracellular calcium can be compensated by approaches that aim for an artificial calcium entrance or release.[9,10] A number of studies have been carried out to assess the value of calcium ionophore as a method of sperm and oocyte activation. This study aimed to evaluate the use of calcium ionophore during assisted oocyte activation (AOA) and achieving hyperactivation in sperms.
MATERIALS AND METHODS
An online search was conducted on articles related to use of calcium ionophore in assisted oocyte activation (AOA) and achieving hyperactivation in sperm on PubMed, Google Scholar, ScienceDirect, and the Wiley online library. Search words like calcium ionophore, sperm capacitation, and assisted oocyte activation were used. The studies, which met the following criteria were recruited for analysis:
Inclusion criteria: Studies involving calcium ionophore for oocyte activation and sperm capacitation.
Exclusion criteria: Older studies (>10 years). The current review recruited studies conducted over the past decade to ensure a uniform criterion for calcium ionophore use.
Outcome measures: The studies were evaluated for the number of embryos fertilized, clinical pregnancy rate, miscarriage rates, and congenital birth defects.
RESULTS
Our study initially yielded 1521 articles via the database search. Nineteen articles, including reviews and meta-analysis. Eventually, nine full-text articles were included in our review, consisting of two meta-analyses (Shan et al.,[9]; Murugesu et al.[12]), two prospective studies (Miller et al.[18]; Bonte et al.[16]), four randomized clinical trials (Nikiforaki et al.[13]; Navarrete et al.[17]; Tateno et al.[8]; Karabulut et al.[15]), and one retrospective study (Miller et al.[18]; Table 1). The flowchart of literature identification and selection is summarized in Figure 1.
| Author, year | Study type, period, and country | Number of cases and oocytes | Oocyte activation protocol | Sperm activation protocol | Fertilization rate | Cleavage rate | Implantation rate | Euploidy rate | Pregnancy rate | Live- birth rate | P-value | Limitations |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Antonio Capalbo, 2016 | Prospective cohort study, June 2008 and May 2009, Roam Itali | Fifty-six metaphase II oocytes were donated from 12 patients, did AOA on 49 oocytes | Oocytes were activated by 40 minutes’ exposure to 100 μΜ calcium- ionophore | NA | 76.90% | NA | NA | 59.30% | NA | NA | P= 0.6 | The limited number of oocytes available for activation and restrictions on creating embryos for research purposes in their country of origin prevented analysis of a normally fertilized control group using oocytes from the same donors. |
| Sughashini Murugesu, 2017 | Meta-analysis, n 1998 and 2016, London | Fourteen studies were selected. Where total 5771 oocytes were taken for the AOA | Oocytes were activated by 10-20 minutes’ exposure to 10-30 μΜ calcium- ionophore | NA | 59.20% | 68.30% | 19.90% | NA | 36.90% | 9.10% | Fertilization rate - <0.00001, Cleavage rate - P = 0.06, blastocyst formation. P = 0.003, top embryo quality (planned for transfer) –<0.00001, implantation rate- <0.00001 | The variation in the oocyte activation protocol and timing, as well as the variation in patient selection criteria, which most likely introduced the greatest variability. Also, in some cases, the exact source and method of sperm extraction was not specified. Another issue is that the degree of follow-up varied, with not all embryos being transferred. |
| Dimitra Nikiforaki, 2015 | Randomized clinicaltrials, 2015, Belgium | 37 oocytes were taken for AOA | Oocytes were activated by 10 minutes of exposure to 10 μmol/L calcium- ionophore | NA | 85% | 71% | NA | NA | NA | NA | <0.001 | The differences between species limit our ability to extrapolate the mouse findings to humans, so we additionally used human in vitro matured oocytes next to mouse Mil oocytes to evaluate the two AOA protocols. In vitro matured human oocytes derived from stimulated cycles are used clinically, in cases of limited number of available in vivo matured Mil oocytes, as well as for research purposes, including Ca2J? oscillation pattern analysis |
| Netanella Miller, 2016 | Retrospective cohort Study, 2016, Israel | 83 patients | Oocytes were activated by 10 minutes exposure to 10 μΜ of Ca ionophore | NA | NA | NA | NA | 65% | NA | 12% | FHealthy pregnancy - 0.639, fetal defect - 0.364, first trimesterabortion - 0.465, IUFD - 0.342, chemical pregnancy - 0.463, second trimesterabortion- 1, Ectopic pregnancy - 0.342 | Excluded cases of egg donation and sperm donation, since investigation of these cases is limited, due to lack of full access to the donor's medical background. |
| Seda Karabulut, 2018 | Multicentered randomized clinicaltrials, 2018, istanbul, Turkey | 78 patients | Oocytes were activated by 30 minutes exposure to 30 μΜ of Ca ionophore | NA | 74.10% | NA | NA | NA | 28.60% | NA | Fertilization rate - 0.9, clinical pregnancy. Rate - 1 | Artificial oocyte activation is used mainly for cases with TFF and globozoospermia. Data analyzing the effects of AOA on the outcomes of ICSI procedure for different indications are limited, and these studies focus mostly on testicular sperm and low fertilization cases |
| Davina Bonte, 2019 | Retrospective cohort study, 2019, Ghent, Belgium. | 1743 oocytes were taken for AOA | Oocytes were activated by 10 minutes exposure to 10 μΜ/L of Ca ionophore | NA | 70% | NA | NA | NA | 49% | 41.20% | <0.001 | Because AOA is still an experimental procedure, our findings highlight that Its use should be reserved for a specific subgroup of patients, that is, those with clear oocyte activation deficiencies. |
| Yinghua Shan, 2021 | Meta study, 2021, Yantai, China | 22 full-text articles were included | Oocytes were activated by 10-20 minutes’ exposure to 10-30 μΜ calcium- Ionophore | NA | 62.92% | 93.72% | 56% | NA | 34.87% | 29% | Pregnancy. Rate - 0.0006 | Due to low-quality studies heterogeneity in the Inclusion and evaluation for live birth rate were seen. |
| Felipe A. N avarrete, 2016 | Randomized cllnlcaltrlals, 2016, USA | 20-30 eggs were inseminated with 1 million sperm cells/ mL | NA | Sperms were activated by 10 minutes of exposure to 20 μΜ calcium- ionophore | 87% | NA | NA | NA | NA | NA | NA | Most of the information regarding the role of Ca2+ in hyperactivation has been obtained using loss-of- functlon approaches analyzing sperm motility in media devoid of Ca2+ Ions. Galn-of-functlon experiments using Ca2+ ionophores (e.g., A23187, ionomycin) to increase [Ca2+] have yielded unexpected results because, instead of enhancing hyperactivation, these compounds stopped sperm movement. |
| Hiroyuki Tateno,2013 | Randomized clinicaltrials, 2013, Japan | 70-140 eggs were inseminated with 1-2 million sperm cells/ml | NA | Sperms were activated by 10 minutes of exposure to 20 μΜ calcium- Ionophore | 80% | NA | NA | NA | NA | 71% | NA | Ionophore Induces the acrosome reaction of spermatozoa of a variety of animal species, but it can also Immobilize them. It must have been the excessive amount of Ca2+ entering spermatozoa that rendered them motionless. |
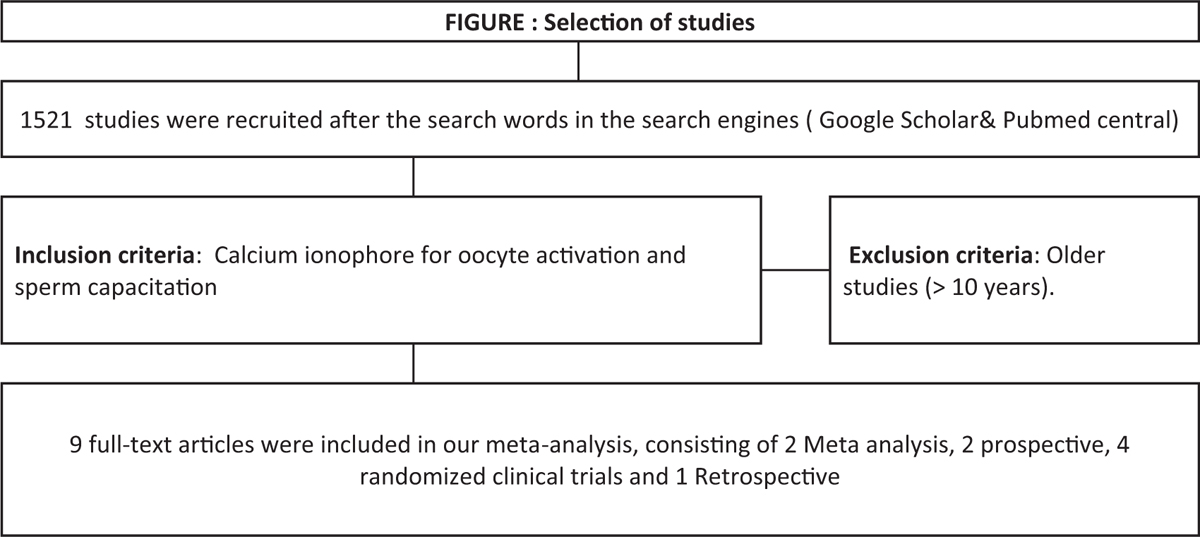
- Selection of studies.
In most of the studies, the oocyte was exposed to 10 μM calcium ionophore dissolved in medium for 10 minutes before ICSI. The oocyte was washed extensively and then exposed 30 minutes later to 10 μM calcium ionophore for 10 minutes again. Finally, it was washed medium and continued for 2 to 3 hours in a medium drop under oil at 37 °C under 6% CO2. Sperms were activated by 10 minutes of exposure to 20 μM calcium-ionophore before doing ICSI.
DISCUSSION
Calcium ionophore treatment for AOA is a common chemical activation method and is always used in cases of low fertilization rates or failed fertilization. Similarly, use of calcium ionophore for achieving hyperactivation in sperms is also used in human sperms. Several studies showed that the use of AOA with calcium ionophore treatment improved pregnancy and the live birth rate to a certain degree. As the number of studies increases, it is necessary to find more reliable evidence of the role of calcium ionophore in improving pregnancy outcomes using both oocytes and sperms. This study was done to explore the efficacy and safety of calcium ionophore treatment in improving pregnancy outcomes and decreasing the incidence of congenital birth defects.
Murugesu et al.[12] studied 14 papers on AOA, where a total 5771 oocytes were taken for the AOA. Where calcium ionophore increased the overall clinical pregnancy rate (per ET; 3.48; 95% confidence interval [CI], 1.65–7.37) and the live birth rate (3.33; 95% CI, 1.50–7.39). This effect of adding calcium ionophore was further demonstrated with fertilization, cleavage, blastocyst, and implantation rates. Subgroup analysis further supported our findings (studies where n > 10 in both arms; random and fixed effects models). The study increases that the effect of calcium ionophore is significantly more pronounced with regards to the overall pregnancy rate.
Antonio et al.,[11] did a sub group analysis on 49 oocytes and the results revealed that most oocytes activated normally. Twenty-seven of these were analyzed, and 16 (59.3%) were euploid, showing no effect of AOA on meiotic segregation. No difference in the proportion of meiosis II[14] type errors was observed between artificially activated oocytes (28.6%; 95% confidence interval 3.7%–71.0%) compared with embryos obtained from normally fertilized oocytes (44.4%; 95% confidence interval 13.7%–78.8%). The abnormally activated oocytes, with >2PN (4 of 39, 10.3%) were diploid, indicating a failure to coordinate the telophase of meiosis II with polar body extrusion.
Miller et al.[18] studied on the basis of a cohort of 595 ICSI pregnancies and 83 ICSI-Ca pregnancies (total number of oocytes taken for AOA not mentioned) theyfound no difference in birth defects rate for singletons or for twins. Additionally, no significant difference was found between defect type (chromosomal aberrations or structural malformations) and malformation type (heart, urogenital, and limb) between the ICSI and ICSI-Ca groups.
Karabulut et al.[15] selected 78 patients (total number of oocytes taken for AOA not mentioned) and Nikiforaki et al.[13] did AOA on 37 oocytes. Shan et al.[9] found fertilization rates and quality of embryos observed in the AOA groups were higher than those of the controls, groups suggesting that not only total fertilization failure patients but also in globozoospermia.
Bonte et al.[16] studied AOA (191 cycles, 1743 oocytes) significantly improved fertilization, pregnancy, and live birth rates in all mouse oocyte activation test (MOAT) groups compared with previous ICSI attempts (243 cycles). Fertilization rates after AOA were significantly different among groups 1 (70.1%), 2 (63.0%), and 3 (57.3%). Depending on the activation rate, patients were classified into MOAT group 1 (20% activation), MOAT group 2 (21–84% activation), or MOAT group 3 (85% activation). Between group 1 and 3, significant differences in pregnancy (49.0% vs. 29.4%) and live birth (41.2% vs. 22.1%) rates were observed. In total, 225 embryo transfers resulted in 60 healthy live births following AOA.
Navarrete et al.[17] used a concentration of 1 million sperm cells/mL on 20 to 30 oocytes and demonstrated that transient incubation of mouse sperm with Ca2+ ionophore accelerated capacitation and rescued fertilizing capacity in sperm with inactivated PKA function. We now show that a pulse of Ca2+ ionophore induces fertilizing capacity in sperm from infertile CatSper1 (Ca2+ channel), Adcy10 (soluble adenylyl cyclase), and Slo3 (K+ channel) KO mice. In contrast, sperm from infertile mice lacking the Ca2+ efflux pump PMACA4 were not rescued. These results indicate that a transient increase in intracellular Ca2+ can overcome genetic infertility in mice and suggest this approach may prove adaptable to rescue sperm function in certain cases of human male infertility. Roles of cAMP were confirmed using KO genetic mouse models lacking either the PKA sperm-specific catalytic splicing variant Cα219, or sAC18. These cycles work the same as humans.
Tateno et al.[8] used a concentration of 1 to 2 million sperm cells/mL on 70 to 140 oocytes. They found that, when spermatozoa were treated with A23187, more than 95% of oocytes were fertilized in the constant presence of the protein kinase A inhibitor, H89. Ionophore-treated spermatozoa also fertilized 80% of oocytes, even in the absence of HCO3−, a component essential for cAMP synthesis under normal in vitro conditions. Under these conditions, fertilized oocytes developed into normal offspring. These data indicate that mouse spermatozoa treated with ionophores are able to fertilize without activation of the cAMP/PKA signaling pathway. Furthermore, they suggest that the cAMP/PKA pathway is upstream of an intracellular Ca2+ increase required for the acrosome reaction and hyperactivation of spermatozoa under normal in vitro conditions.
Limitations
This study analyzed the evidence on the effect of calcium ionophore use as part of fertility treatment, a method of AOA before ICSI, and capacitation of sperm. We have tried to include all studies relating AOA with calcium ionophore in the last 10 years related to our topic. According to our analysis, the use of such treatment leads to an improved range of fertility outcomes. Our conclusions are strengthened by a number of findings. Likely, the effect of calcium ionophore applies at each stage of the fertility process, that is, fertilization, cleavage, blastulation, implantation, and overall pregnancy rate. Limitations included heterogeneity; not all studies were on humans; some included mouse, live birth, and genetic studies were not analyzed in most of the papers. The small data set of our study and operators of ICSI may have different skills were other limitations.
CONCLUSION AND RECOMMENDATIONS
Calcium ionophore treatment on oocytes during ICSI and on sperms for achieving capacitation results in an improvement in fertilization rate. Though overall blastulation, implantation, pregnancy rate, and live-birth rates have yet to be proven statistically significant. It can be recommended for couples where ICSI alone yields poor fertilization rates. This analysis may have clinical application in patients with repeated fertilization failures in ICSI. However, larger randomized clinical trials are needed to recommend its standard use.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- National, regional, and global trends in infertility prevalence since 1990: a systematic analysis of 277 health surveys. PLoS Med. 2012;9:e1001356.
- [CrossRef] [PubMed] [Google Scholar]
- Human Fertilisation and Embryology Authority: Fertility treatment in 2012: trends and figures. Available at: http://www.hfea.gov.uk/docs/FertilityTreatment2012TrendsFigures.PDF (accessed )
- [Google Scholar]
- Factors associated with failed treatment: an analysis of 121,744 women embarking on their first IVF cycles. PLoS One. 2013;8:e82249.
- [CrossRef] [PubMed] [Google Scholar]
- Understanding fertilization through intracytoplasmic sperm injection (ICSI) Cell Calcium. 2014;55:24-37.
- [CrossRef] [PubMed] [Google Scholar]
- Assisted reproductive technology in Europe, 2010: results generated from European registers by ESHRE. Hum Reprod. 2014;29:2099-113.
- [Google Scholar]
- Phospholipase Cz rescues failed oocyte activation in a prototype of male factor infertility. Fertil Steril. 2013;99:76-85.
- [CrossRef] [PubMed] [Google Scholar]
- Phospholipase C zeta (PLCz): oocyte activation and clinical links to male factor infertility. Adv Biol Regul. 2013;53:292-308.
- [CrossRef] [PubMed] [Google Scholar]
- Ca2+ ionophore A23187 can make mouse spermatozoa capable of fertilizing in vitro without activation of cAMP-dependent phosphorylation pathways. Proc Natl Acad Sci USA. 2013;110:18543-8. doi: 10.1073/pnas.1317113110
- [CrossRef] [PubMed] [Google Scholar]
- Assisted oocyte activation with calcium ionophore improves pregnancy outcomes and offspring safety in infertile patients: a systematic review and meta-analysis. Front Physiol. 2022;12:751905. doi: 10.3389/fphys.2021.751905
- [CrossRef] [PubMed] [Google Scholar]
- Assisted oocyte activation following ICSI fertilization failure. Reprod Biomed Online. 2014;28:560-71.
- [CrossRef] [PubMed] [Google Scholar]
- Artificial oocyte activation with calcium ionophore does not cause a widespread increase in chromosome segregation errors in the second meiotic division of the oocyte. Fertil Steril. 2016;105:807-14.
- [CrossRef] [PubMed] [Google Scholar]
- Does the use of calcium ionophore during artificial oocyte activation demonstrate an effect on pregnancy rate? A meta-analysis. Fertil Steril. 2017;108:468-82.e3.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of two assisted oocyte activation protocols used to overcome fertilization failure on the activation potential and calcium releasing pattern. Fertil Steril. 2016;105:798-806.e2. doi: 10.1016/j.fertnstert.2015.11.00
- [CrossRef] [PubMed] [Google Scholar]
- Artificial oocyte activation: evidence for clinical readiness. Reprod Biomed Online. 2016;32(3):271-3.
- [CrossRef] [PubMed] [Google Scholar]
- Artificial oocyte activation with calcium ionophore for frozen sperm cycles. Syst Biol Reprod Med. 2018;64:381-8. doi: 10.1080/19396368.2018.1452311
- [CrossRef] [PubMed] [Google Scholar]
- Assisted oocyte activation significantly increases fertilization and pregnancy outcome in patients with low and total failed fertilization after intracytoplasmic sperm injection: a 17-year retrospective study. Fertil Steril. ;112:266-74. doi: 10.1016/j.fertnstert.2019.04.006
- [CrossRef] [PubMed] [Google Scholar]
- Transient exposure to calcium ionophore enables in vitro fertilization in sterile mouse models. Sci Rep. 2016;6:33589. doi: 10.1038/srep33589
- [CrossRef] [PubMed] [Google Scholar]
- Oocyte activation by calcium ionophore and congenital birth defects: a retrospective cohort study. Fertil Steril. 2016;106:590-596.e2.
- [CrossRef] [PubMed] [Google Scholar]







